There’s a pretty standard hierarchy in medicine:
Medical Student → Junior Resident → Senior Resident → +/- Fellow → Attending
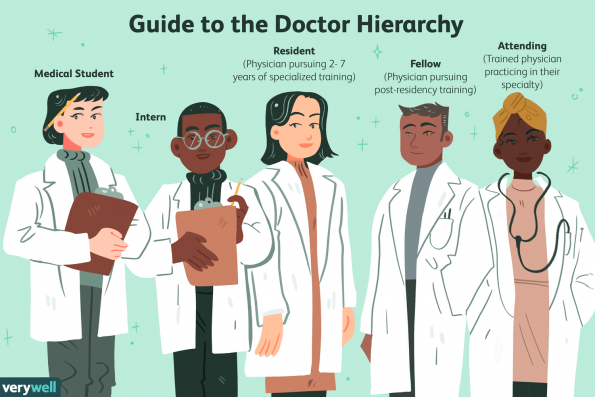
Very Well/Emily Roberts
Similar to many things in medicine, this hierarchy stems from old habits and practices. In the ninetieth century, medical apprentices were legally bound to their surgeon (master) for 7 years – working as a servant in exchange for the acquisition of skills. This ‘apprenticeship model’ has not really changed, although we’ve deviated from calling attending physicians ‘masters’ (1).
The Hierarchy
The hierarchy exists because medicine is a numbers game. The idea being, if you do x number of assessments, procedures, or surgeries – that you will become proficient in that skill. This is why trainees are encouraged to maintain a low threshold to gain exposure and experience. There is only so much learning that occurs in a textbook – medicine is about the nuances. Now, this approach makes sense educationally. But at some point (and I’d argue that this now occurs too frequently) this hierarchy is no longer educational. Instead – it loses its educational potential and has the potential for significant patient harms (now also remember, trainees are in the hospital to learn).
As an Emergency Physician I have the luxury of working on the frontlines, alongside most of the hospital’s residents. I see them at all hours of the day, evenings and weekends. I have a first hand look at their workload, how sick their patients are, when they need help, and when they’re having a good night. Emergency Physicians are uniquely positioned where we see how consulting services flow – we could provide some very high yield feedback on how the radiology resident did with flow overnight, or how the medicine senior triaged consults.

Down in the ED, we see everything. So we also see when residents/services need help. Not because they’re incapable, but because patients are sicker, and hospitals are busier than ever before – with overcrowding being a daily occurrence. Everyone in medicine has days or moments where they are overwhelmed by the task list in front of them, but it becomes especially problematic when the vast majority of your days in training are spent feeling overwhelmed because of circumstances external to one’s control.
The hierarchy system of medicine is one of the most inefficient ways to approach a problem. Lets say an Emergency Physician has diagnosed a patient with appendicitis at 0900; the medical student comes down to do a consult, and hour later, they review with a junior, maybe the senior resident. They decide to admit the patient and schedule surgery. We should also mention that there are 4 patients in the ED with appendicitis, 2 with cholecystitis, and 2 post-operative complications in the ED, plus 3 sick post-operative patients on the ward, plus all the regular regular patients that need to be seen. Plus… a full day of operating. The amazing thing is – the trainees will get the work done.
But… should they?
Medicine is different from twenty years ago. patients are sicker, acuity is higher, they have far more comorbidities and complexity (i.e.: the patient has a UTI, but has also had a recent renal transplant), and the increasing geriatrics population provides unique challenges in care. Adding to this is unprecedented levels of overcrowding. The hierarchy may have had some merit, when patient volumes were lower, crowding was less, paperwork was minimal and patient complexity/aging populations were lower. But step one foot in any Emergency Department and you’ll see a busy, chaotic environment with an endless sea of patients. There is also evidence that has demonstrated the hierarchy approach can lead to direct patient harms.
When your cognitive load is high, you will under-perform at tasks. This is worsened by fatigue (i.e.: prolonged hours on call). So when the medicine senior resident has 8 consults pending, 2 consults that they need to review, and an Emergency Department with an influx of sick patients – their cognitive load has the potential to result in patient harm. Just because the medicine resident can accomplish these tasks, doesn’t mean that they should. Because, as a healthcare system – our priority is to the patient, and in this model – the patient suffers.
Residents have a very prominent role in running the hospital, ensuring that patient’s have their daily medical care needs met in conjunction with our allied health professionals, they help facilitate admissions, discharges and direct patient care. They do this, because it is this experience and training that will help them develop the toolbox they need to become a proficient staff physician. Then there is the historical ideology of; “well, I put in the work, so you have to as well.”
But, there hits a point where the experience is no longer educational, but harmful to that learner. When there is an unmanageable cognitive load – the trainee stops learning. The experience begins to lack educational value – and instead, they may pick up bad habits, or it can sour their disposition towards medicine. I’d argue that point of diminishing returns is happening on a more frequent basis with our trainees because of how busy hospitals have become.
So the naive observer may ask – why not just ask for help? Why doesn’t the resident call for back up?
Well..
Medical Student → Junior Resident → Senior Resident → +/- Fellow → Attending
That’s how it’s done in medicine, the resident struggles – but isn’t “supposed” to reach out for help, because historically – it would be a sign of weakness in a sociologic power dynamic.
So instead, the resident works – and patient’s wait. .. and wait… and wait.
I will apply dietetic measures for the benefit of the sick according to my ability and judgment; I will keep them from harm and injustice.
– Hippocratic Oath
The reluctance to ask staff for help is borne out of a fear that is naturally created by medicine’s power dynamic. But, to be honest – they shouldn’t have to ask for help. There needs to be a medical cultural change that makes it implicit the hierarchal establishment should come help out when things are busy. The amount of time it will take a staff cardiologist to disposition a patient, can help offload a significant volume of work. It needs to become normal in the culture of medicine that staff and fellows help their learners on the frontlines and in the trenches, because the volume, acuity and complexity of patients is continuing to trend up. Not to mention, the added complexity of training during a global pandemic.
We challenge senior residents in the ED to ‘run a section’ of the department – but when it hits a critical number of patients (when the bus arrives), we’ll step in to help. Not because the resident can’t handle it – but because they shouldn’t. At some point, the cognitive load no longer becomes educational, and patient’s suffer as a result.
Team Dynamics
So, if we should scrap the medical hierarchy, what is the solution? The wheel has already been created on this one – and it is through a team-based approach. Now, conventionally, when we think about teams in medicine, we think about allied health teams or inter-disciplinary work. Within our healthcare teams, there are sub-teams that encompass the conventional medical hierarchy from student to staff physician.
Five Dynamics of Effective Teams
In 2015, Julia Rozovsky started Project Aristotle at Google – with the intent of addressing the question of what makes teams effective. They came up with 5 key domains that have relevant applications to how medical teams function:
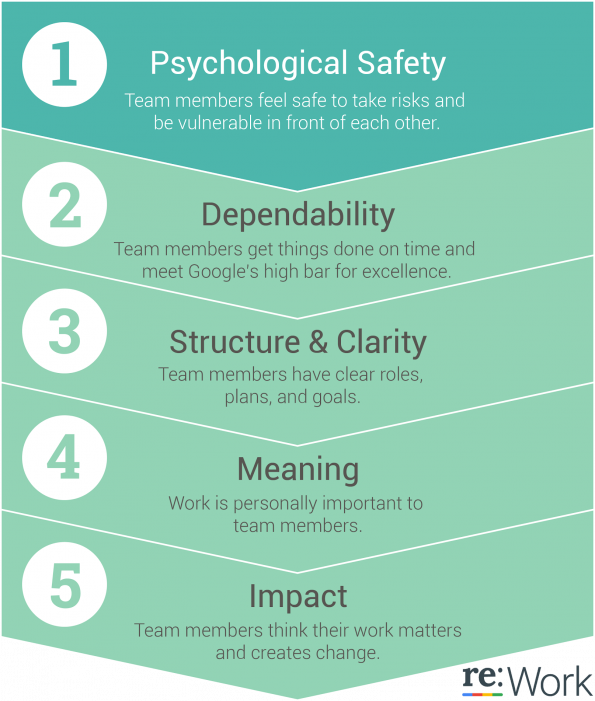
- Psychological Safety: This was felt to be the most important dynamic in an effective team. When one doesn’t feel psychologically safe, they worry about speaking up, answering questions, or questioning potentially unsafe medical practices for fear of being viewed as incompetent or disruptive. Psychological safety allows for open discussions around patient care, and can enhance the patient experience by creating an environment where people feel they can express thoughts related to patient care. In much of medicine there is no singular ‘right way’ to do things – so this can enhance patient care by allowing the sharing of ideas in order to ‘group think’ best practices. This is challenging to overcome because of the (unavoidable) power dynamic amongst the various ‘ranks’ in medicine, but ensuring trainees feel psychologically safe will enhance team rapport (CanMEDS: communicator) and facilitate better learning and patient care.
- Dependability: Members of a team were reliable to get tasks done effectively and on time – when it comes to medicine, this one is a no-brainer. It does not, however, preclude asking for help.
- Structure and Clarity: A team needs to have clear roles and responsibilities. Every individual on the team needs to understand what is expected of them, and what the current objectives are – whether that is stabilizing someone prior to surgery, or arranging discharges, goals need to be specified on an individual and group level.
- Meaning: Finding purpose in work is important for team effectiveness. This is where it is key to remember that trainees are in the hospital to gain educational experience and knowledge, so as teachers – it is our job to teach. I talked to a resident who recently changed specialities, and remarked that he had “found the fun” in medicine again – one’s job needs to be rewarding and provide meaning.
- Impact: The most effective teams are often based on how one’s work contributes to the team’s goals and what their influence has been.
When we think about how we are going to ‘run our teams’ (or; department, OR, ER, birthing unit, etc), keeping these principles in mind will help us better educate our trainees and provide better patient care. The hierarchy of medicine needs to be re-considered, and we should devote our efforts to approaching each of our environments with a team based approach. What that means at any given point in time is going to vary based on your situational awareness. The service is busy? Maybe that is a good time for the staff member to prioritize discharges, or reviewing consults. Quiet day? Perhaps it is didactic teaching after letting the senior learner run the team. Part of team dynamics is that they need to be flexible, based on situational awareness.
Knowing what your learners needs are is a sign of a master teacher, while still maintaining the needs of the patient is the sign of a masterful physician.
The last thing I will say is that if you’re a resident in a hospital at night, and you need an opinion or a hand? Go find the Emergency physician on. Chances are, we’ll have some ideas – and we’re (almost) all happy to help. There is always, a staff physician around, somewhere.


Very thoughtful.
Some interesting perspectives. What is often omitted in discourse such as this is the opportunity cost of the more senior doctors providing these additional activities. In order for them to do this something else has to give as those colleagues also have other important activities which are essential for patient care