Pulling back the Pall from palliative care
The word pall refers to a traditional death shroud or a dark cloud of dust or smoke. The aim of this blog post is both explore some of the inequities and recommendations for the palliative care landscape today, but also to remove the connotation of palliative care being a death sentence; it is about symptom control and facilitating a comfortable transition to end of life.
There are many approaches to Palliative care (PC) and End of Life care (EOL) in the emergency department (ED), and a wide spectrum of involvement of the Emergency Physician (EP) in initiating such care. Anecdotally, the EP’s role in the initiation of EOL care is often prevalent in the following scenarios:
-
- Unsalvageable presentations in a patient with baseline diminished protoplasm (i.e., very advanced age or carrying the label of “terminal illness”);
- Acute illness refractory to all interventions proffered by standard or modified ACLS approaches;
- Identification of those that are likely to die imminently, regardless of what that EP or consulting services have in their armamentarium.
With an increasingly aging population, palliative and end of life care are a core component of providing patient-centred care. The question then becomes – can we as ED physicians do more than the scenarios above? By earlier identification of patients who might benefit from PC services through appropriate EM education, we could:
-
- Reduce the amount of ED visits;
- Provide a better quality of life for patients to live their end of days in an environment of their choice.
In this 2-part series, we will delve into the subject further by exploring the following topics:
-
- Access to Palliative Care and its Inequities
- Screening Tools: The Old and the New (Part 2)
- Education and Integration of PC into EM (Part 2)
Access to Palliative Care and its Inequities
It is no surprise that patients with malignancies account for the largest part of palliative care resource allocation in Canada. Cancers are automatically deemed “terminal”, thus allowing for early initiation of resources. Comparatively, diseases ranked second (Heart Diseases), third (Cerebrovascular Diseases) and fourth (Lower Respiratory Disease) – highest for morbidity and mortality in Canada, often do not receive the “terminal” label1. It’s important to note that it’s not the amount of time left on the clock but the amount of suffering over time.
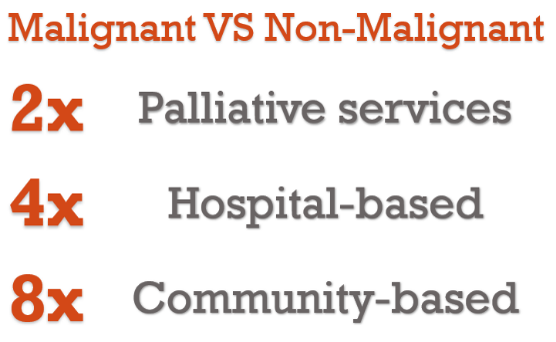
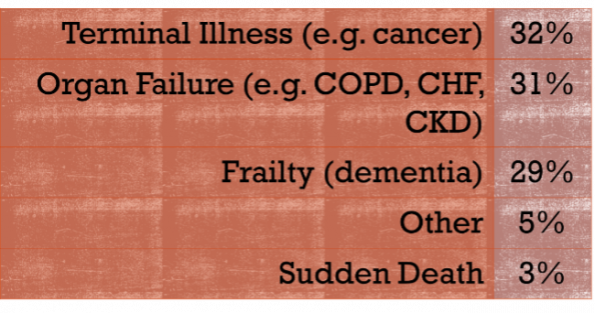 A 2017 population-based study conducted by Seow et al, among 235k Ontario decedents, identified terminal illness (e.g., cancer), organ failure (e.g. COPD, CHF, and CKD), and frailty (e.g. advanced dementia) patients in nearly equal proportions (see table).2 However, 88% of patients diagnosed with cancer received palliative care services, compared to 44% and 32% for organ failure and frailty, respectively. Furthermore, patients with cancer received four times more hospital-based and eight times more community-based PC days.
A 2017 population-based study conducted by Seow et al, among 235k Ontario decedents, identified terminal illness (e.g., cancer), organ failure (e.g. COPD, CHF, and CKD), and frailty (e.g. advanced dementia) patients in nearly equal proportions (see table).2 However, 88% of patients diagnosed with cancer received palliative care services, compared to 44% and 32% for organ failure and frailty, respectively. Furthermore, patients with cancer received four times more hospital-based and eight times more community-based PC days.
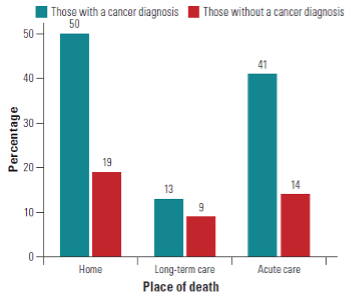
Percentage of individuals receiving care, based on place of death.In 2019, the CIHI assembled provincial data across Canada and showed similar results; patients with cancer diagnoses are three times as likely to receive PC as those with other diseases.3
This is problematic, as the symptom burden suffered by patients with malignancy and those with end-stage organ failure are relatively comparable. A paper by Edmonds compared the incidence of symptoms of chronic lung diseases (ICD codes 491-502) and lung cancer (ICD code 162) and found that those with chronic lung disease experienced breathlessness 16% more frequently than those with lung cancer. In addition, the rate at which both categories of these patients experienced pain, vomiting, insomnia, confusion, and low mood was nearly equal. See et al compared symptoms of patients with malignant vs non-malignant diagnoses admitted to a palliative care unit. They showed that those in the malignant group reported far greater pain scores, while there was no significant difference in dyspnea, nausea, insomnia, or bowel symptoms.
 I’m sure, at this point, you have recognized a pattern – despite similar symptomatology between chronic diseases and cancers, those with chronic diseases receive limited end-of-life services. There is a clear discrepancy that suggests that patients with end-stage organ failure and those with advanced dementia may not get the resources they need, despite mounting evidence, that palliative care has positive outcomes on quality of life.
I’m sure, at this point, you have recognized a pattern – despite similar symptomatology between chronic diseases and cancers, those with chronic diseases receive limited end-of-life services. There is a clear discrepancy that suggests that patients with end-stage organ failure and those with advanced dementia may not get the resources they need, despite mounting evidence, that palliative care has positive outcomes on quality of life.
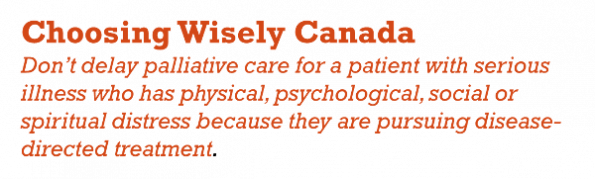
The World Health Organization (WHO) has made a statement on the role of PC, emphasizing the improvement of quality of life and prevention of suffering.4 Furthermore, Choosing Wisely Canada (CWC) recommends early initiation of PC for any individual with serious illness, regardless of aetiology or stage of treatment.5 I encourage readers to consider the above on their next shift, become acquainted with your referral process, and consider referring appropriate individuals to palliative services early in the process.
Palliative Care Involvement = Fewer ED Visits
Further to improving patient quality of life, early PC involvement has a direct impact on decreasing fewer visits to the ED and ICU admissions. In the previously mentioned CIHI study, palliative care involvement greater than 30 days prior to the end of life showed:
-
- 6% decrease in patients requiring 2 or more ED visits.3
- 19% decrease in ICU admissions compared to those with no palliative involvement.3
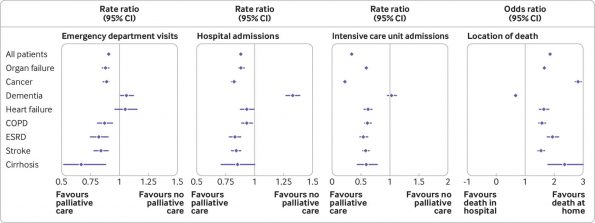
Quinn et al reported similar findings in 2020, showing that PC involvement was associated with:
-
- 12% reduction in ED visits and hospital admissions.
- 41% decrease in ICU admissions, except for patients dying from dementia who were found to use the ED and require hospital admission more often.
The dementia outlier is thought to be due to the perspective of the substitute decision-maker possibly not recognizing dementia as terminal, or that reasons for ED visits or hospital admission aren’t related to dementia.6
Take-Home Points
-
- Patients with organ failure and dementia are underserved by Palliative Care services at end-of-life;
- The extent of symptom burden of malignant and non-malignant disease at end-of-life is similar;
- Palliative care involvement = Fewer visits to the ED and fewer admissions to the ICU.
Now that we have identified the above, stay tuned for part 2 of this blog series, where we will explore identification of patients that would benefit from PC resources, in addition to how to beset integrate PC into the Emergency Department.
References
1. Statistics Canada. Leading causes of death, total population, by age group. Published November 26, 2020. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039401
2. Seow H, O’Leary E, Perez R, Tanuseputro P. Access to palliative care by disease trajectory: a population-based cohort of Ontario decedents. BMJ Open. 2018;8(4):e021147. doi:10.1136/bmjopen-2017-021147
3. Alicia Costante CL and CC. Access to Palliative Care in Canada. Healthc Q. 2019;21(4):10-12.
4. World Health Organization. Palliative Care. Published August 5, 2020. https://www.who.int/news-room/fact-sheets/detail/palliative-care
5. Canadian Society of Palliative Care Physicians. Palliative Care – Five Things Physicians and Patients Should Question. Choosing Wisely Canada. https://choosingwiselycanada.org/palliative-care/
6. Quinn KL, Stukel T, Stall NM, et al. Association between palliative care and healthcare outcomes among adults with terminal non-cancer illness: population based matched cohort study. BMJ. 2020;370:m2257. doi:10.1136/bmj.m2257
7. Downar J, Goldman R, Pinto R, Englesakis M, Adhikari NKJ. The “surprise question” for predicting death in seriously ill patients: a systematic review and meta-analysis. Can Med Assoc J. 2017;189(13):E484. doi:10.1503/cmaj.160775
8. Ermers DJ, Kuip EJ, Veldhoven C, et al. Timely identification of patients in need of palliative care using the Double Surprise Question: A prospective study on outpatients with cancer. Palliat Med. 2021;35(3):592-602. doi:10.1177/0269216320986720
9. Bowman J, George N, Barrett N, Anderson K, Dove-Maguire K, Baird J. Acceptability and Reliability of a Novel Palliative Care Screening Tool Among Emergency Department Providers. Acad Emerg Med. 2016;23(6):694-702. doi:10.1111/acem.12963
10. Tan A, Durbin M, Chung FR, et al. Design and implementation of a clinical decision support tool for primary palliative Care for Emergency Medicine (PRIM-ER). BMC Med Inform Decis Mak. 2020;20(1):13. doi:10.1186/s12911-020-1021-7
11. Baylis J, Harris DR, Chen C, et al. Palliative and end-of-life care education in Canadian emergency medicine residency programs: A national cross-sectional survey. CJEM. 2019;21(2):219-225. doi:10.1017/cem.2018.470
12. Grudzen CR, Brody AA, Chung FR, et al. Primary Palliative Care for Emergency Medicine (PRIM-ER): Protocol for a Pragmatic, Cluster-Randomised, Stepped Wedge Design to Test the Effectiveness of Primary Palliative Care Education, Training and Technical Support for Emergency Medicine. BMJ Open. 2019;9(7):e030099. doi:10.1136/bmjopen-2019-030099
13. Chung FR, Turecamo S, Cuthel AM, et al. Effectiveness and Reach of the Primary Palliative Care for Emergency Medicine (PRIM-ER) Pilot Study: a Qualitative Analysis. J Gen Intern Med. 2021;36(2):296-304. doi:10.1007/s11606-020-06302-2
14. Carter AJE, Arab M, Cameron C, et al. A national collaborative to spread and scale paramedics providing palliative care in Canada: Breaking down silos is essential to success. Prog Palliat Care. 2021;29(2):59-65. doi:10.1080/09699260.2020.1871173