Ischemic stroke and Transient Ischemic Attack have been a vigorously studied subject, particularly in the past few years. With numerous updates and recommendations, we will provide an updated guide for Emergency Physicians in regards to ischemic stroke and TIA management and workup.
Endovascular therapy for Ischemic Stroke:
- In 2013, three high quality studies published in NEJM failed to show a benefit for endovascular therapy, compared to standard treatment [1-3].
- Within two years, however, there was a significant paradigm shift to alter this theory, based on five high quality studies published in NEJM, showing a benefit for endovascular therapy in ischemic stroke [4-8].
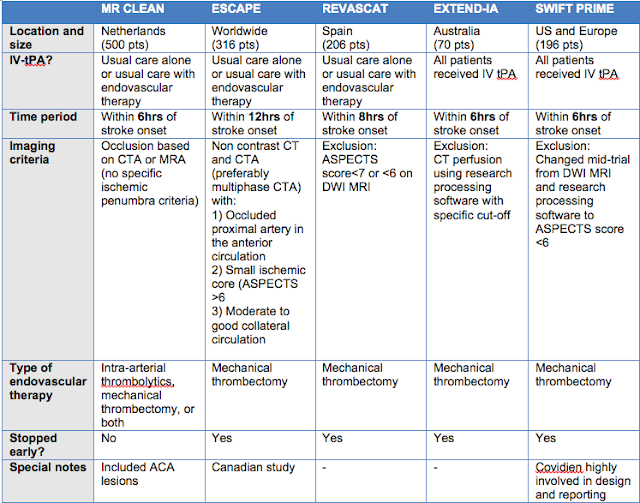
- The newer studies had some fundamental differences in comparison to the earlier negative trials [9]:
- Strict patient selection: Most studies used stroke onset < 6 hours, with the ESCAPE trial having the longest inclusion time with stroke onset <12 hours [4].
- Improved imaging selection: Demonstration of a large proximal clot in the anterior circulation with an salvageable ischemic penumbra [10,11].
- New Technologies: Development of mechanical thrombectomy with new generation retrievable stents instead of intra-arterial tPA.
Each of these 2015 studies were fairly similar, aside from a few important differences:
- The primary outcome of each study was Modified Rankin Score at 90 days, and all studies demonstrated that the endovascular therapy group was associated with functional independence (mRS of 0-2) at 90 days compared to standard therapy [12].
- NNT from all of these positive studies ranged from 4-8.
- The ESCAPE trial additionally demonstrated an mortality benefit at 90 days, with an NNT of 11 [4].
- Across all studies there was no statistical difference in events of symptomatic intracranial hemorrhage at 90 days.
- Of note, although the ESCAPE trial randomized patients up to 12 hours after stroke onset, only a small number of patients were actually randomized after 6 hours, and the results were not statistically significant (although, the direction of effect favoured endovascular therapy) [4].
- All of the trials were stopped early, with the exception of MR CLEAN (as that was the first trial released, demonstrating the initial benefit of endovascular therapy).
Limitations and future directions:
- Endovascular therapy has been demonstrated to have a clear benefit in a SPECIFIC patient population.
- Benefit has not yet been demonstrated in an expanded patient population.
- Smaller occlusions more amenable to IV tPA, and larger occlusions more amenable to thrombectomy.
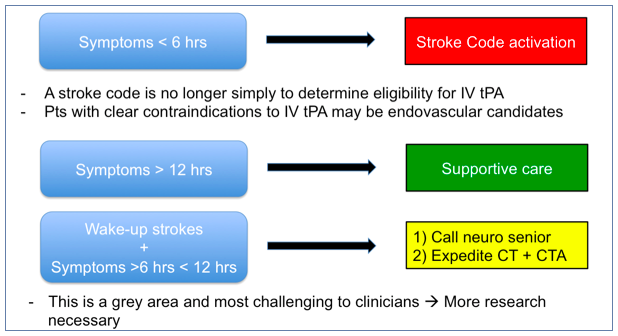
- Upper time limit for this benefit is still unknown
- Most studies used <6 hours from stroke onset as their inclusion
- ESCAPE randomized patients up to 12 hours, but those included after 6 hours did not yield an statistical benefit.
- Future directions will likely include a shift from “last time seen well” towards “imaging completed” to determine the time course for intervention.
Bottom lines:
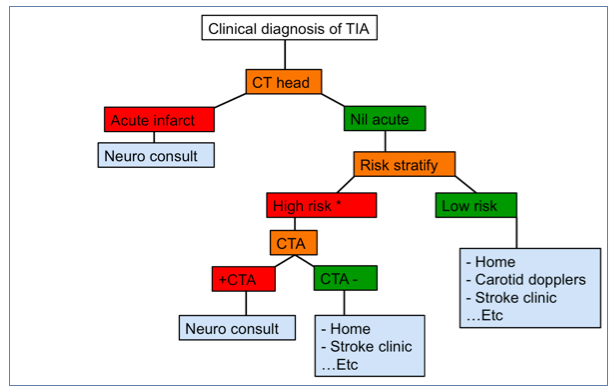
Imaging in TIA
- It is well known that the risk of stroke is highest immediately following an TIA, and that intervening at this point can improve long term outcomes [13-16].
- Classically, clinical prediction scores such as ABCD2 have been used for risk stratification but have not performed well [17].
What about imaging findings contributing to risk evaluation?
CT Head:
- A study published in Stroke last year investigated the link between imaging findings of acute ischemia on non-contrast CT head in patients presenting with TIA, and subsequent risk of recurrent stroke [18].
- The study included over 2000 TIA patients presenting to Canadian ED’s, and assessed the head CT for acute/chronic ischemia or microangiopathy, with stroke at 90 days representing their primary outcome.
- The authors found that as the “ischemic load” increased, the risk of recurrent stroke increased as well (OR of 3-8), with a large part of that risk occurring in the first 48 hours after presentation.
- This suggests that ischemic changes on a non-contrast CT head greatly increase the risk of subsequent stroke in TIA patients.
Vascular imaging:
- Historically, vascular imaging in the setting of TIA was mainly used to evaluate for carotid stenosis, following the NASCET study in 1998, which demonstrated an large benefit for carotid endarterectomy in symptomatic carotid stenosis ≥ 50% [19].
- With increasing availability of CT-A (especially after hours), this became another viable alternative to carotid dopplers, with the caveat that this will increase visualization of potentially asymptomatic lesions.
- To better help determine which patients would benefit from vascular imaging, the CATCH study published in Stroke in 2012 demonstrated that CT-A findings could predict recurrent stroke in TIA and minor stroke patients [20].
- Patients presenting with high risk TIA features (focal weakness or speech disturbance) or minor ischemic stroke (NIHSS <3) underwent CT and CT-A, and were followed to 90 days to determine of recurrent stroke occurred.
- CT/CT-A was considered positive if any of the following were seen:
- Acute ischemic change seen on CT.
- Intracranial or extracranial vessel occlusion
- Stenosis ≥ 50% ipsilateral to the clinically relevant ischemic brain tissue.
- The study found that abnormal CT/CT-A imaging had a significantly higher risk of recurrent stroke. Of note, intracranial stenosis or occlusion was identified to be as high risk as extracranial stenosis or occlusion.
Bottom Line:
- Higher risk patients should receive an CT-A prior to leaving the Emergency Department.
- High risk patients are those with a) motor symptoms, or b) speech symptoms
- Patients presenting with TIA require an neurology consultation in the department if they have one of the following features:
- Acute stroke on CT Head
- Free floating thrombus
- Carotid artery stenosis ≥ 50% (in conjunction with vascular surgery).
- Of note: these indications for neurology referral are predicated by imaging findings, rather than clinical findings.
References
- Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R. Endovascular Treatment for Acute Ischemic Stroke. New. 2013;268:904-913. doi:10.1056/NEJMoa1213701
- Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923. doi:10.1056/NEJMoa1212793
- Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893-903. doi:10.1056/NEJMoa1214300
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030. doi:10.1056/NEJMoa1414905
- Campbell BCV, Mitchell PJ, Kleinig TJ, et al. Endovascular Therapy for Ischemic Stroke with Perfusion-Imaging Selection. N Engl J Med. 2015;372(11):1009-1018
- Berkhemer O, Fransen P, Beumer D, et al. A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke. New Engl J Med. 2014;372(1):11-20. doi:10.1056/NEJMoa1411587
- Saver JL, Goyal M, Bonafe A, et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N Engl J Med. 2015;372(24):2285-2295. doi:10.1056/NEJMoa1415061
- Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 Hours after Symptom Onset in Ischemic Stroke. N Engl J Med. 2015;372(24):1-11. doi:10.1056/NEJMoa1503780
- Furlan AJ. edi t or i a l s Endovascular Therapy for Stroke — It ’ s about Time. 2015:2347-2349.
- Pexman JHW, Barber PA, Hill MD, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. Am J Neuroradiol. 2001;22(8):1534-1542
- Menon BK, D’Esterre CD, Qazi E, et al. Multi-phase CTA: A new tool for the imaging triage of patients with acute ischemic stroke. Int J Stroke. 2015;10(2):307-308
- Badhiwala JH, Nassiri F, Alhazzani W, et al. Endovascular Thrombectomy for Acute Ischemic Stroke. Jama. 2015;314(17):1832. doi:10.1001/jama.2015.13767
- othwell PM, Warlow CP. Timing of TIAs preceding stroke: time window for prevention is very short. Neurology. 2005;64(5):817-820. doi:10.1212/01.WNL.0000152985.32732.EE
- Lisabeth LD, Ireland JK, Risser JMH, et al. Stroke risk after transient ischemic attack in a population-based setting. Stroke. 2004;35(8):1842-1846. doi:10.1161/01.STR.0000134416.89389.9d
- Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007;370(9596):1432-1442. doi:10.1016/S0140-6736(07)61448-2
- Lavallée PC, Meseguer E, Abboud H, et al. A transient ischaemic attack clinic with round-the-clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953-960. doi:10.1016/S1474-4422(07)70248-X.
- Kamal N, Hill MD, Blacquiere DPV, et al. Rapid Assessment and Treatment of Transient Ischemic Attacks and Minor Stroke in Canadian Emergency Departments: Figure. Stroke. 2015;46(10):2987-2990. doi:10.1161/STROKEAHA.115.010454
- Wasserman JK, Perry JJ, Sivilotti ML a, et al. Computed Tomography Identifies Patients at High Risk for Stroke After Transient Ischemic Attack/Nondisabling Stroke: Prospective, Multicenter Cohort Study. Stroke. 2014:1-7. doi:10.1161/STROKEAHA.114.006768
- Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. N. 1998:1415-1425
- Coutts SB, Modi J, Patel SK, Demchuk AM, Goyal M, Hill MD. CT/CT angiography and MRI findings predict recurrent stroke after transient ischemic attack and minor stroke: Results of the prospective CATCH study. Stroke. 2012;43(4):1013-1017. doi:10.1161/STROKEAHA.111.637421