You’re on shift and a patient presents with pelvic pain. You suspect the ovaries may be involved, but the transvaginal probe isn’t available. Don’t worry — your transabdominal PoCUS skills can still get the job done.
This month’s PoCUS Pearl covers:
1️⃣ How to confidently identify ovaries using a transabdominal approach
2️⃣ How to recognize common ovarian pathologies and their management
Why bother scanning the ovaries?
Serious ovarian pathology is rare in the ED — but recognition matters.
-
Ovarian torsion occurs in about 0.16 % of ED visits among reproductive-aged women.
-
Life-threatening ovarian pathologies such as hemorrhagic cysts or tubo-ovarian abscesses have a < 0.5 % prevalence in gynecologic ED visits.
-
Torsion can lead to loss of ovarian function and infertility if diagnosis is delayed.
-
Ruptured cysts usually resolve but ~15 % require surgery for hemoperitoneum or instability.
-
Ovarian cancer is often diagnosed through emergency presentations, carrying much higher mortality.
Even uncommon pathologies deserve attention — timely identification can be life-changing.
Why PoCUS?
Even when a CT or radiology-performed ultrasound is ordered, early bedside PoCUS helps you:
✅ Reduce diagnostic uncertainty and decision fatigue
✅ Initiate empiric management earlier
✅ Consult OBGYN sooner
✅ Guide interventions in real time
Technique: Identifying the ovaries
Probe: Curvilinear Preset: Pelvic / Abdomen Position: Supine, bladder moderately full
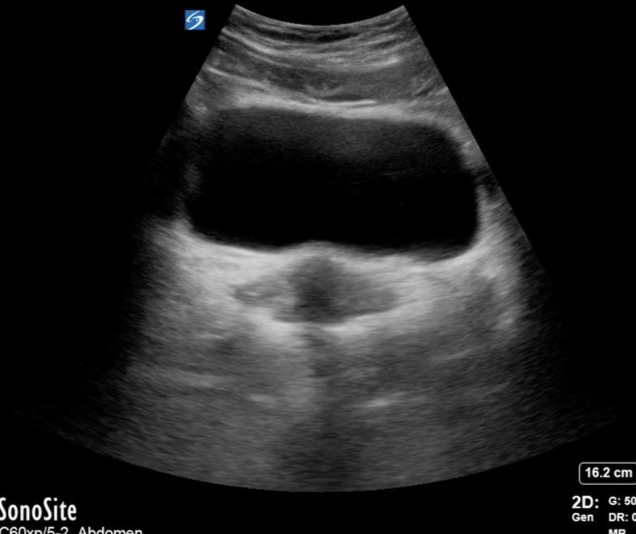
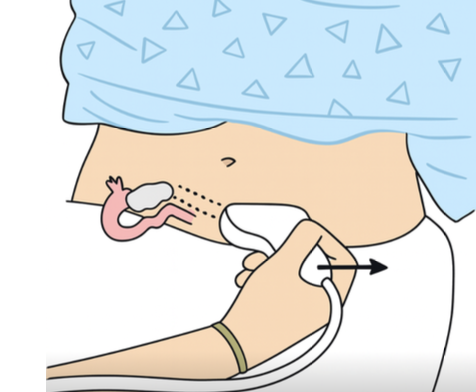
1️⃣ Start as for a trauma E-FAST bladder view (transverse suprapubic).
2️⃣ With the bladder in near field and uterus in far field, rock the probe tail → left to find the right ovary.
3️⃣ Reverse direction to visualize the left ovary.
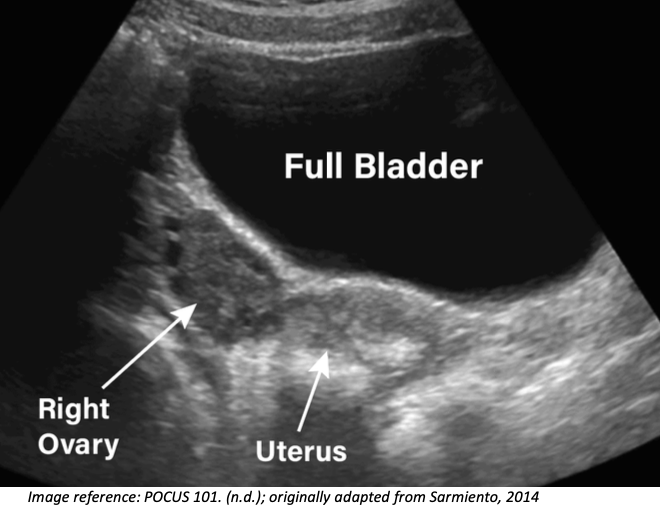
Appearance: Oval, isoechoic or mildly hypoechoic stroma with anechoic cystic follicles.
Location: Just lateral to the uterus and medial to the internal iliac vessels.
Performing the Scan
- Begin as if you were scanning the bladder in a trauma E-FAST.
-
With the probe in the transverse position, gently rock the probe’s tail toward the patient’s left to bring the right ovary into view. It may require a little cephalocaudal sweeping to find the ovary.
-
To visualize the left ovary, use the same approach in the opposite direction by rocking the tail toward the patient’s right
How Will I Know if I am Looking at an Ovary?
Appearance:
- The normal ovary will appear as an oval structure with an isoechoic, if not slightly hypoechoic stroma (the supportive connective tissue surrounding the follicles) and variable anechoic cystic follicles.
Location:
- The ovaries will appear just lateral to the uterus and medial to internal iliac vessels (Schwimer, 1985).
Common Ovarian Pathologies
Now you know how to identify the ovaries. In this section, we’ll take a look at some of the more common ovarian findings you may encounter in our adult ED population.
Simple Cyst
PoCUS features
- Anechoic, unilocular, thin/smooth walled
- Posterior acoustic enhancement (the fluid within the cyst enhances the ability of ultrasound waves to reach the posterior aspect of the structure)
- No internal vascularity on Doppler
- Round or oval in shape
- The absence of septations, papillary projections, or solid elements is crucial. If any of those features are present, the cyst is not simple and requires further characterization.
Management / Follow-up
-
Most simple cysts < 5 cm in pre-menopausal women are physiologic (e.g., follicular or corpus luteum cysts) and usually resolve spontaneously.
-
In post-menopausal women, simple cysts can still be benign, but follow-up is often recommended depending on size (usually > 1–2 cm).
-
Simple cysts > 5 cm are at much higher risk for torsion and should be considered in symptomatic patients with a large cyst (Baron and Mathai, 2023).
Hemorrhagic Cyst
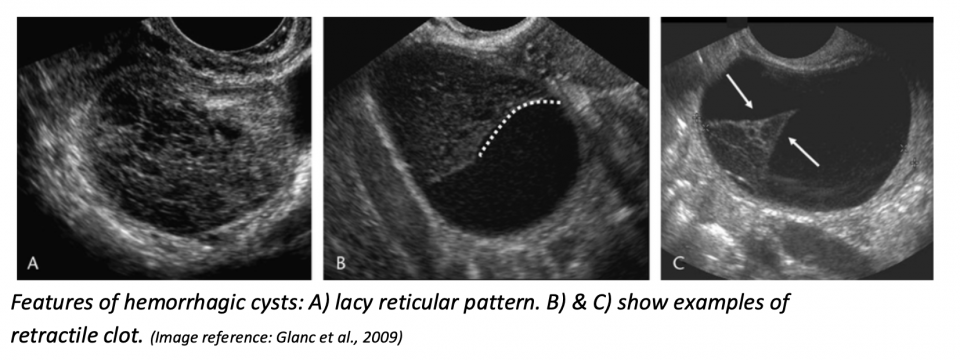
PoCUS features
-
Reticular or “lacy” pattern of fine internal echoes (“fishnet” or “cobweb” appearance) — due to fibrin strands from clotted blood
-
Fluid–fluid levels (from settling of blood products)
-
May show retracting clot: fibrin components contract, causing a concave, sharp, curvilinear or triangular internal mass that pulls away from the cyst wall
-
Usually no internal Doppler flow (but circumferential wall flow may be seen)
Management / Follow-up
-
Uncomplicated cyst rupture:
Patients with limited bleeding and no significant hemoglobin drop are best managed conservatively with observation rather than surgery.
They should be counseled on warning symptoms such as worsening pain or signs of anemia (e.g., dizziness, light-headedness) and advised to return if these occur.
Repeat ultrasound is performed only if symptoms change; routine imaging for resolution is unnecessary.
Pain control is managed with oral analgesics such as acetaminophen or NSAIDs as needed. -
Complicated cyst rupture:
Surgical consultation in the ED is indicated if there is evidence of intra-abdominal free fluid, hemodynamic instability, or significant drop in hemoglobin/hematocrit.
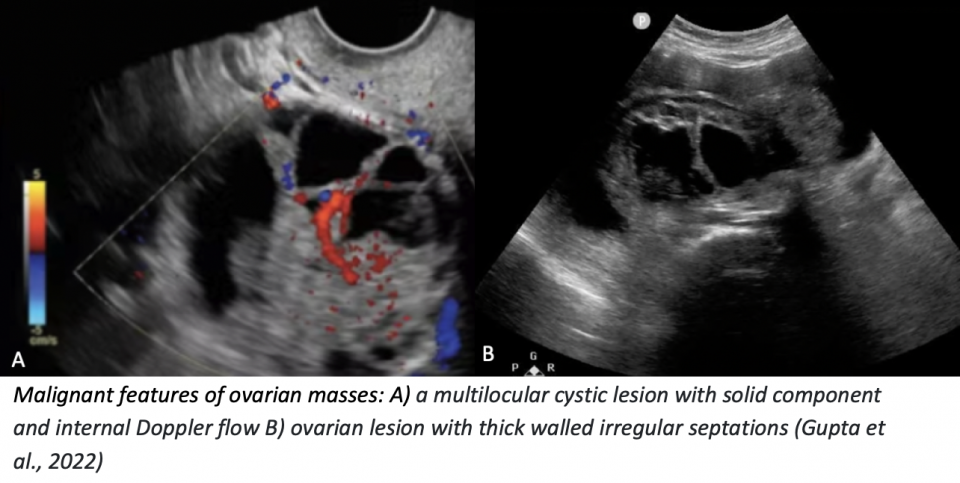
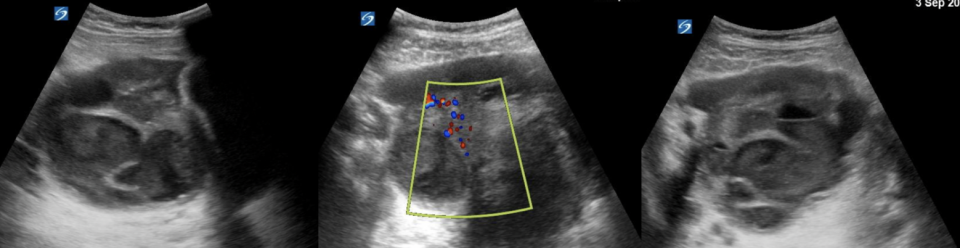
Neoplastic / Malignant Features
PoCUS features
- Thick-walled (> 2–3 mm), irregular septations
- Solid components with vascularity on Doppler
- Papillary projections (especially with flow)
- Ascites or peritoneal implants may be seen
Management / Follow-up
-
Radiology-performed ultrasound ± CT
-
Gynecology referral
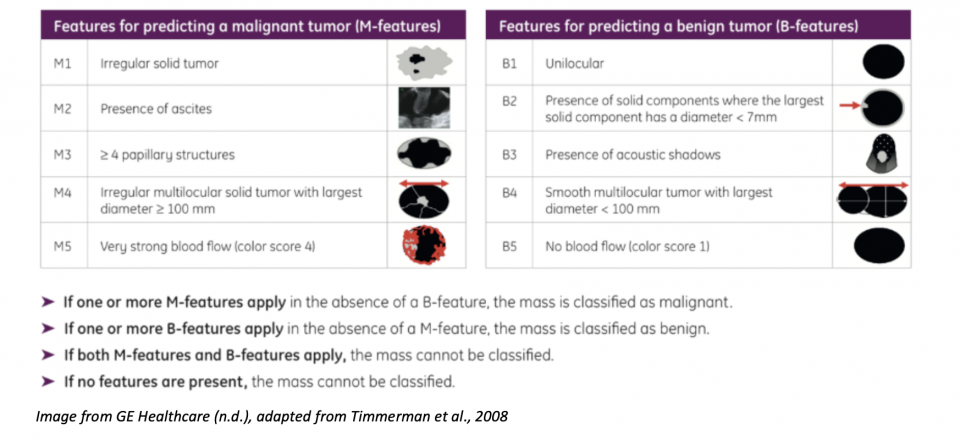
Bonus:
Here’s a helpful table from the International Ovarian Tumor Association (IOTA) outlining features of malignant vs benign ovarian masses.
(Image from GE Healthcare, n.d., adapted from Timmerman et al., 2008)
Tubo-ovarian Abscess (TOA)
PoCUS features
- Ill-defined borders, often multi-loculated
- Thick, irregular walls
- Heterogeneous internal echoes from debris, pus, or clot
- Internal septations may be present, showing the “waist sign”
- The pathognomonic finding may be the “cogwheel sign”, referring to the cross-sectional appearance of infolding projections into the fallopian tube, giving the appearance of a cogwheel (Radiopaedia, 2022).
- Absence of discrete solid vascular nodules helps distinguish from neoplasm
- Frequently associated with pelvic free fluid, which may be simple (anechoic) or complex (echogenic)
- Increased vascular flow in the wall/septa on Doppler due to inflammation (hyperemia)
Management / Follow-up
- IV antibiotics
- Gynecology consult in ED
Final Thoughts
Transabdominal ultrasound in the ED is a quick and easy way to help your patients. Looking for ovarian pathology with PoCUS is only a slight modification of the technique you already use to perform your first-trimester scans or E-FAST.
Though rare, ovarian pathology can have devastating consequences for your patient. So, if it’s on your differential — pick up the probe and start scanning.
References
-
Baron, S. L., & Mathai, J. K. (2023, July 17). Ovarian torsion. In StatPearls [Internet]. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK560675/ -
GE HealthCare. (n.d.). A guide to abnormal adnexa: Ultrasound and adnexal mass terminology. Voluson Club.
https://www.volusonclub.net/empowered-womens-health/a-guide-to-abnormal-adnexa-ultrasound-and-adnexal-mass-terminology/ -
Glanc, P., Salem, S., & Farine, D. (2009). Adnexal masses in the pregnant patient: A diagnostic and management challenge. Ultrasound Quarterly, 24(4), 225–240.
https://doi.org/10.1097/RUQ.0b013e31819032f -
Gupta, A., Kim, K. A., Feldstein, V. A., Peterson, E., Zaloudek, C. J., & Lee, S. I. (2022). Ovarian cancer detection in average-risk women: Classic- versus nonclassic-appearing adnexal lesions at US. Radiology, 305(3), 575–584.
https://doi.org/10.1148/radiol.212338 -
Karena, Z. V., & Mehta, A. D. (2023). Sonography female pelvic pathology assessment. In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK585034/ -
POCUS 101. (n.d.). Pelvic ultrasound probe position for gynecologic scanning [Image]. POCUS 101.
https://www.pocus101.com/gynecology-pelvic-ultrasound-made-easy-step-by-step-guide/ -
Sarmiento, J., Stewart, K., Aguila, J., Bagherpour, A., & Kupesic Plavsic, S. (2014). Pelvic ultrasound simulation training models and case scenarios. Donald School Journal of Ultrasound in Obstetrics and Gynecology, 8(1), 22–30.
-
Schwimer, S. R., & Lebovic, J. (1985). Transvaginal pelvic ultrasonography: Accuracy in follicle and cyst size determination. Journal of Ultrasound in Medicine, 4(2), 61–63.
-
Tabbara, F., Hariri, M., & Hitti, E. (2024). Ovarian torsion: A retrospective case series at a tertiary care center emergency department. PLOS ONE, 19(3), e0297690.
https://doi.org/10.1371/journal.pone.0297690 -
Timmerman, D., Testa, A. C., Bourne, T., Ameye, L., Jurkovic, D., Van Holsbeke, C., Paladini, D., Van Calster, B., Vergote, I., Van Huffel, S., & Valentin, L. (2008). Simple ultrasound-based rules for the diagnosis of ovarian cancer. Ultrasound in Obstetrics and Gynecology, 31(6), 681–690.
https://doi.org/10.1002/uog.5365 -
Xholli, A., Londero, A. P., Camacho Mattos, L., Vujosevic, S., & Cagnacci, A. (2023). Gynaecological pathologies leading to emergency department admissions: A cross-sectional study. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 282, 38–42.
https://doi.org/10.1016/j.ejogrb.2023.01.006 -
Yap, J. (2022). Cogwheel sign. Radiopaedia.
https://radiopaedia.org/articles/cogwheel-sign?lang=us (Accessed Oct 2025)