We continue to discuss the latest recommendations for ED management of atrial fibrillation (AF) as presented in the newly published 2014 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation. The Guidelines PDF can be downloaded from the CCS website at 2014 Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation
Clinical experience and published reports support the general belief that it is safe to proceed with cardioversion if the duration of AF/AFL is clearly less than 48 hours and the patient has no high-risk stroke characteristics.1-9 Before proceeding with cardioversion, physicians must be aware of the characteristics that put patients at high risk of immediate stroke and how to mitigate that risk. Furthermore, physicians must carefully consider the need to initiate OAC therapy prior to discharge from the ED, based on the “CHADS-65” algorithm discussed last week in Part 1. Early follow-up with a specialist is recommended to review the need for long-term OAC. The updated approach is summarized in the revised ED Treatment Algorithm (Figure).
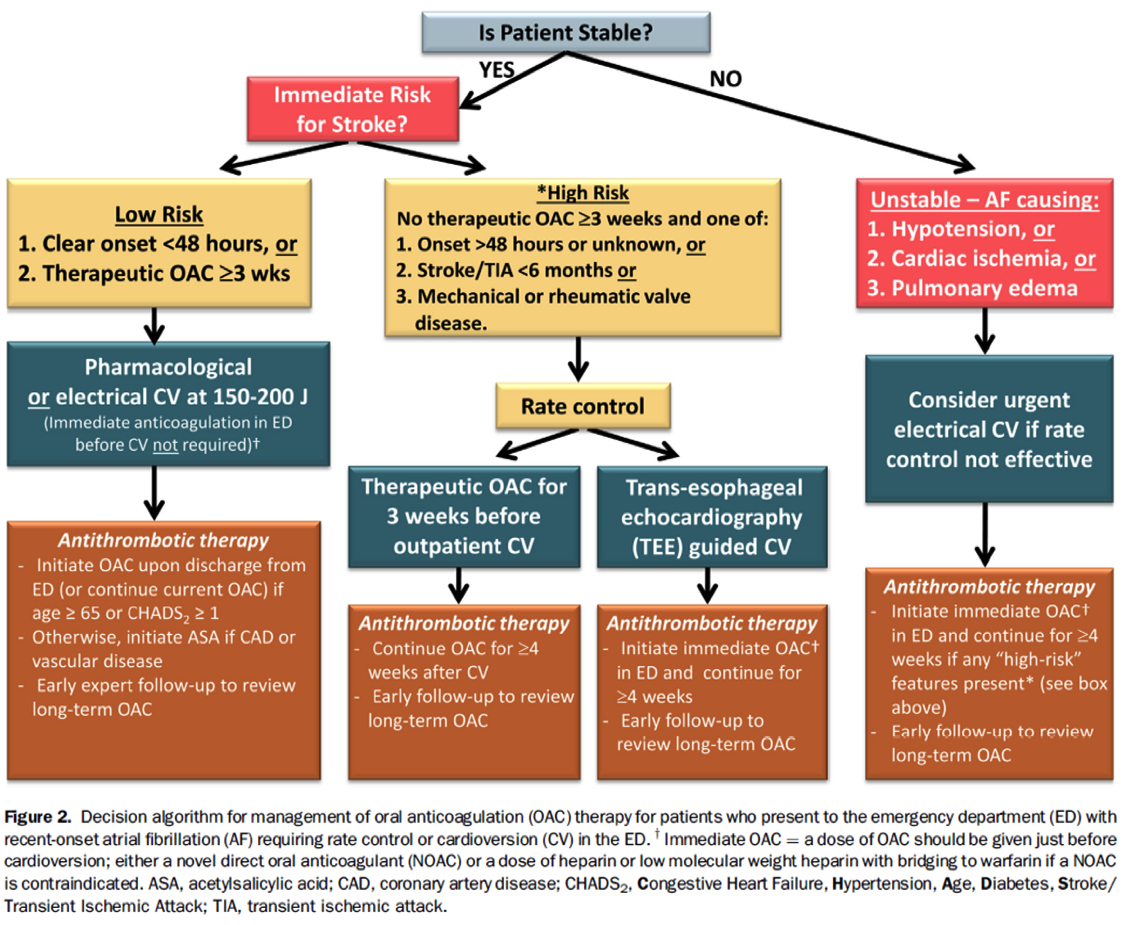
ED management of patients with recent-onset fibrillation should be based upon initial stratification for hemodynamic stability and immediate risk of stroke. Rarely does recent-onset atrial fibrillation cause instability requiring immediate electrical cardioversion. Stable low-risk patients may undergo pharmacological or electrical cardioversion without prior anticoagulation, whereas those at higher risk should not undergo cardioversion unless cleared by trans-esophageal echocardiography. At discharge, physicians should evaluate the need to prescribe oral anticoagulants or ASA and to ensure proper follow-up.
In the next posting, Part 3, we will look at the unstable AF patient with hypotension, ischemic chest pain, or pulmonary edema.
References
(1) Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 2010; 31(19):2369-2429.
(2) Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA et al. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol 2011; 57(11):e101-e198.
(3) Cairns JA, Connolly SJ, Talajic M, McMurtry MS, Stephenson M. Prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter (in press). Can J Cardiol 2011.
(4) Weigner MJ, Caulfield TA, Danias PG, Silverman DI, Manning WJ. Risk for clinical thromboembolism associated with conversion to sinus rhythm in patients with atrial fibrillation lasting less than 48 hours. Ann Intern Med 1997; 126(8):615-620.
(5) Michael JA, Stiell IG, Agarwal S, Mandavia DP. Cardioversion of paroxysmal atrial fibrillation in the emergency department. Ann Emerg Med 1999; 33:379-387.
(6) Gallagher MM, Hennessy BJ, Edvardsson N, Hart CM, Shannon MS, Obel OA et al. Embolic complications of direct current cardioversion of atrial arrhythmias: association with low intensity of anticoagulation at the time of cardioversion. J Am Coll Cardiol 2002; 40(5):926-933.
(7) Burton JH, Vinson DR, Drummond K, Strout TD, Thode HC, McInturff JJ. Electrical cardioversion of emergency department patients with atrial fibrillation. Ann Emerg Med 2004; 44(1):20-30.
(8) Stiell IG, Clement CM, Perry JJ, Vaillancourt C, Symington C, Dickinson GE et al. An aggressive protocol for rapid management and discharge of emergency department patients with recent-onset episodes of atrial fibrillation and flutter. Can J Emerg Med 2010; 12(3):181-191.
(9) Scheuermeyer F.X., Grafstein E, Stenstrom R, Innes G, Poureslami I, Sighary M. Thirty-day outcomes of emergency department patients undergoing electrical cardioversion for atrial fibrillation or flutter. Acad Emerg Med 2010; 17(4):408-415.
Ian Stiell MD
Twitter @EMO_Daddy

