Opioid Use and Misuse
Oligoanalgesia:
A landmark study in 1989 demonstrated how bad we are at providing adequate analgesia in the ED: 56% of patients in pain received no analgesia, 42% waited more than 2 hours before receiving any, and 32% received a less than optimum dose1
Bottom Line
We still don’t prescribe adequate doses of opioids to patients in acute severe pain (which, generally speaking, are safer than we think). In otherwise healthy patients, we ought to give an appropriate initial dose, and titrate to effect. However, we should also not be surprised if opioids aren’t effective in everyone.
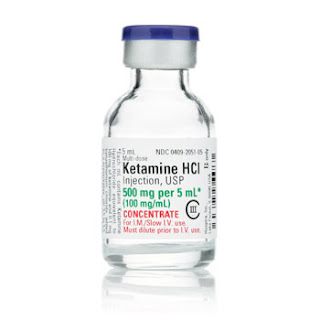
Alternative #1: Ketamine
There has been a lot research done on the use ketamine as an analgesic, in both the emergency and anesthesia literature. Ketamine is primarily an NMDA receptor antagonist, but also a weak mu and kappa agonist, as well as a serotonin, dopamine, and norepinephrine re-uptake inhibitor. This means that it not only MODULATES the painful stimulus after transmission (as the opioids do), but it may actually BLOCK the transmission of the painful impulse in the first place.
Evidence
- It has been studied in a double-blind RCT of 73 trauma patients, with a dose of 0.2mg/kg IV as an adjunct to a standard morphine 0.1mg/kg dose, resulting in less total morphine use (0.149mg/kg vs 0.202 mg/kg), a similar pain reduction, but increased neuropsychological effects (36% vs 3%).7
- It has also been studied in a double-blind RCT in addition to morphine, at two different doses (0.15mg/kg and 0.3mg/kg). Both ketamine doses achieved a superior absolute pain reduction to morphine alone, although only the higher dose maintained this advantage at the 2 hour mark. Dizziness was reported by 0% and 45% in the low and high dose ketamine groups, respectively, compared to 10% for morphine alone. Dysphoria was reported by 10% and 15% in the two ketamine groups.8
- A large retrospective case series of 530 patients receiving low-dose ketamine (~0.15mg/kg) may suggest the side effects aren’t actually that prevalent, with only 3.5% of patients having truly psychomimetic or dysphoric reactions (and even fewer requiring any sedation).9
Bottom Line
Ketamine for analgesia is experiencing a surge of interest. It appears to allow for greater pain reduction (or at least limits the amounts of opioids used), and is safe. Consider its use in cases where opioids need to be limited, or where pain is refractory. Its biggest drawback seems to be dysphoric and psychomimetic reactions, however these might be reduced by using a low dose (eg. 0.15mg/kg IV over 10 mins, +/- an infusion of 0.03-0.06mg/kg/hr)
Alternative #2: Lidocaine
A sodium channel blocker that is ubiquitous as a local anesthetic, where it totally blocks nerve transmission. May also have a role as an IV analgesic, although the mechanism is less clear. It is increasingly used in oncologic/palliative settings, as well as in severe chronic and neuropathic pain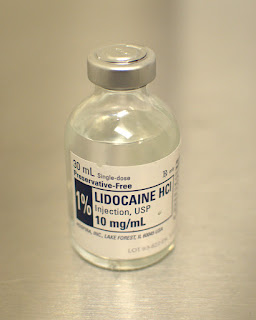
Evidence
Lidocaine at a dose of 1.5mg/kg vs. morphine 0.1mg/kg was studied in a double-blind RCT of renal colic patients – the lidocaine group had a statistically significant reduction in pain scores, with about 8.3% experiencing transient dizziness and 2.5% experiencing some peri-oral numbness.10
Another RCT looked at its use in critical limb ischemia, where a dose of 2mg/kg of lidocaine achieved statistically significant lower pain scores than morphine, without any adverse effects reported
Bottom Line
IV lidocaine has some evidence to suggest its possible use in the ED, however its unclear mechanism and unfamiliar route of administration is likely to make many physicians uncomfortable. Still, its use might be considered in the specific clinical situations studied, and with sufficient monitoring capabilities and buy-in from colleagues in other departments.
Alternative #3: Propofol
Another drug that we are used to in the ED, although usually for its indication as a procedural sedation/induction agent. It is a hypnotic/amnestic, with most of its effects coming from GABA potentiation, although with some likely sodium channel blocking and endocannabinoid properties. It has primarily been used in the setting of severe/refractory migraine
Evidence
- A prospective, non-blinded study in a migraine clinic gave an average dose of 110mg over 20-30 mins to patients, with an astounding 95% reduction in headache on a 10 point VAS, and a recurrence the next day of only 3/77 patients.11
- A more relatable double-blind RCT from 2014, of 90 ED migraine patients, compared sumatriptan 6mg SC (the migraine treatment with the strongest recommendation from the Canadian Headache Society) with propofol 30-40mg bolus, followed by 10-20mg boluses until a RASS of 3-4 was achieved (essentially procedural sedation). All patients achieved similarly remarkable pain reductions, although the propofol group achieved it quicker, with a much lower rate of recurrence in 24 hours (17% vs 55%).12
Bottom Line
While it was weakly recommended AGAINST in the most recent Canadian Headache Society guidelines13 (primarily due to concerns about its ineffectiveness and side effects of drowsiness and slurred speech), propofol is a drug we are eminently familiar with in the ED, and is potentially worth a try for the patient who is refractory to standard migraine treatments.
Dr. Francis Bakewell is a fourth-year Emergency Medicine resident at the University of Ottawa, and a MHSc. candidate in Bioethics through the Joint Centre for Bioethics at the University of Toronto.
References