Steroids in biphasic anaphylaxis
- In the patient presenting with anaphylaxis, there is a theoretical possibility that a biphasic reaction may occur. Biphasic reactions are defined as a return of symptoms after complete resolution of the initial symptoms without re-exposure to an allergen.
- The delayed response usually occurs within 8 hours, but can occur up to 72 hours after initial reaction.
- The literature reports a range of 1-20% of biphasic anaphylaxis [1], although this likely represents a significant overestimation.
- The primary action of steroids is to down-regulate the late inflammatory response, as opposed to the early phase response – the rationale for their use in anaphylaxis is based on research in other similar atopic conditions, such as asthma, but not in anaphylaxis itself [2].
- A 2012 Cochrane review examined the benefits and harms of steroid treatment in anaphylaxis, but were unable to complete the review due to a lack of RCT’s performed in this field [3].
- Furthermore, 2014 practice parameters state that there is “no definitive evidence that corticosteroids decrease the risk of biphasic reactions, although there is a theoretical possibility owing to their anti-inflammatory properties” [4].
- However, management algorithms and guidelines continue to include steroids for treatment after initial treatment with epinephrine.
- A 2015 retrospective study in two Canadian ED’s demonstrated that steroid use is NOT superior to no steroids when comparing ED revisits after seven days. Interestingly, the majority of patients who did return with a biphasic reaction were in the steroid group [5].
- This begs the question as to whether these patients had a more severe initial reaction, or were more likely to have a biphasic reaction than patients who did not receive steroids.
Bottom Line:
Steroids in sepsis
- Sepsis continues to be a topic of debate when it comes to steroids, previously the 2002 trial by Annane et al had supported its use, citing a mortality benefit, whereas the CORTICUS trial in 2008 did not yield a benefit, however, was an underpowered study [6,7].
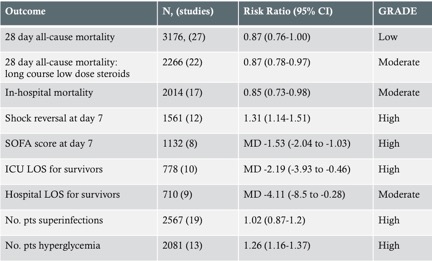
- The most recent Cochrane review in 2015 examined the effect of corticosteroids on all cause mortality at 28 days in patients with sepsis [8]:
- Overall, long course low dose steroids reduced all-cause mortality at 28 days by 13%, which was statistically significant. However, the quality of the outcome was hindered by heterogeneity across trial results, in part due to differences in dosing strategies and varied study populations.
Bottom Line:
- Steroids may favourably impact all-cause mortality at 28 days in patients with sepsis, but there are significant limitations to this evidence.
- If given, it should be given at low dose (≤400mg hydrocortisone or equivalent) for ≥3 days at full dose.
- The ADRENAL study is in progress, and will be the largest study to examine steroids in sepsis.
Steroids in pneumonia
Steroids have recently been studied in pneumonia [9], with an large RCT published in 2015 randomizing 785 patients to steroids or placebo, demonstrated that a 7 day course of Prednisone (50 mg) decreased the time required to reach clinical stability (measured by vital signs), and thereby decreased hospital length of stay and duration of IV antibiotics by one day [10].
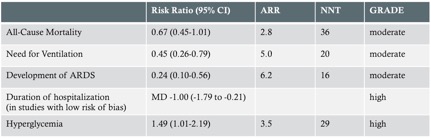
- Following the publication of this trial, an systemic review and meta-analysis was published [11], demonstrating:
 |
|
Chart modified from Siemieniuk et al [11] (ARR and NNT calculated from data)
|
- Overall, the review suggested that use of systemic corticosteroids may lead to: decreased need for mechanical ventilation, reduced ARDS and reduced hospital length of stay.
- In regards to complications, there were increased rates of hyperglycemia but no significant GI bleeds.
Bottom line:
- In patients admitted with severe community-acquired pneumonia, steroids are worth considering given the potential to reduce hospital length of stay.
- However, this benefit should be carefully weighed in patients susceptible to the side effects of steroids (hyperglycemia).
Steroids in lumbosacral radiculopathy
- Low back pain is a common presentation, and is often difficult to treat in the ED, with NSAIDs and activity modification continuing to be the mainstay of treatment.
- Previously, RCT’s and systemic reviews examining the use of steroids for lumbosacral radiculopathy have been negative [12], but an recent RCT published in JAMA demonstrated decreased disability scores in patients receiving a 15 day course of steroids versus placebo for acute sciatica [13].
- Patients in the intervention group received a tapering dose of oral prednisone for a total treatment duration of 15 days.
- Inclusion criteria in this study, however, required patients to have a herniated disc demonstrated on MRI, pain extending below the knee in a nerve root distribution and at least moderate disability (30%) as measured by the Oswestry Disability Index.
- Patients were excluded if they had chronic symptoms longer than 3 months, prior back surgery, diabetes or other contraindications to surgery.
Bottom line:
- With very strict inclusion criteria, this study demonstrates a potential benefit for steroid utilization in a small subset of patients.
- More research is required, with a focus on improvement of disability and function in patients, rather than pain improvement scores.