We have seen a large surge of the utilization of New Oral Anticoagulants (NOAC’s) in the past few years, as such, it has been a novel challenge when these patients present to the Emergency Department (ED) with life threatening bleeding. Dr. Michael Ho looks to discuss treatment options, and future options in these patients.
NOACs vs Warfarin
- Rapid onset of action
- Shorter half-life
- Less food and drug interference
- Predictable pharmacokinetics
- Ease of use and no requirement for monitoring
Reversal of anticoagulation
Warfarin
- Fresh Frozen Plasma (FFP) + Vitamin K
- Prothrombin Complex Concentrate (PCC) + Vitamin K
NOACs
- Stop all anticoagulants and antiplatelet agents
- Identify the source of bleeding and apply local and surgical measures as appropriate
- Supportive measures (volume, pRBCs, platelets) as needed
- Confirm timing of last dose of NOAC, if <4 hours consider activated charcoal
- Measure coagulation parameters: PT/INR, aPTT, anti-Xa, TT
- If patient is taking dabigatran and
-
- TT is normal: there is no drug on board
- TT abnormal but aPTT normal: clinically insignificant drug on board
-
- If patient is taking apixaban or rivaroxaban and
-
- Anti-Xa < 0.1: no drug on board
- Calculate CrCl and estimate half-life [1]
- Most NOACs have a half-life of approximately 12-14 hours
- Accumulation of drug does not occur
- Low plasma concentrations of all NOACs are expected after one half-life
- Administer 4-factor PCC of FEIBA [7]
- The evidence for administering PCC or activated PCC (FEIBA) for life threatening bleeding is based off weak evidence in animal models, in vitro studies and studies on healthy volunteers.
- Evidence slightly favours FEIBA for Dabigatran reversal and 4-factor PCC for Xa inhibitor reversal.
- Requires high doses (>50 U/kg) to “overload” the coagulation system with clotting factors and induce thrombin generation in the setting of thrombin of Xa inhibition.
- Concerns with this strategy: non-specific reversal, increased risk of thrombosis with high dose PCC, inconsistent experimental data, and no human data demonstrating benefit.
- At the Ottawa Hospital (TOH) we currently use FEIBA for all NOAC bleeding for simplicity.
- For patients on Dabigatran, hemodialysis can be considered [7].
- 50% of active Dabigatran is removed after 4 hours of HD in ESRD patients
- Xa inhibitors are too highly protein bound for HD to be useful.
Idarucizumab (Praxbind)
- 90 patients, 86 were taking Dabigatran for atrial fibrillation
- Group A: Life threatening bleeding: 51 patients
- Group B: Emergency procedures: 39 patients
- Group A: Time to hemostasis, modified Rankin scores for ICH patients and hemodynamic stability.
- Group B: intraprocedural hemostasis, periprocedural bleeding for 24 hours
- Primary
- 11/51 patients had normal Dabigatran levels at baseline, they were excluded from analysis.
- At 4 hours, 100% of the remaining 40 patients were reversed with Praxbind
- Normalization of dTT and ECG occurred within 30 minutes of Praxbind infusion.
- Secondary
- Group A:
- Bleeding assessable in 35/51 patients
- Median time to hemostasis: 11.4 hours
- Group B:
- Normal hemostasis in 33/36 patients
- Adverse events:
- 18 deaths (20% mortality rate)
- 5 thrombotic events (1 in the first 72 hours, others after day 7)
- 2 GI bleeds
- Group A:
- International, mutli-center trial
- Robust demonstration of biochemical reversal
- Hemostasis evaluated
- Only 2 patients lost to follow up.
- Group A (Life threatening bleeding)
- No Control group
- Authors state a control group “…would be unethical to assign patients to receive placebo or no active treatment” – the authors here are making a big assumption that their drug is already clinically effective and safe.
- How can we make any conclusions about the clinical efficacy and safety of this drug without a control group?
- Small sample size
- Difficult to make conclusions about safety
- Mortality rate was high (20%)
- Typical mortality rate of major extracranial bleeding is 5-8% in other studies. Only 4/90 (4.4%) of deaths were due to ICH. Was this study group just very sick, or did the study drug increase the mortality rate? Without a control group, there is no way to know.
- Only 50% of patients in Group A with “life threatening bleeding” required a blood transfusion.
- They did not report bleeding scores
- They did not report modified Rankin score outcomes for ICH patients
- Study was funded by Boehringer Ingelheim, the company that engineered the drug
- No Control group
- Group B (emergency procedures)
- Were these procedures truly emergent?
- Most commonly performed procedure: orthopedic OR
- Other included procedures:
- LP, abscess I&D, HD line placement, ureteric stents
- No neurosurgical interventions
- Subjective assessment of intraoperative hemostasis
- Were these procedures truly emergent?
Bottom Line
- This study confirms phase I trial findings of biochemical reversal of effect in bleeding patients and patients requiring emergency procedures
- (Subjectively) normal hemostasis was reported
- Does not convincingly report a clinically meaningful benefit
- Safety still in question
Availability and Cost
- Under accelerated approval by FDA in US and Europe
- Submitted for approval in Canada Feb 2016
- Expected cost: $3400 per dose (2 x 2.5g)
- Cost direct to hospital pharmacy
- Comparison
- FEIBA: $3500
- PCC: $1500
- 6 units FFP: $1500
- These costs are direct to Canadian Blood Services
- Expected to be available in the ER at TOH, use restricted by Thrombosis
- Expected indication: life threatening bleeding (including ICH) and the need for emergency surgery / procedure within 8 hours.
Antidote Pitfalls
- Worth mentioning that having this (expensive) antidote might lead to [1]:
- Overuse when it is unclear if patient is taking an anticoagulant OR which one they are taking
- Careless timing of invasive procedures
- Delay in necessary intervention
- We also have no idea how to use this drug in the case of overdose.
Does reversal of anticoagulation help our patients?
We’ve been talking a bit about reversing bleeding with NOACs, but does reversal make a clinically meaningful difference to our patients? To look at this question, the best place to look is warfarin. Warfarin has been around for a long time, and reversal is easy (replace the factors) and fast (PCC).
Evidence that rapid reversal makes no difference:
- Zubkov et al. Arch Neurol 2008 [13]
- 88 patient prospective cohort with warfarin-related ICH reversed with FFP and Vitamin K.
- Initial INR and time to INR reversal had no correlation with survival to 7 days in univariate or multivariate analyses.
- Sarode et al. Circulation 2013 [5]
- 202 patient RCT reversing warfarin-related major bleeding with FFP vs PCC
- Similar hemostatic efficacy at 24 hours
- No difference in 30-day mortality rate
- The 45-day mortality rate was 9.7% vs 4.6% favouring FFP (authors state these deaths not related to reversal).
- Alonso et al. Thromb Haemost 2013 [14]
- 71 patient prospective cohort of warfarin-related ICH, reversed with PCC + Vitamin K
- Baseline INR, anticoagulation reversal, hematoma enlargement were not related to functional outcomes.
Evidence that rapid reversal is helpful:
- Tilton et al. Ann Pharm 2014 [15]
- 403 patient retrospective study of 3-factor PCC for reversal of warfarin-related acute bleeding
- Achieving INR < 1.5 correlated with survival (OR 3.8, P<0.01).
- Tazarourte et al. Crit Care 2014 [16]
- 822 patient prospective study of 4-factor PCC + Vitamin K for reversal of warfarin-related severe bleeding
- Giving PCC ≥ 20 units/kg and vitamin K ≥ 5 mg IV within 8 hours was associated with:
- 2-fold reduction in 7-day mortality in all patients
- 3-fold reduction in 7 day mortality for ICH patients
- Steiner et al. Int J Stroke 2011 (INCH trial) [17]
- The INCH trial is an open-label RCT comparing reversal of warfarin-related ICH with FFP vs PCC. These unpublished results were presented at the International Stroke Conference (Feb 2016) and are available online.
- In favour of PCC:
- Decreased rate of hematoma expansion
- Mortality rate 19% vs 35% (non-sig, P=0.14)
- All 4 deaths in the first 48 hours were int he FFP group – all of these were related to hematoma expansion
- First death in PCC group was at day 5, due to cardiac arrest
- No difference in functional outcomes
Upcoming development: Andexanet alfa (Xa inhibitor reversal agent)
ANNEXA Trials
- Anti-Xa activity reduced by 94% compared to 21% with placebo
- Thrombin generation restored to 100% vs 11%
- Anti-Xa activity reduced by 92% compared to 18% with placebo
- Thrombin generation restored 98% vs 7%.
Phase II Study
- Estimated enrolment of 270 patients with major bleeding while using a Xa inhibitor in the last 18 hours
- Co-primary efficacy endpoints
- Change in Anti-Xa levels within 2 hours
- Effective hemostasis within 12 hours
- 45-day safety follow up
- No control group
Upcoming development: Ciraparantag / PER977 (NOAC and Heparin reversal)
- Rat tail transection model using Dabigatran, Rivaroxaban, Apixaban and Edoxaban
- 12.5 mg PER977 decreased bleeding by >90% vs control
- Rats given Edoxaban: thromboelastography assays normalized within 30 minutes with 20 mg/kg PER977.
- Human in vitro study: reduced anti-Xa activity of Rivaroxaban, Apixaban, Enoxaparin in dose-dependent relationship
- A phase I study of 80 healthy volunteers showed rapid reversal of whole blood clotting time in patients receiving Edoxaban
- Phase II trials are ongoing..
Bottom Lines
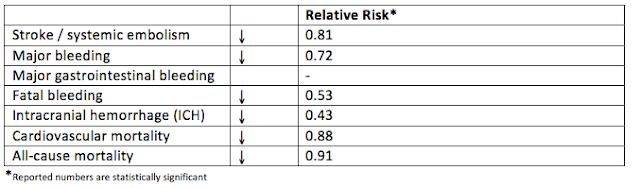
- NOACs are safer than warfarin, and are here to stay.
- Reversal of anticoagulation has not convincingly been shown to improve clinical outcomes, even when it is safe and effective.
- Reversal agents for NOACs are coming, whether we want them or not. Their biochemical results are robust, but their clinical benefits are not yet proven. We will likely be forced to use these drugs without evidence of clinical benefit for the time being.
- Idarucizumab (Praxbind) will likely soon be available in Canadian EDs, and they will be indicated for life threatening bleeding and emergency procedures/surgery.
- Drugs to watch for:
- Andexant alfa (Xa inhibitor reversal)
- Ciraparantag (NOAC and heparin reversal)
References