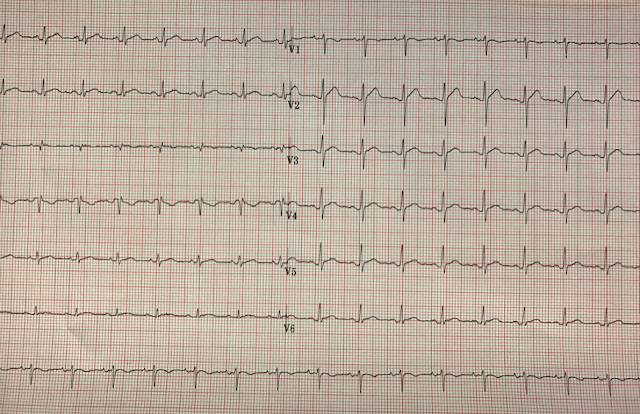
A young, previously healthy male in his 30s presents to the ED from his family physicians office with chest pain and an abnormal ECG. He has a 3-4 day history of non-radiating upper back pain and sensation of chest tightness that is pleuritic in nature and worse when supine. In addition there is a history of fever, chills, myalgias and night sweats. He has no recent travel history. He denies any SOB, cough, orthopnea, PND or syncope.
There is no IV drug use, immunocompromise or diabetes. He has no previous cardiac history other than a possible history of pericarditis a year ago. There is no personal history of PE/DVT.
On initial presentation the patient was febrile at 38.1C and tachycardic in the 120s. His blood pressure was normal at 114/79. Respiratory rate and oxygen saturation were normal on room air.
His cardiovascular exam was normal, other than an S3. There was no pericardial rub. Respiratory exam was unremarkable.
Laboratory investigations were unremarkable, including an undetectable troponin level.
What is your differential diagnosis?
The top two differential diagnoses at this point were pericarditis vs. pulmonary embolism (which can be a noninfectious cause of fever).
What is your next step? CXR? CT-PE? POCUS?
In this case the next step was POCUS. Take a look at the clips below.
Subxiphoid
Parasternal Long
Apical 4-Chamber
Discussion
A clinically significant pericardial effusion was found which is more consistent with a diagnosis of pericarditis. This finding prompted the ED physician to contact the cardiology team for an admission to observe the effusion.
A comprehensive echocardiogram completed next day showed a moderate size pericardial effusion with RA and LA collapse and a non-collapsable IVC dilation that suggested a hemodynamic effect. The LV systolic function was interpreted as borderline reduced.
Conclusion
POCUS helped to focus in on the diagnosis and avoided the significant radiation dose of a CT-PE for this patient! It also helped risk stratify as the effusion (along with the persistent tachycardia), and prompted a call to cardiology and subsequent admission.
Expert Comment – Dr. Michael Woo
Be cautious when commenting on the size of an effusion when only looking at the subxiphoid view. Yes, subxiphoid is the best to identify effusion, however the operator can make it look much larger than it seems and also demonstrate some sonographic RV collapse as well, which can be very misleading. Subxiphoid can be very helpful in identify presence or absence of PCE but should be careful when talking about the size of effusion unless in conjunction with other echo views (PSL, A4C, PSS).
*Details of the case have been anonymized and altered in order to protect patient privacy*
Case by:
Dr. Julia Traer PGY-3 – University of Ottawa
Expert Reviewers:
Dr. Paul Pageau – Ultrasonography Program Director
Dr. Michael Woo – EMUS Fellowship Director
For more information on our POCUS program please see Clinical Sonography Ottawa