Point-of-Care Ultrasonography (POCUS) is a valuable tool in the diagnostic armamentarium of the emergency physician. We have been successfully using it to the place lines, diagnose AAAs and assess the cardiac function of our dyspnea patients for awhile now. But what about the lungs? Typically air is thought of as the enemy of ultrasound, but can we successfully use it to diagnose acute respiratory conditions despite this? In this Grand Rounds review, Dr. Elizabeth Lalande goes through the use of POCUS in the diagnosis of Acute Cardiogenic Pulmonary Edema in the undifferentiated, dyspneic patient.
Objectives:
1. Definitions in lung ultrasound (US)
2. The role of POCUS in diagnosing acute cardiogenic pulmonary edema
Definitions in Lung Ultrasound
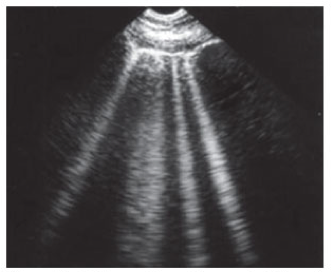
B-line: A discrete laser-like, vertical, hyperechoic reverberation artifact. It arises from the pleural line, extends to the bottom of the screen without fading, and moves synchronously with lung sliding.
First described in 1982 by Ziskin et al. and initially termed”The Comet Tail Artifact”
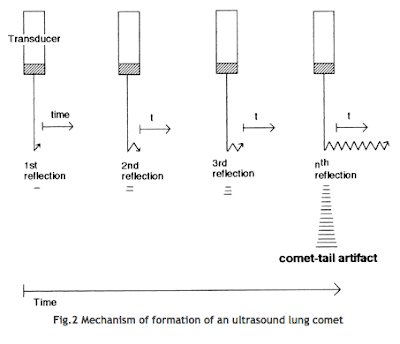
Physics of the B-line: Occurs when there is a change in acoustic impedance between an object and its surroundings. The reflection of the beam creates a phenomenon called “resonance.” The US beam gets trapped within the system and results in an endless “to-and-fro” mechanism. This results in an endless beam as seen on the screen.
|
Positive zone for B-lines: A positive zone is determined when there are at least 3 B-lines in one intercostal space that can be seen at any moment during a respiratory cycle.
Alveolo-interstitial syndrome (AIS): This syndrome is defined by a B-profile, as described by Lichtenstein DA and Mezière GA in their 2008 study: “Relevance of Lung Ultrasound in the Diagnosis of Acute Respiratory Failure, The BLUE protocol” published in Chest (2). The B-profile will have two separate, positive zones for B-lines, as previously defined, bilaterally.
|
|
Lung US profiles. From Lichtenstein DA and Mezière GA, Relevance of Lung Ultrasound in the Diagnosis of Acute Respiratory Failure, The BLUE protocol. (2)
Role of POCUS in Diagnosing Pulmonary EdemaThe sensitivity of POCUS for AIS is around 97% with a specificity of 95%. Considering that previous studies looking at the test characteristics of CXR, which is used on a daily basis for this purpose, showed a sensitivity ranging from 50 to 70% for AIS as interpreted by a Cardiologist, these figures are quite impressive.
The differential diagnosis for AIS, however, includes a variety of lung conditions not just ACPE but also acute respiratory distress syndrome, interstitial pneumonia and diffuse parenchymal lung disease, as described by the International evidence-based recommendations for Point-of-Care lung ultrasound, published in 2012 (3). So the clinical context of the scan is as important as the scan itself.
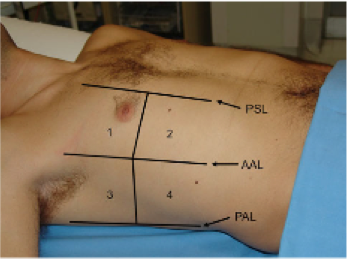
In terms of technique to elicit the B-profile, the best method was described by Volpicelli et al. in 2006. They described an 8 zones technique, 4 zones on each side of the thorax, as shown below:
|
The next question after a scanning protocol is determined is, can we accurately use POCUS to diagnose ACPE in the ED?
Fortunately, there are two major literature sources that can answer that for us:
These patients all presented with acute dyspnea and a suspicion of ACPE, which is pretty similar to our population in the ED. There was no restriction on the protocol, machine or operator performing the scan used as long as they used B-lines to make the diagnosis and the physicians performing the scan was a non-radiologist at the bedside.
The primary outcome was the clinical diagnosis of ACPE using POCUS with B-lines and the reference standard was final diagnosis at clinical follow-up. The pooled sensitivity was 94% and specificity was 93%. They did another analysis without 3 of the studies that could alter the estimates and found similar results. This study showed us that lung US has great test characteristics to diagnosis ACPE.
This review looked at the operating test characteristics of the different modalities used by emergency physicians (EPs) for the diagnosis of ACPE among patients presenting to the ED with dyspnea. They included the performance of lung US in the diagnostic work-up. Studies eligible focused on the diagnosis of acute heart failure in the ED population.
Their search for lung US studies was not limited to a specific protocol but they narrowed their inclusion of studies investigating lung US and echocardiography to those that had EPs both performing and interpreting the lung US.
Eight studies were included in the final analysis for lung US. Their results: a pooled sensitivity of 85% and specificity of 92% with a +LR of 7.4 and a negative one of 0.16 for lung US. Once again, this study has demonstrated that lung US is a great diagnostic tool for us when looking for ACPE in the acute, undifferentiated dysnpneic patient.
How about integrating cardiac views as well?
ACPE comes from a sick heart. It is certainly useful to visualize the left ventricular systolic function to assess if it goes in hand with the diagnosis of ACPE. If the echo views show a depressed systolic left ventricular function, then it really helps confirm the diagnosis.
Conclusions:
1. Lung US is a great tool to diagnose ACPE, with excellent test characteristics.
2. An eight zone protocol can be used at the bedside to look for the B-profile in your patients with undifferentiated dyspnea. Remember a B-profile consists of at least 3 B-lines in one intercostal space.
3. Don’t forget to look at the heart as well, to increase your post-test probability of finding the right diagnosis for your patient!
—- Dr. Elizabeth Lalande, MD, FRCPC is an Emergency Medicine POCUS Fellow at the University of Ottawa. She also works as a staff physician at The Ottawa Hospital.
Edited and Formatted by Dr. R Suttie, PGY2, Emergency Medicine.
References:
1. Lichtenstein DA and coll., The Comet-tail Artifact: An Ultrasound Sign of Alveolar-Interstitial Syndrome. Am J Respir Crit Care Med 1997;156:1640–1646.
2. Lichtenstein DA and Mezière GA, Relevance of Lung Ultrasound in the Diagnosis of Acute Respiratory Failure* The BLUE Protocol. CHEST 2008;134:117–125.
3. Volpicelli G and coll., International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012;38:577–591.
4. Volpicelli G and coll., Bedside lung ultrasound in the assessment of alveolar-interstitial syndrome. AJEM 2006; 24(6):689-96.
5. Al Deeb M and coll., Point-of-care ultrasonography for the Diagnosis of Acute Cariogenic Pulmonary Edema in Patients Presenting with Acute Dyspnea: A systematic Review and Meta-Analysis. Acad Emer Med 2014;21:844–852.
6. Martindale JL and coll., Diagnosing Acute Heart Failure in the Emergency Department: A Systematic Review and Meta-analysis. Acad Emer Med 2016;23:223–242.



Great read! In patients with a low pretest probability for ACPE, a negative US study can almost exclude the possibility of ACPE. Further studies including large numbers of ED patients presenting with undifferentiated dyspnea are required to gain more valid and reliable estimates of test accuracy in ED patients.