Pediatric endotracheal intubation is an uncommon procedure in the Emergency Department (ED); even in high volume tertiary pediatric centres the incidence has been reported at 8-10/10,000 patients. While infrequent, pediatric airway management is an essential and life-saving skill that all ER physicians must be prepared for. Much of the knowledge and skill set from the adult world is applicable here, however there are several important differences that are unique to the pediatric population.
Objectives:
- Provide a basic review of pediatric airway physiology + anatomy
- Discuss predictors of the pediatric difficult airway
- Review the literature on pediatric ER intubation practices and associated complications
- Review Delayed Sequence Intubation (DSI) and the pediatric surgical airway
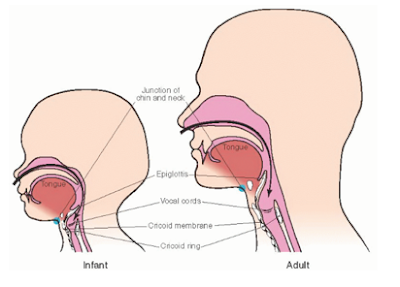
- Large occiput + head à Add a shoulder roll to align the airway axes
- Large Tongue à obstruction more common, maneuvers to open the airway may be necessary (eg jaw thrust)
- Superior larynx and anterior vocal cords + floppy epiglottis à visualization can be more challenging, consider a straight blade in younger children to lift the large epiglottis
- Large stomach with relatively small lungs à consider early NG tube
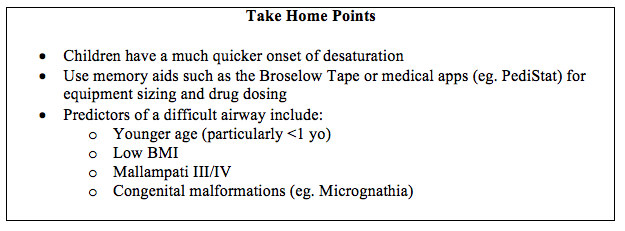
2. Physiologically, kids have a considerably shorter time to desaturation than adults and their relatively larger extracellular fluid compartment means a quicker onset and shorter duration of RSI drugs16.
- There are many different equations out there to figure out sizing of tubes, blades, masks, etc., but the bottom line is that it’s too much to memorize for something you won’t need to use often, so to reduce error in critical situations use memory aids such as the Broselow tape or your favourite medical app
- < 1 year old
- Mallampati score (if attainable) III + IV
- Low BMI
- Children undergoing cardiac and oromaxillofacial surgery patients – likely due to higher proportion craniofacial dysmorphisms eg. Cleft palate, micrognathia
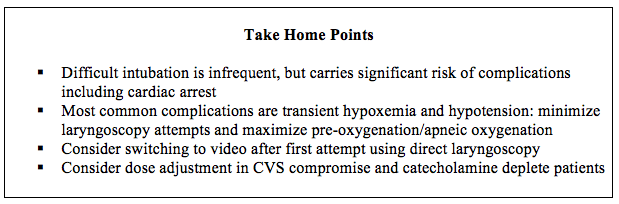
- The incidence of pediatric intubations was found to be 9/10,000
- 79% of intubations were for medical conditions (seizure most commonly), 21% were for trauma
- Median age was 3, with 25% of intubations being in the <1 population
- First pass success rate was 78%
- First pass rate without hypotension or hypoxia was only 49%
- Difficult intubation was seen in 7% of cases, but all intubations were ultimately successful
- Ketamine was the most commonly used mono-agent and was the induction agent of choice in patients with CVS compromise
- More than two intubation attempts
- Weight < 10kg
- Short thyromental distance
- 3 direct laryngoscopy attempts before switching to indirect technique
|
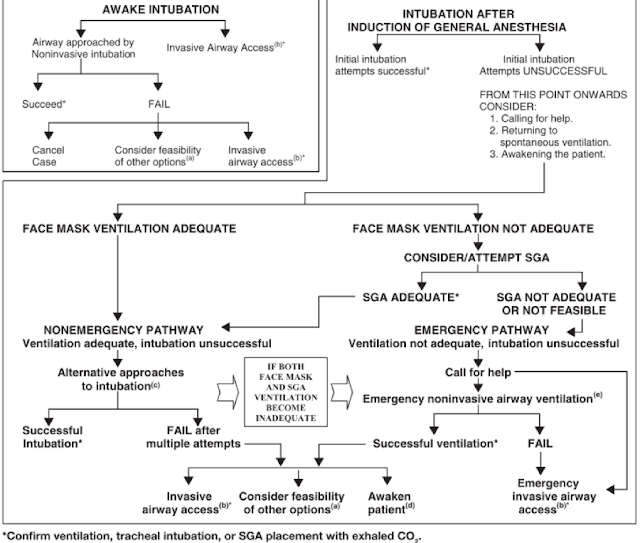
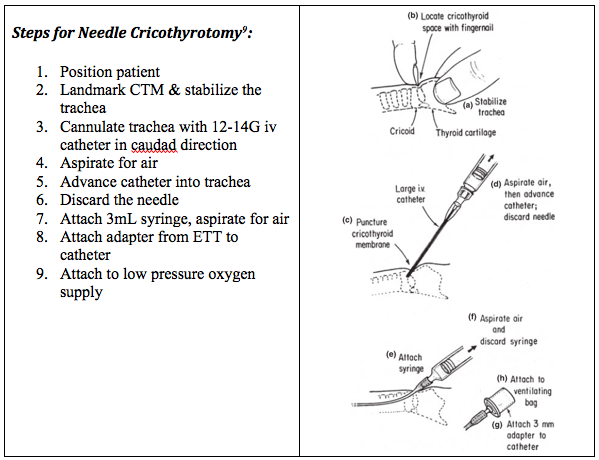
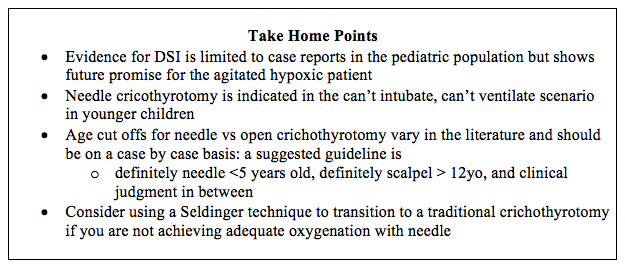
Finally, if you find yourself in the exceedingly rare but completely terrifying can’t intubate, can’t ventilate scenario with a pediatric patient, remember that needle cricothyrotomy is indicated in younger children14.

Dr. Rebecca Brown, MD, CCFP – is a third year resident in the CCFP-EM Program at the University of Ottawa. Edited and Formatted by Dr. Rob Suttie, PGY2 at the University of Ottawa
|