Many aspects of cardiac arrest care are likely to change in the not-so-distant future. Let’s take a system-level view of cardiac arrest care and see what we can do to conservatively start to move in the direction of more regionalized care. We’ll also take a further evidence based look at Cardiac Arrest Centres; what they are, and what they entail for patients. Note that some of the systems related components in this post may be specific to care in the Ottawa Valley.
Introduction: Cardiac Arrest –The Current System
Pre-hospital Medical VSA Protocol for Advanced Care Paramedics (ACP)
- Interventions:
- CPR (including Lucas mechanical CPR system)
- Defibrillation
- Lidocaine
- Fluids
- Supraglottic airway
- Intubation
- Mandatory Patch Point: They must patch to the base hospital physician (BHP) following 3 rounds of epinephrine ( every 4min) or after 3rd analysis
- Exceptions to this rule: “Unusual circumstances” (ex: overdose), hypothermia, airway obstruction
Pre-hospital Return of Spontaneous Circulation (ROSC) Protocol for ACPs
- Targets:
- SBP≥ 90mmHg
- Oxygen saturation ≥94%
- EtCO2 35-40 mmHg
- Assessments:
- 12 lead ECG
- Interventions:
- Fluids
- Dopamine
- Upon ROSC they must transport to closest hospital
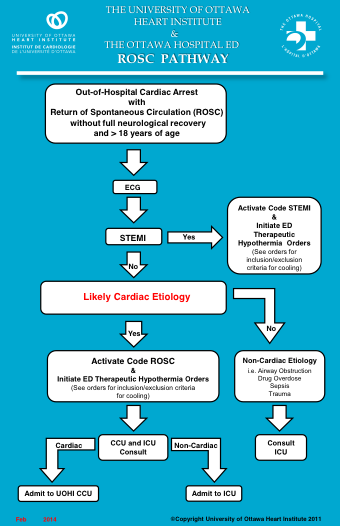
The Ottawa Hospital – Code ROSC Pathway
- Upon ROSC in the ED a 12 lead ECG is performed:
- If STEMI positive: the patient will proceed emergently to the cath lab
- If STEMI negative: ICU and Cardiology will both assess the patient to decide which is the appropriate service
- There are challenges with determining disposition with STEMI negative patients with a shockable rhythm in the field without a clearly non-cardiac etiology (especially when a cardiology staff or fellow are not readily available)
Ottawa Out-of-Hospital Cardiac Arrest (OHCA) Data
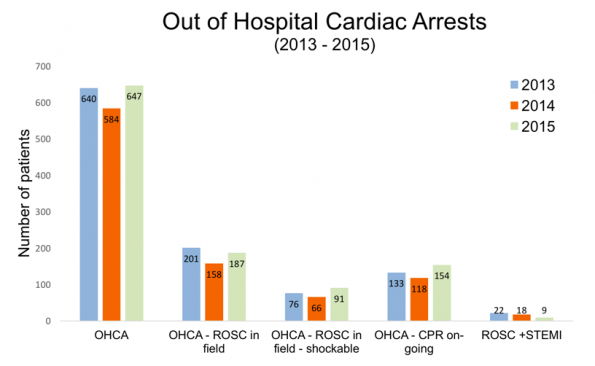
OHCA in Ottawa region (2013-2015): includes transports done by OPS, Renfrew, and Prescott Russell
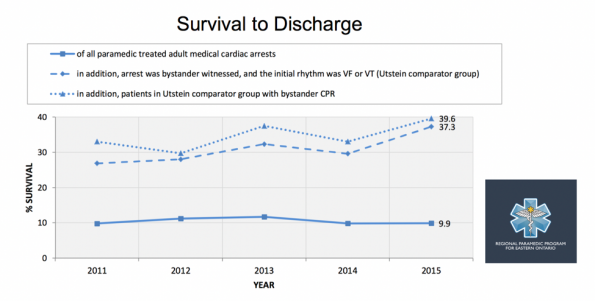
Survival from OHCA (RPPEO Region): Survival roughly stable over time
Part I: ROSC
Post Cardiac Arrest Syndrome: Results from resumption of spontaneous circulation after complete whole body ischemia
- Components:
- Unresolved pathological process causing arrest
- Brain injury
- Myocardial dysfunction
- Systemic ischemia/reperfusion
- Pillars of ROSC care:
- Cardiovascular care
- PCI
- Hemodynamic targets (SBP ≥90; MAP ≥65)
- Targeted Temperature Management (TTM)
- Comatose ROSC patients should have TTM at 32-36ºC for 24 hrs
- Respiratory care
- Oxygenation (target Sp02≥94%) and ventilation (target normal PC02)
- Neurologic care
- Seizure management, no “early” prognostication (do not prognosticate until 72hrs after patient reaches normothermia)
- Cardiovascular care
Cardiac arrest centres
- Historical context: Initially cardiac arrest centres driven by access to therapeutic hypothermia and aggressive cooling. After the 2015 ILCOR guidelines emphasized TTM interest diminished.
- AHA 2015 guidelines in regards to regionalized cardiac arrest centres4:
- “A regionalized approach to OHCA resuscitation that includes the use of cardiac resuscitation centre’s may be considered (Class IIb, Level of Evidence C-LD).”
However, there have now been new studies since 2015 emphasizing the benefit of cardiac arrest centres.
- Schober et al. Admission of Out-of-Hospital Cardiac Arrest to a High Volume Cardiac Arrest Centre is Linked to Improved Outcome. Resuscitation 2016
- Retrospective study from 2013-2015 in Vienna involving 861 patients
- Survival examined in relation to hospital admission rate of VSA patients/year
- Admit to high frequency centre (>100 VSA patients per year) had an OR of 5.2 (1.2 –7) p= 0.025 for survival with good neurologic outcome (CPC 1-2)
- Stub et al. Association between hospital post-resuscitative performance and clinical outcomes after out-of-hospital cardiac arrest. Resuscitation 20156
- Retrospective study of ROC PRIMED cohort from 2007-2009 involving over 3000 patients in US and Canada
- Survival examined in relation to how adherent hospitals were with respect to 3 factors:
- 1) Coronary angiography within 24h
- 2) TTM
- 3) No prognostication for 72hrs
- Survival to discharge in high performers was 35.1% compared with 16.2% in low performers (and survival with modified Rankin Score ≤3 of 26% vs 8.4%)
- Patterson et al. A Randomised tRial of Expedited transfer to a cardiac arrest centre for non-ST elevation ventricular fibrillation out-of-hospital cardiac arrest: The ARREST pilot randomised trial. Resuscitation 2017. 7
- Feasibility study for larger RCT looking at OHCA VF arrests without STEMI randomized to ROSC centre vs closest hospital in UK
- Primary outcome: 30d mortality
- Secondary outcomes: Neurologic Performance
- Found to be feasible – hopefully full RCT will answer this question definitively
PCI for OHCA
PCI is one of the main components of cardiac arrest centers
- There is clarity for OHCA with STEMI (These patients should go emergently to cath lab)
- Uncertainty for ROSC patients without ST elevation but shockable rhythm
AHA 2015 Guidelines:
- “Emergency cath is reasonable for select (eg, electrically or HD unstable) adult patients after OHCA of suspected cardiac origin but without ST elevation on ECG (Class IIa, LOE B-NR)4”
However, there are numerous benefits to PCI in OHCA patients:
- Culprit lesion in 59-71% of OHCA without an obvious non-cardiac etiology
- ECG and biomarkers have poor sensitivity (42%) in ROSC patients
- Access to intra-aortic balloon pump, cooling catheter, LV function
There is mounting evidence for PCI in all ROSC patients with a shockable rhythm
- Hollenbeck et al. Early cardiac catheterization is associated with improved survival in comatose survivors of cardiac arrest without STEMI. Resuscitation 2014
- 269 patients; all VF/VT arrests, USA
- Early cath (on arrival or initiation of TTM) vs late cath (during admission)
- Primary outcome: survival to hospital discharge
- Secondary outcomes: neurologic outcome
- Mortality: early cath 34.3% vs 51.4 % in no early cath (P<0.01)
- Cerebral Performance Category (CPC) 1-2: 60.7% in early cath vs 44.5% in no early cath (P<0.01)
- Patel et al. Trends and Outcomes of Coronary Angiography and Percutaneous Coronary Intervention After Out-of-Hospital Cardiac Arrest Associated With Ventricular Fibrillation or Pulseless Ventricular Tachycardia. JAMA Cardiology 2016
- Observational study using NIS database (USA), >400 000 patients with VF/VT OHCA from 2000-2012
- Use of PCI in patients with VF/VT OHCA without ST elevation increased (19.3% to 33.9% p<0.001)
- Survival to discharge in patientts without STE increased (43.3 to 56.8% p<0.001)
- Cath had OR of 6.26 (5.93 –61) for survival to discharge
ROSC Patient Bypass – Transport Safety
If we are advocating bypassing closer EDs to bring patients to a cardiac arrest centre what about safety during transport?
- Re-arrest rate estimated at 18% for VF/VT during transport to hospital12
- A number of studies have looked at transport bypass in pre-hospital VSA which found no association between transport time and survival13-14
- Perhaps best study looking at this issue was Cudnik et al. A geospatial assessment of transport distance and survival to discharge in out of hospital cardiac arrest patients: Implications for resuscitation centers. Resuscitation 201015
- Secondary analysis of ROC study, 7540 patients (2005 -2007)
- Those taken to further hospital had better survival compared to a closer hospital for VF/VT (32.8% vs 25.6% p<0.001)
- Distance (per km) OR 1.00 (0.99 – 1.01) and transport to closest hospital OR 0.82 (0.69 – 0.97)
- Limitations: Overall transport distances were modest
Ottawa ROSC Data
What if the Ottawa Civic Hospital was made into a regionalized cardiac arrest centre?
- One could bypass patients with refractory VF/VT (defined as still in VF/VT after 4th analyze) from other Ottawa hospitals to the Civic ED
- This would result in increase of:
- 13 pt/Year ≈1 pt/Month
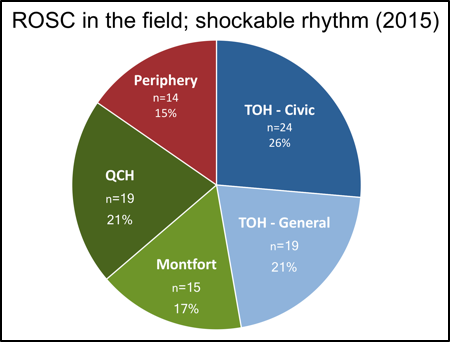
Ottawa hospital destination for field ROSCs with shockable rhythm
Part II: Refractory VF/VT
Treatment options for refractory VF/VT:
- ACLS
- Double sequential defibrillation – feasible in pre-hospital environment but online medical control required
- Beta-blockade (Esmolol) – unavailable in pre-hospital environment
- PCI (?post ROSC) – destination decision integral
- ECMO – destination decision integral
ECMO for Refractory VF/VT
- AHA 2015 Guidelines:
- Insufficient evidence to recommend the routine use. In settings where it can be rapidly implemented, ECPR may be considered for select patients for whom the suspected etiology of the cardiac arrest is potentially reversible (Class IIb, LOE C-LD).
- The number of publications surrounding EMCO for OHCA have increased exponentially
- There are many examples of studies showing promising early results for ECMO in the setting of OHCA
One highly interesting article by Yannopoulos et al. published in J Am Heart Assoc. 2016 titled “Minnesota Resuscitation Consortium’s Advanced Perfusion and Reperfusion Cardiac Life Support Strategy for Out-of-Hospital Refractory Ventricular Fibrillation.” It looked at system changes to treat refractory VF/VT patients
- The idea was to institute a mechanical CPR device and ECMO in order to get the patient to the cath lab for PCI
- Preliminary results of their pre-hospital bypass and ECMO program for refractory ventricular fibrillation during a 3 month trial period (Dec 2015 – Feb 2016) involving 27 patients
- Inclusion criteria were very reasonable and likely similar to what could be applied in a city like Ottawa.
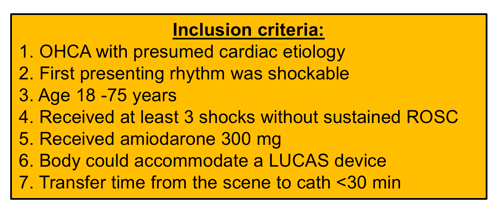
Minnesota inclusion criteria for pre-hospital bypass
- Their results are quite impressive:
- time from 911 to cath lab arrival 60.1 min (+/- 11)
- 78% survived from cath lab and admitted to hospital
- 53% survived to discharge and 1 month
- 50% with CPC 1-2
Ottawa Refractory VF/VT Data
What if the Civic was made into a regionalized cardiac arrest centre?
- One could bypass patients with refractory VF/VT (defined as still in VF/VT after 4th analyze) from other Ottawa hospitals to the Civic ED
- This would result in increase of 13 patients/year ≈1 patient/month
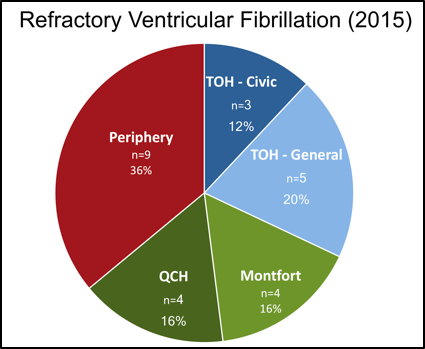
Ottawa hospital destination for refractory VF/VT
Part III: Hypothermic Arrest
- Extracorporeal rewarming provides superior rewarming rates (6-9ºC/hr compared with 0.1-4ºC/hr for other rewarming methods) and also provides cardiac support
- Evidence for extracorporeal Rewarming is based on only multiple case reports or case series
- Expert consensus is that accidental hypothermia patients presenting VSA should be rewarmed with CPB or ECMO
- Supported by AHA guidelines for accidental hypothermia (last updated in 2010)
- Such patients should be transported to facility capable of cardiopulmonary bypass or ECMO
Khorsandi et al. Extracorporeal Life Support for Refractory Cardiac Arrest from Accidental Hypothermia: A 10-Year Experience in Edinburgh. Journal of Emergency Medicine. 2016
- one of the larger case series at a single centre in the UK over a 10 year period (2006-2016)
- 11 patients, all hypothermic cardiac arrests, Mean temp on admission 20.6C
- Recovery scene to extra-corporeal life support = on average, hours
- 9 patients received cardiopulmonary bypass and 2 received VA ECMO
- Survival discharge: 72%; Survival neurologically intact: 54%
Ottawa Hypothermic Cardiac Arrest Data
What if the Ottawa Civic Hospital was made into a regionalized cardiac arrest centre?
- One could bypass patients with accidental hypothermic cardiac arrests from other Ottawa hospitals to the Civic ED
- This would result in increase of 1 patient/year
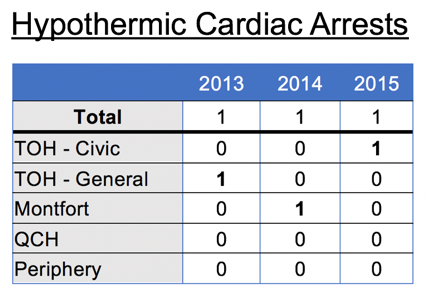
Ottawa Hypothermic Cardiac Arrests
Part IV: Cardiac Arrest – The Future
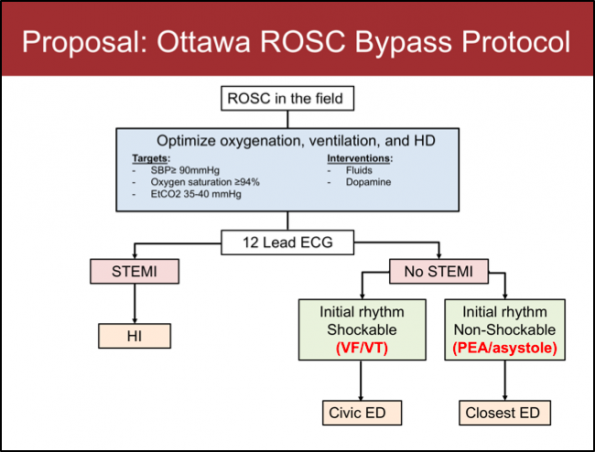
Proposed Ottawa ROSC Bypass Protocol
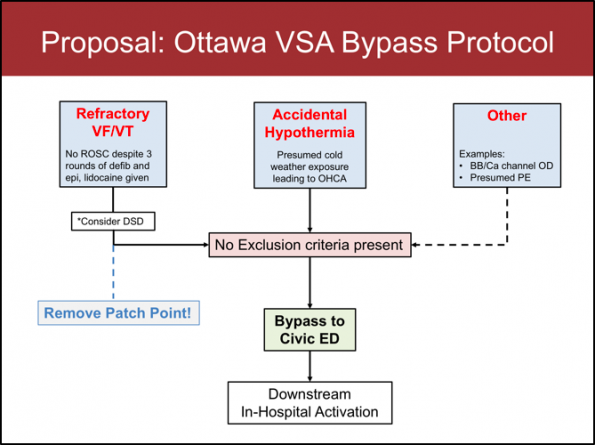
Proposed Ottawa VSA Bypass Protocol
Future issues to be determined
- Drive time criteria: drive time radius that would be included in bypass
- Exclusion criteria: criteria that would exclude patients from VSA transport bypass
- Downstream in-hospital activation: in-hospital downstream effects before/during/after patient arrival
Take home points
- OHCA and ROSC patients deserve specialized, regionalized care
- An obvious start is making modest destination changes
- The face of cardiac arrest care is likely to differ dramatically within the next 5 years – let’s conservatively start to move in that direction!
References:
- Advanced Life Support Patient Care Standards (Version 3.3) Ontario MOH LTC RPPEO Out of hospital cardiac arrest report 2015. Version 1.4: 5/2/2016
- Nolan JP, Neumar RW, Adrie C, et al. Post-cardiac arrest syndrome: Epidemiology, pathophysiology, treatment, and prognostication: A scientific statement from the International Liaison Committee on Resuscitation (Part 1). Int Emerg Nurs. 2009;17(4):203-25.
- Callaway CW, Donnino MW, Fink EL, et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S465-82.
- Schober A, Sterz F, Laggner AN, et al. Admission of out-of-hospital cardiac arrest victims to a high volume cardiac arrest center is linked to improved outcome. Resuscitation. 2016;106:42-8.
- Stub D, Schmicker RH, Anderson ML, et al. Association between hospital post-resuscitative performance and clinical outcomes after out-of-hospital cardiac arrest. Resuscitation. 2015;92:45-52.
- Patterson T, Perkins GD, Joseph J, et al. A Randomised tRial of Expedited transfer to a cardiac arrest centre for non-ST elevation ventricular fibrillation out-of-hospital cardiac arrest: The ARREST pilot randomised trial. Resuscitation. 2017;
- Larsen JM, Ravkilde J. Acute coronary angiography in patients resuscitated from out-of-hospital cardiac arrest–a systematic review and meta-analysis. Resuscitation. 2012;83(12):1427-33.
- Dumas F, Cariou A, Manzo-silberman S, et al. Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest: insights from the PROCAT (Parisian Region Out of hospital Cardiac ArresT) registry. Circ Cardiovasc Interv. 2010;3(3):200-7.
- Hollenbeck RD, Mcpherson JA, Mooney MR, et al. Early cardiac catheterization is associated with improved survival in comatose survivors of cardiac arrest without STEMI. Resuscitation. 2014;85(1):88-95.
- Patel N, Patel NJ, Macon CJ, et al. Trends and Outcomes of Coronary Angiography and Percutaneous Coronary Intervention After Out-of-Hospital Cardiac Arrest Associated With Ventricular Fibrillation or Pulseless Ventricular Tachycardia. JAMA Cardiol. 2016;1(8):890-899.
- Salcido DD, Sundermann ML, Koller AC, Menegazzi JJ. Incidence and outcomes of rearrest following out-of-hospital cardiac arrest. Resuscitation. 2015;86:19-24.
- Spaite DW, Bobrow BJ, Vadeboncoeur TF, et al. The impact of prehospital transport interval on survival in out-of-hospital cardiac arrest: implications for regionalization of post-resuscitation care. Resuscitation. 2008;79(1):61-6.
- Spaite DW, Stiell IG, Bobrow BJ, et al. Effect of transport interval on out-of-hospital cardiac arrest survival in the OPALS study: implications for triaging patients to specialized cardiac arrest centers. Ann Emerg Med. 2009;54(2):248-55.
- Cudnik MT, Schmicker RH, Vaillancourt C, et al. A geospatial assessment of transport distance and survival to discharge in out of hospital cardiac arrest patients: Implications for resuscitation centers. Resuscitation. 2010;81(5):518-23.
- Brooks SC, Anderson ML, Bruder E, et al. Part 6: Alternative Techniques and Ancillary Devices for Cardiopulmonary Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S436-43.
- Stub D, Bernard S, Pellegrino V, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. 2015;86:88-94.
- Dennis M, Mccanny P, D’souza M, et al. Extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest: A multicentre experience. Int J Cardiol. 2017;231:131-136.
- Yannopoulos D, Bartos JA, Martin C, et al. Minnesota Resuscitation Consortium’s Advanced Perfusion and Reperfusion Cardiac Life Support Strategy for Out-of-Hospital Refractory Ventricular Fibrillation. J Am Heart Assoc. 2016;5(6)
- Brown DJ, Brugger H, Boyd J, Paal P. Accidental hypothermia. N Engl J Med. 2012;367(20):1930-8.
- Vanden hoek TL, Morrison LJ, Shuster M, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S829-61.
- Khorsandi M, Dougherty S, Young N, et al. Extracorporeal Life Support for Refractory Cardiac Arrest from Accidental Hypothermia: A 10-Year Experience in Edinburgh. J Emerg Med. 2017;52(2):160-168