Patients who receive solid organ or stem cell transplants are complex, but we see them frequently in the Emergency Department! This review summarizes the physiology of transplant and a few of the key issues to be aware of in these patients.
Transplant by the numbers
- Locally, in Ottawa, there are approximately1:
- 100 renal transplants per year – the transplant clinic follows over 1000 patients
- 25 heart transplants per year – the UOHI follows 350 patients
- 150 hematopoietic stem cell transplants per year
- These are patients who visit the ED frequently2-6:
- In a US study of patients post renal transplant, 12% had visited the ED by 1 month, and 40% by 12 months
- 50-60% of these visits led to hospital admission
- Most common reasons for presentation: fever (35%), abdo pain/GI symptoms (27-31%)7
- Infection is most common reason among transplant patients for admission to hospital8
Physiology of transplant medicine
Renal transplant9-12
- Options: deceased donor or living donor
- Donor kidneys are matched for blood type and HLA classes, and an extensive workup is performed for potential malignancy and latent infection in the donor kidney
- Patients receive intra-op induction therapy, which usually is a combination of a T-lymphocyte depleting agent such as ATG (antithymocyte globulin, aka rabbit-derived anti-T cell antibodies) or an IL-2 receptor antagonist and high-dose corticosteroids
- The kidney is typically placed extra-peritoneally in the iliac fossa, with the renal vessels anastomosed to the external iliac artery and vein and ureter anastomosed to a cystostomy
- Routine for the transplanted ureter to be stented – the stent stays in for first 6 weeks
- Recipients are on lifelong immunosuppression so that the recipient does not reject the donor kidney. The most common combination is:
- Calcineurin inhibitor (tacrolimus or cyclosporine)
- Antimetabolite (mycophenolate or azathioprine)
- Systemic steroids – first high dose, then taper after 4 weeks to dose of approx. 5 mg PO daily
- Risk of rejection is highest in the first several months post-transplant – over years, “host-graft” adaptation occurs in which donor dendritic cells presenting antigens decrease, and host T cells are less responsive to these antigens
- Patients are on antimicrobial prophylaxis short-term to prevent infection; at TOH, this means:
- Septra x 3 months (UTI/PCP prophylaxis)
- Acyclovir or valganciclovir (if CMV mismatch) x 3 months (HSV/CMV prophylaxis)
- No systemic antifungal (as you will see is given for heart and SCT)
Heart transplant13-17
- There are two main techniques for heart transplantation: biatrial and bicaval
- Biatrial: Recipient atria are anastomosed to the donor heart atria – results in irregularly sized/shaped atria
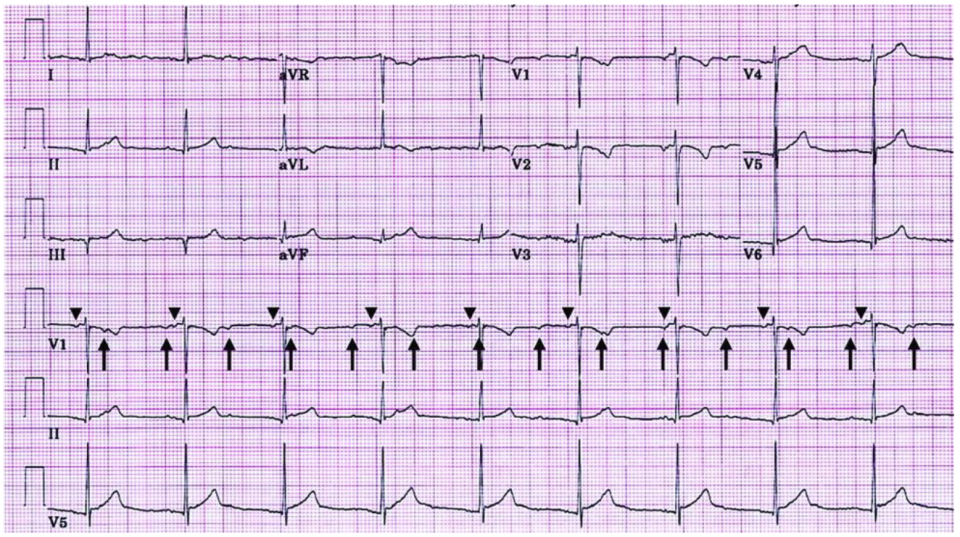
- The recipient SA node is preserved, which is why you may see two distinct p waves on ECG for patients with biatrial orthotopic heart transplant (see below) – typically, the donor SA node impulses are the only ones conducted18
- Bicaval: Recipient RA is excised and the donor RA are anastomosed to the recipient SVC and IVC
- This is thought to result in fewer dysrhythmias
- Donor heart is denervated, which means that the heart has less intrinsic vagal tone
- Transplant recipients’ heart rates are higher as a result, typically around 90-110
- Transplant patients are on lifelong immunosuppression, typically a combination of a calcineurin inhibitor, antimetabolite, and steroids similar to renal transplant patients
- Antimicrobial prophylaxis post heart transplant consists of:
- Septra x 3-6 months
- Itraconazole x 3 months (for prophylaxis of fungal infections including Aspergillus)
- Valacyclovir or acyclovir x 3-6 months, depending on CMV positivity of donor and recipient
Hematopoietic stem cell transplant (HSCT)19-21
- HSCT is performed for a number of indications, including hematologic malignancy (e.g. leukemia, lymphoma, myeloma, etc.) and autoimmune disorders (e.g. multiple sclerosis, stiff person syndrome, etc.)
- Two types of HSCT:
- Autologous (patient’s own stem cells) – avoids risk of graft versus host disease
- Allogeneic (related or unrelated donor, matched for HLA alleles) – has the added benefit of “graft versus tumor” effect for hematologic malignancy where the donor cells attack any remaining cancer cells
- Typical procedure:
- Conditioning: week prior to transplant – high dose chemo (often cyclophosphamide) + total body irradiation to kill cancer cells and recipient bone marrow
- Transplant (day 0): Infusion of stem cells
- Engraftment: typically occurs around 12-30 days
- Immune reconstitution: occurs over weeks-months
- Immunosuppressants: only used in short term, in contrast to solid organ transplant – and weaned around 2-3 months post22
- Antimicrobial prophylaxis:
- Acyclovir 800 BID x 1 year
- Septra 1 tab daily (PCP proph) x 1 year
- Fluconazole x 3 months
- Patients are considered significantly immunosuppressed for the first 6 months at least, even if they have recovered their counts and are off immunosuppressants!
- They need to be re-vaccinated, which starts around 6 months-1 year
- For those patients who live 20-30 years post-transplant, they are felt to have normal or very near-normal immunity, based on clinical study and levels of circulating T cells23
Infection in transplant patients
- Infections look different in the transplant patient because of: 24-26
- Immunosuppression
- Decreased innervation to transplanted organ
- Infections are common: Infection with identified pathogen occurs at rate of 45/100 patient-years within years 1-3 post renal transplant
- Fever is still the most common sign or symptom of infection – it is present in 50% of patients with infection!
- However, consider using a lower temperature as a marker for fever:
- In a prospective study of solid organ transplant patients with documented infection compared with non-transplant patients, transplant patients had a lower Tmax (37.8 vs 38.2) in transplant, as well as lower WBC (11.3 vs 15.4)27
- The types of infections to worry about depend on the timing post-transplant: 28, 29
- 1 month (early): nosocomial, surgical site infection, or donor-derived
- Nosocomial: pneumonia, UTI, device-related infections
- Donor-derived: bacteria resistant to standard antibiotics (MRSA, VRE, TB), fungi (Candida), and parasites (Toxoplasmosis, Trypanosoma)
- 1-6 months (intermediate): opportunistic infection6
- CMV
- Pneumonitis is the most common form, but can be multi-system in presentation (fever, myelosuppression, enterocolitis, encephalitis)
- Highest risk is in patients who are seronegative, who get transplanted CMV positive organs – or in SCT patients, those who are seropositive but receive stem cells from seronegative donor
- Hepatitis B/C
- HSV, VZV, EBV
- PCP
- Fungi: Histo, Coccidioides, Cryptococcus, Aspergillus, Zygomycetes
- CMV
- 6+ months (late): community-acquired infections
- Patients are at elevated risk of community-acquired infections – especially if they have chronic graft rejection and are on aggressive immunosuppression, or if they have immunomodulator related chronic infection (ex CMV, Hep B)
- 1 month (early): nosocomial, surgical site infection, or donor-derived
Take Home Points for patients with potential infection in the ED:
- Lower threshold for fever/WBC to make you think infection
- Microbiological diagnosis is key in this group – more invasive testing (bronch, tissue biopsy, etc.) often done to identify a pathogen
- Antibiotic choices:
- Keep broad-spectrum in ED
- Antifungal therapy rarely indicated in ED
UTIs in renal transplant 31-34
- UTI is the most common source of sepsis in renal transplant patients, and UTI will occur in up to 20% of renal transplant patients at 1 year
- Frequent UTIs can lead to decreased graft survival
- Most common bacteria in UTI for patients post renal transplant: E. coli (60%), E. faecalis (12%), Enterobacter, Pseudomonas, CoNS
- Look at previous cultures when prescribing antibiotics for patients with suspected UTI – pip-tazo/vanco (or ceftriaxone/ampicillin) will not cover ESBL organisms!
- Studies in transplant patients show incidence of 15-28% ESBL UTIs
- There is also significant E. coli resistance to ciprofloxacin in transplant population
- Ceftriaxone as single agent has zero Enterococcus coverage
- Continue to refer to our local protocols for UTI – there isn’t enough data to indicate when we should deviate from standard practice for these patients with UTI
- Length of treatment: 7-10 days (considered “complicated”)
- What to do with asymptomatic bacteriuria?
- Common in renal transplant patients: 51% incidence of asymptomatic bacteriuria in renal transplant patients by 3 years
- Limited, small studies have failed to show benefit (in the form of reduced UTI or maintenance of renal function) in treating asymptomatic bacteriuria in KTRs
- There are ongoing trials to assess whether there is a role for antibiotics, but in the interim, our local practice is to not treat asymptomatic bacteriuria except in the first 6 weeks when patients have ureteric stents
Dysrhythmias in transplant patients 35-39
-
- In transplants, the donor heart sympathetic and parasympathetic nerves are severed, so vagal tone is lost
- Patients maintain responsiveness at beta receptors and may have upregulation of these receptors
- They rely on circulating catecholamines to raise their heart rate with exercise
- The donor heart is very sensitive to sympathomimetics
- Dysrhythmias are common, but typically transient and in post-op period due to trauma or edema
- In patients who present with bradycardia, atropine will not be effective, but beta-agonists and temporary pacing will still have an effect
- Tachycardia:
- Vagal maneuvers will not be effective
- For rate control, beta blockers preferred over calcium channel blockers due to interactions of CCB with calcineurin inhibitors
- Patients are exquisitely sensitive to adenosine – consider using a lower dose
- In an EP study comparing adenosine effects in transplanted vs native hearts, all transplant patients responded to the lowest dose adenosine, and the duration of AV node slowing was approx. 4x longer in the transplanted hearts!39
- Cardioversion is still indicated for unstable dysrhythmias
- For patients with new dysrhythmias after post-transplant period, think about the cause: sepsis, rejection, and ischemia should be at the top of your differential
- CAV – cardiac allograft vasculopathy40
- This is accelerated atherosclerosis in transplanted hearts – occurs in 1/3 of patients after 5 years to some degree40
- Because the heart is denervated, patients may not have any chest pain when they present with ischemia
- In transplants, the donor heart sympathetic and parasympathetic nerves are severed, so vagal tone is lost
HSCT pearls 41, 42
- Immunizations not started until 1 year post SCT – immune competence generally not thought to occur until 2 years post
- Respiratory symptoms in the BMT patient
- Lung infection is the most common documented infection in BMT patients
- Diagnosis of a pathogen is key (whether bacterial or viral)
- When presenting with respiratory symptoms: send sputum, respiratory virus panel, influenza swab
- Diarrhea in the BMT patient
- Differential is wide, and includes:
- Infectious enteritis/colitis: C. difficile, viral infections, Strongyloides, Cryptosporidium, Giardia, bacterial causes, neutropenic enterocolitis
- Non-infectious: GVHD
- T lymphocytes of donor graft attack recipient tissue (due to antigenic differences between donor/host MHC)
- Can present with rash, diarrhea, abdo pain, cholestasis, transaminitis
- Treated with immunosuppressants – which modifies patient risk for infection
- For the BMT patient with diarrhea/abdominal pain, consider performing more testing than for your standard patient, including stool C. diff assay, O+P, culture
- Differential is wide, and includes:
Medications used in solid organ transplant 43, 44
Calcineurin inhibitors
- Aka cyclosporine and tacrolimus
- Interfere with intracellular signaling and IL-2 release (needed for proliferation of cytotoxic T cells)
- Dosing based on pre-dose trough levels – so a random level in the ED is not helpful
- Toxicities:
- Nephrotoxicity
- Neurotoxicity – seizure, headache, tremor
- Hypertension – including hypertensive crisis, PRES
- Some of the drugs that we give that will interact with the P450 system and increase the levels of calcineurin inhibitors:
- Calcium channel blockers
- Amiodarone
- Aminoglycosides
- Macrolides – consider substituting a non-macrolide antibiotic
- Antifungals
Mycophenolate
- Prodrug that releases mycophenolic acid, which inhibits synthesis of purines – which are required for proliferation of lymphocytes
- Toxicities: Mostly GI (diarrhea), neutropenia, anemia
- No blood level monitoring
Take Home Points:
- Maintain a high level of suspicion for infection in the post-transplant patient
- Infection types depend on timing post-transplant
- Look at previous cultures and cover for resistant organisms if known
- UTI in renal transplant: consider Enterococcus coverage, cover for ESBL if prior ESBL UTIs, and do not treat asymptomatic bacteriuria except if indwelling ureteric stent
- Dysrhythmias in heart transplant: cardioversion and beta blockers are safe; judicious dosing of adenosine and catecholamines
- Consider the cause of dysrhythmia including ischemia, rejection, sepsis
- HSCT patients: high risk for infections, even if counts are normal – think about more extensive testing for infection in this group
- Work with our colleagues in transplant who have extensive experience with these patients!
References
- Trilium Gift of Life Network. Breaking Through: Trillium Annual Report 2016/2017. (2017). doi:10.1021/cen-09227-bus2
- Schold, J. D. et al. Emergency Department Visits after Kidney Transplantation. Clin. J. Am. Soc. Nephrol. 11, 674–683 (2016).
- Trzeciak, S. et al. Infections and severe sepsis in solid-organ transplant patients admitted from a university-based ED. Am. J. Emerg. Med. 22, 530–533 (2004).
- Venkat, K. K. & Venkat, A. Care of the renal transplant recipient in the emergency department. Ann. Emerg. Med. 44, 330–341 (2004).
- Ergin, M., Dal, U., Granit, D., Aslay, S. & Selhanoglu, M. Management of Renal Transplant Patients in the Emergency Department. J. Acad. Emerg. Med. 14, 83–87 (2015).
- Unterman, S. et al. A descriptive analysis of 1251 solid organ transplant visits to the emergency department. West. J. Emerg. Med. 10, 48–54 (2009).
- Uysal, E. et al. The Reasons of Renal Transplant Recipients’ Admission to the Emergency Department; a Case Series Study. Emergency 4, 207–210 (2016).
- Jones, A. E., Trzeciak, S. & Kline, J. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at time of emergency department presentation. Crit. Care Med. 37, 1649–1654 (2009).
- Gritsch, H. A. & Blumberg, J. M. in Campbell-Walsh Urology 1069–1088.e2 (Elsevier Inc., 2011). doi:10.1016/B978-1-4557-7567-5.00047-9
- Pham, P.-T., Danovitch, G. M. & Pham, P.-C. T. Chapter 105: Medical Management of the Kidney Transplant Recipient: Infections, Malignant Neoplasms, and Gastrointestinal Disorders. Comprehensive Clinical Nephrology, 5/e (Elsevier Inc., 2015). doi:10.1016/B978-1-4557-5838-8.00105-2
- Barlow, A. D. & Nicholson, M. L. Chapter 103: Kidney Transplantation Surgery. Comprehensive Clinical Nephrology, 5/e (Elsevier Inc., 2015). doi:10.1016/B978-1-4557-5838-8.00103-9
- Halloran, P. F. Immunosuppressive drugs for kidney transplantation. N. Engl. J. Med. 351, 2715–2729 (2004).
- Lindenfeld, J. Drug Therapy in the Heart Transplant Recipient: Part I: Cardiac Rejection and Immunosuppressive Drugs. Circulation 110, 3734–3740 (2004).
- Hunt, S. A. Taking Heart — Cardiac Transplantation. N. Engl. J. Med. 355, 231–235 (2006).
- John, R. & Liao, K. Orthotopic heart transplantation. Oper. Tech. Thorac. Cardiovasc. Surg. 15, 138–146 (2010).
- Lindenfeld, J. Drug Therapy in the Heart Transplant Recipient: Part II: Immunosuppressive Drugs. Circulation 110, 3858–3865 (2004).
- Costanzo, M. R. et al. The international society of heart and lung transplantation guidelines for the care of heart transplant recipients. J. Hear. Lung Transplant. 29, 914–956 (2010).
- Cooper, JA, Saeed IM, et al. Lost P’s, but not yet forgotten. Circulation 115, e41-42 (2007).
- Heslop, H. E. in Hematology 1591–1595 (Elsevier Inc., 2018). doi:10.1016/B978-0-323-35762-3.00103-7
- Holtan, S. G., Majhail, N. S. & Weisdorf, D. J. in Hematology 1669–1684.e2 (Elsevier Inc., 2018). doi:10.1016/B978-0-323-35762-3.00109-8
- Léger, C. S. & Nevill, T. J. Hematopoietic stem cell transplantation: a primer for the primary care physician. CMAJ 170, 1569–77 (2004).
- Bouchlaka, M. M. N., Redelman, D. & Murphy, W. J. W. Immunotherapy following hematopoietic stem cell transplantation: potential for synergistic effects. Immunotherapy 2, 399–418 (2010).
- Storek, J. et al. Immunity of patients surviving 20 to 30 years after allogeneic or syngeneic bone marrow transplantation. Blood 98, 3505–3513 (2001).
- Kalil, A. C. et al. Is bacteremic sepsis associated with higher mortality in transplant recipients than in nontransplant patients? a matched case-control propensity-adjusted study. Clin. Infect. Dis. 60, 216–222 (2015).
- Snyder, J. J. et al. Rates of first infection following kidney transplant in the United States. Kidney Int. 75, 317–326 (2009).
- Sawyer, R. G., Crabtree, T. D., Gleason, T. G., Antevil, J. L. & Pruett, T. L. Impact of solid organ transplantation and immunosuppression on fever, leukocytosis, and physiologic response during bacterial and fungal infections. Clin. Transplant. 13, 260–5 (1999).
- Pelletier, S. J. et al. Characteristics of infectious complications associated with mortality after solid organ transplantation. Clin. Transplant. 14, 401–8 (2000).
- Fishman, J. A. Infection in Solid-Organ Transplant Recipients. New Engl. J. Med. 357, 2601–2614 (2007).
- O’Shea, D. T. & Humar, A. Life-threatening infection in transplant recipients. Crit. Care Clin. 29, 953–973 (2013).
- Coussement, J. & Abramowicz, D. Should we treat asymptomatic bacteriuria after renal transplantation? Nephrol. Dial. Transplant. 29, 260–262 (2014).
- Kotagiri, P., Chembolli, D., Ryan, J., Hughes, P. D. & Toussaint, N. D. Urinary Tract Infections in the First Year Post–Kidney Transplantation: Potential Benefits of Treating Asymptomatic Bacteriuria. Transplant. Proc. 49, 2070–2075 (2017).
- Fiorante, S. et al. Systematic screening and treatment of asymptomatic bacteriuria in renal transplant recipients. Kidney Int. 78, 774–781 (2010).
- Kasiske, B., Zeier, M. & Craig, J. KDIGO clinical practice guideline for the care of kidney transplant recipients. … Transplant. … (2009).
- Nicolle, L. E. et al. Infectious diseases society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin. Infect. Dis. 40, 643–654 (2005)
- Birati, E. Y. & Rame, J. E. Post-heart transplant complications. Crit. Care Clin. 30, 629–637 (2014).
- Cannom, D., Rider, A. K., Stinson, E. B. & Harrison, D. C. Electrophysiologic Studies in the Denervated Transplanted Human Heart. Am. J. Cardiol. 36, 859–866 (1975).
- Awad, M. et al. Early denervation and later reinnervation of the heart following cardiac transplantation: A review. J. Am. Heart Assoc. 5, 1–22 (2016).
- Thajudeen, A. et al. Arrhythmias After Heart Transplantation: Mechanisms and Management. J. Am. Heart Assoc. 1, e001461–e001461 (2012).
- Ellenbogen, K. A., Thames, M. D., DiMarco, J. P., Sheehan, H. & Lerman, B. B. Electrophysiological effects of adenosine in the transplanted human heart. Circulation 81, 821–828 (1990).
- Birati, E. Y. & Rame, J. E. Post-heart transplant complications. Crit. Care Clin. 30, 629–637 (2014)
- Adelberg, D. E. & Bishop, M. R. Emergencies Related to Cancer Chemotherapy and Hematopoietic Stem Cell Transplantation. Emerg. Med. Clin. North Am. 27, 311–331 (2009).
- Afessa, B. & Azoulay, E. Critical Care of the Hematopoietic Stem Cell Transplant Recipient. Crit. Care Clin. 26, 133–150 (2010).
- BC Renal Agency. Major drug interactions with cyclosporine and tacrolimus. (2016).
- Trofe-Clark, J, and Lemonovich T. Interactions between anti-infective agents and immunosuppressants in solid organ transplantation. American Journal of Transplantation 13, 318-326. (2013).




