It is not uncommon to see patients present to the Emergency Department with Hypertension. One in 4 Canadians has a diagnosis of hypertension, and chronic hypertension is the leading cause of disability-adjusted life expectancy (which considers for the quality of life to be comprised of a composite of mortality, institutionalization, and limitations on activities of daily living).
Hypertensive emergencies are a heterogeneous group of acute hypertensive disorders that need rapid diagnosis and appropriate therapy. Many of these emergencies, such as pre-eclampsia, eclampsia, ACS, acute ischemic stroke, ICH, and acute aortic syndrome have specific treatments and targets. These are discussed readily in medical literature, and academics at various stages of training. However, there are a few hypertensive emergencies that are more subtle to identify, but important as patients may benefit from prompt urgent treatment. This review will focus on these more subtle cases, more specifically hypertensive retinopathy, nephropathy, and encephalopathy. We will aim to guide the development of an approach to the assessment of the acutely hypertensive patient, to better identify patients requiring urgent treatment, and those who can be referred for outpatient management.
Hypertension in the Emergency Department
Hypertension alone is a relatively common presentation to emergency departments. Astarita and colleagues published a systematic review showing that 0.3-0.9% of presentations to the emergency department are for hypertensive urgencies and emergencies (1). What prompts these patients to present to the ED? Are they referred? Or are they symptomatic? An observational study looking at patients presenting to the emergency department with hypertension in Ontario, Canada found that the referral source for these patients was home readings (41%), a physician referral (13%), pharmacy referral (8%) and unknown (38%) (2).
Hypertensive Emergencies
Hypertensive emergencies are a group of heterogeneous acute hypertensive disorders that need rapid diagnosis and treatment. At present, there are 3 main guidelines that offer us a definition.
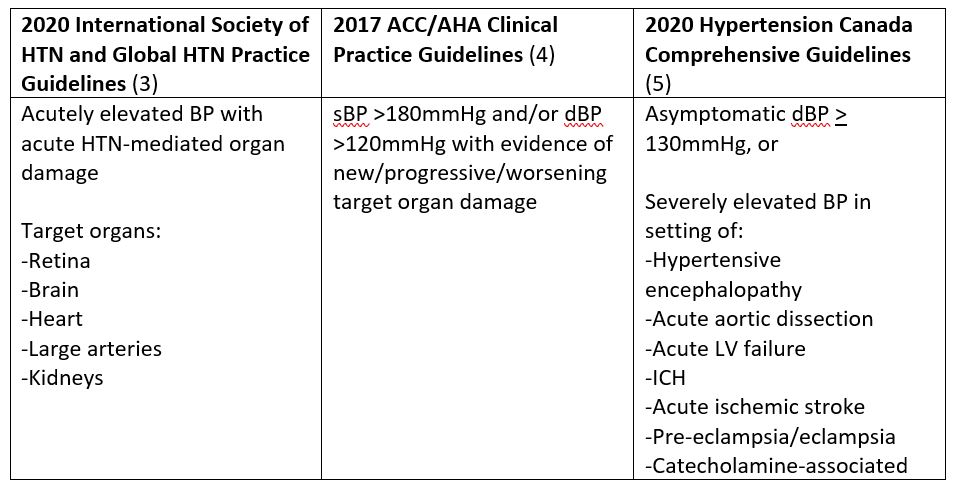
From the above, hypertensive emergencies can be simplified to:
-
-
- Severe hypertension (most commonly sBP > 180 and/or dBP > 120-130), and
- Evidence of acute or worsening end-organ damage
-
Patients who lack acute hypertension-mediated end-organ damage do not have a hypertensive emergency and simply have uncontrolled hypertension. Note that, the term “hypertensive urgency” is just uncontrolled hypertension and NOT an entity on its own.
As previously stated, the focus of this review is to look at the more subtle cases of hypertensive emergencies comprised of hypertensive retinopathy, nephropathy, and encephalopathy. These cases can be in the “grey” zone and could easily be missed but would benefit from urgent treatment.
Hypertensive Retinopathy
Fundoscopy is an extremely important examination technique in an otherwise asymptomatic severely hypertensive patient as findings act as a gateway for so much information. The European Society of Cardiology defines hypertensive emergencies as severe blood pressure elevation with advanced retinopathy (6), and this alone is an indication for acute treatment. In the emergency department setting increasing accuracy and confidence with optic disc assessment can be attained by using the PanOptic ophthalmoscopy. Pertruskin, et al studied the panoptic use in the emergency department and found that with a short intervention resident physicians with no previous experience using PanOptic were able to double their sensitivity to finding abnormal discs compared to direct ophthalmoscopy (7).
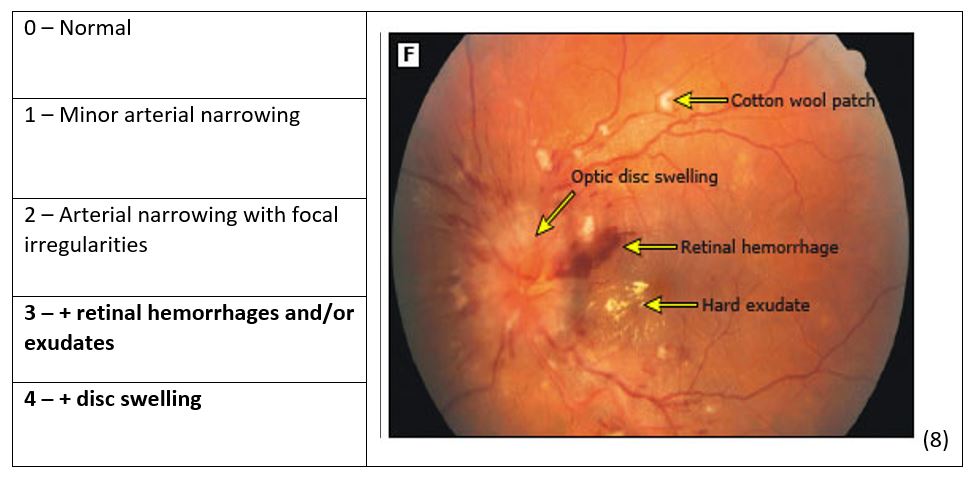
Grade III and IV changes on fundoscopy carry the same prognosis and can be stratified together and when these findings are present bilaterally they are highly specific for a hypertensive emergency (7).
Tips to panoptic use:
-
-
- Lights off
- Smallest pinhole possible
- Get close
- Follow the vessel
-
As papilledema is the only feature to distinguish Grade III versus IV changes PoCUS could be considered as it is non-invasive and it can also be used in obtunded patients. There are limitations to PoCUS to look for papilledema including false positives from things such as optic drusens (calcium in the disc) and inflammatory disorders such as sarcoidosis and optic neuritis. These false positives are often unilateral therefore if you choose to do PoCUS you should always measure both eyes.
Technique for PoCUS to measure optic sheath diameter
-
-
- High-frequency linear probe
- Transverse orientation
- Measure 3mm behind the globe
- Measure outer wall to outer wall of the optic sheath
-
Take Home Points
-
-
- Fundoscopic examination is essential in the assessment of the hypertensive patient as it acts as a gateway for further assessment
- Acute/severe hypertensive retinopathy includes hemorrhages, exudates, and papilledema
- If you find severe retinal changes you should consider lowering BP acutely and doing further screening for other signs of end-organ dysfunction
- PoCUS shouldn’t replace fundoscopy when looking for hypertensive changes however it may add value in the patient where exudates and hemorrhages are visible but you are unsure about papilledema or in the obtunded patient.
-
Hypertensive Nephropathy
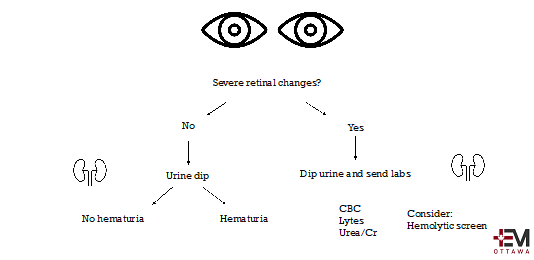
All the major guidelines identify an acute or rapidly declining renal function as a sign of end-organ dysfunction that indicates a possible hypertensive emergency. Systemic microvascular damage is the hallmark of severe, or sometimes known as malignant, hypertension (6). Hematuria, which is usually microscopic, can be found in up to 75% of patients with hypertensive emergencies (6). This is why considering screening with a urine dip is important in the severely hypertensive patient who is otherwise asymptomatic without another identifiable cause or trigger. If a patient does have hematuria and a newly elevated creatinine with severely elevated BP then they are having a hypertensive emergency.
Suggested Approach:
Hypertensive Encephalopathy
Another more subtle presentation of hypertensive emergency is the case of hypertensive encephalopathy. This section will cover the case of the severely hypertensive patient who presents without focal neurological deficit but is altered.
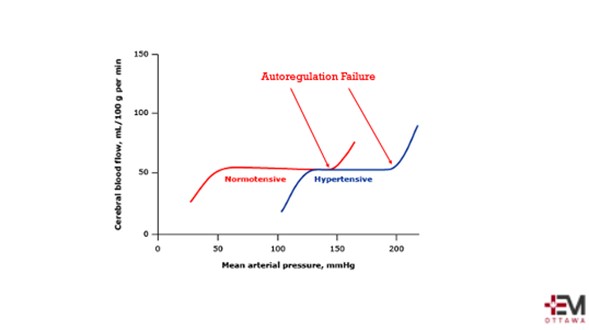
Our brains are under tight control. With severe rises in BP, autoregulation fails and leads to cerebral edema. The actual number at which autoregulation failure occurs depends on a patient’s background and previous history of hypertension. This narrow range of autoregulation contributes to why acutely lowering BP can be dangerous when not clinically indicated.
Hypertensive encephalopathy is defined as the presence of signs or symptoms of cerebral edema secondary to severe and/or sudden rises in BP. It’s characterized by:
Severe Hypertension with 1+ of:
- Seizures
- Lethargy
- Cortical Blindness
- Coma
It is a diagnosis of exclusion, often confirmed after the mental status improves with lowering the BP into the autoregulation range. Risk factors included medical comorbidities including TTP, vasculitis, sepsis and bone marrow transplant, medications such as cyclosporine, IVIG and chemotherapeutic agents. It is a diagnosis that needs a high index of suspicion and should be considered in the workup of the altered patient. The management includes lowering the MAP 10-15% in the first hour with IV labetalol as both a diagnostic and management option.
Of note, there is little evidence to suggest that headache alone is a sign of a hypertensive emergency, however, in combination with visual changes, lethargy, seizures or altered mental status it may be an indication of hypertensive encephalopathy.
To Treat or Not To Treat

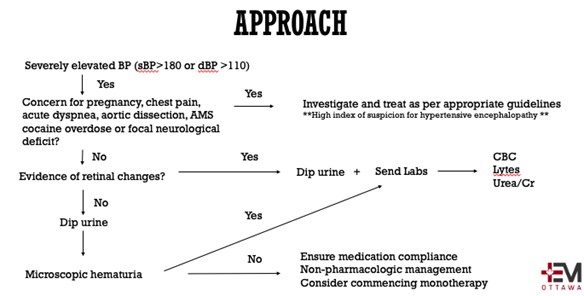
Approach
Approach to the asymptomatic severely hypertensive patient:
-
-
- Do they have a known history of HTN?
- If so, when was the last time they had their BP checked outside of this acute scenario? This will give you a baseline to screen for potential acuity
- How compliant are they with their medications?
- History of recent triggers most with the most common culprits being: Salt, EtOH, NSAIDs, steroids and decongestant cough/cold medications
- Systems review looking for symptoms of hypertensive emergency
- Screen for pregnancy in the appropriate population
- Examine the patient including fundoscopy and urine dip
-
Basic Principles to commencing antihypertensive therapies:
-
-
- If there is no target end-organ damage it is NOT a hypertensive emergency!!!
- Do not lower the BP too quickly as there is a risk of ischemic damage to vascular beds (exceptions for acute ischemic or hemorrhagic stroke, aortic dissection, ICH, and pre-eclampsia)
- ACEP and AHA/ACC recommend against decreasing asymptomatic BP with IV agents
-
ACEP 2013 guidelines recommend against routine screening of asymptomatic hypertensive patients however they do say that select patients would benefit from screening (Level C Recommendation) (11). Patients with severe asymptomatic hypertension with BP > 180/110 without other confounders such as pain, anxiety, or substance misuse, have a diagnosis of hypertension and this does need long-term management to decrease morbidity. These patients need to be approached in a systematic way. As per discussion around hypertensive emergency diagnosis, fundoscopy and urine dip should be considered part of our physical exam in patients with severe hypertension and should always be considered.
When looking at commencing antihypertensives there is a risk of harm most commonly seen in the inpatient setting where intensification of medication on discharge in hypertensive patients has been shown to lead to more adverse events such as AKI, myocardial injury and falls (12, 13).
Treatment Options
Behaviour modification
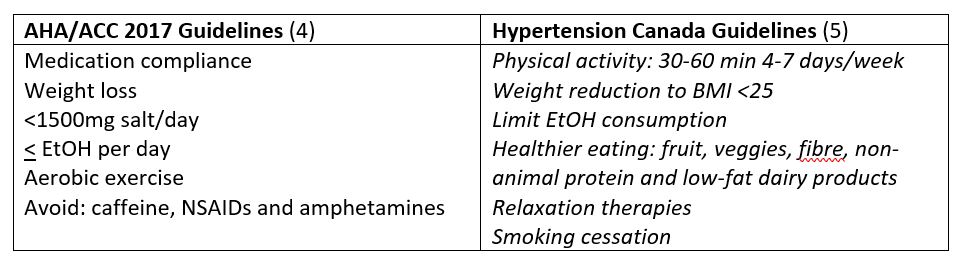
Oral Therapy
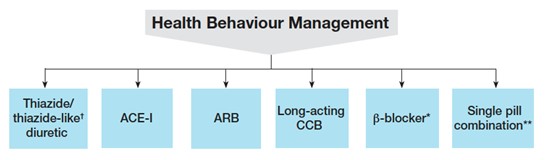
Hypertension Canada suggests a wide variety of choices for starting antihypertensives. In the case of diastolic HTN with or without systolic HTN or isolated systolic HTN first-line agents include thiazides, ARB and long-acting CCB. In an emergency department setting, CCB may be the most reasonable agent as it requires little follow-up blood work. It also is first-line across most comorbidities outside of MI/CHF/TIA/remote stroke. Additionally, prescribing a BP cuff for a patient in addition to monotherapy would be appropriate. These patients can then be titrated in the community by their primary care physician.
Take-Home Points
-
-
- Fundoscopy and urine dip are key in the assessment of the severely hypertensive patient who you are working up for a possible hypertensive emergency
- Keep a high index of suspicion for hypertensive encephalopathy in the severely hypertensive and altered or comatose patient with or without seizures or cortical blindness
- Treat the patient and not the number
- Understand the potential risk of harm in starting antihypertensives but if you do:
- Start low and go slow
- CCB is a reasonable choice for monotherapy from the emergency department
- Arrange follow-up within 1-2 weeks
-
References
-
-
- Astarita A, Covella M, Vallelonga F, Cesareo M, Totaro S, Ventre L, Apra F, Milan A. Hypertensive emergencies and urgencies in emergency departments: a systematic review and meta-analysis. J Hypertens. 2020 Jul; 38(7): 1203-1210.
- Atzema C, Wong A, Masood S, Zia A, Al-Bulushi S, Sohail Q, Cherry A, Chan F. The characteristics and outcomes of patients who make an emergency department visit for hypertension after use of a home or pharmacy blood pressure device. Ann Emerg Med. 2018 Nov; 72(5): 534-543.
- Unger T, Borghi C, Charchar F, Khan N, Poulter N, Prabhakaran D, Ramirez A, Schlalch M, Sterglou G, Tomaszewski M, Wainford R, Willians B, Schutte A. 2020 International Society of Hypertension and Global Hypertension Practice Guidelines. Hypertension. 2020 Jun; 75(6): 1334-1357.
- Whelton, P, Carey R, Aronow W, Casey Jr D, Collins K, Dennison Himmelfarb C, Depalma S, Gidding S, Jamerson K, Jones D, MacLaughlin E, Munter P, Ovbiagele B, Smith Jr S, Spencer C, Stafford R, Taler S, Thomas R, Williams Sr K, Williamson J, Wright Jr J. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults: A Report for the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018 Jun; 71(6) e13-115.
- Rabi D, McBrien K, Sapir-Pchhadze R, Nakhla M, Ahmed S, Dumanski S, Butalia S, Leung A, Harris K, Cloutier L, Zarnke K, Ruzicka M, Hiremath S, Feldman R, Tobe S, Campbell T, Bacon S, Nerenber K, Dresser G, Fournier A, Burgess E, Lindsay P, Rabkin S, Prebtani A, Grover S, Honos G, Alfonsi J, Arcand J, Audibert F, Benoit G, Bittman J, Bolli P, Cote A, Dionne J, Don-Wauchope A, Edwards C, Firoz T, Gabor J, Gilbert R, Gregoire J, Gryn S, Gupta M, Hannah-Shmouni F, Hegele R, Herman R, Hill M, Howlett J, Hundemer G, Jones C, Kaczorowski J, Khan N, Kuyper L, Lamarre-Cliché M, Lavoie K, Leiter L, Lewanczuk R, Logan A, Magee K, Leiter L, Lewanczuk R, Logan A, Magee L, Mangat B, McFarlane P, McLean D, Michaud A, Milot A, Moe G, Penner S, Schiffrin E, Shelby P, Sharma M, Shoamanesh A, Sivapalan P, Townsend R, Tran K, Trudeau L, Tsuyuki R, Vallee M, Woo V, Bell A, Daskalopoulou S. Hypertension Canada’s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children. Can J Cardiol. 2020 May; 36(5): 596-624.
- Van den Born J, Lip G, Brguljan-Hitij J, Cremer A, Segura J, Morales E, Mahfoud F, Amraoui F, Persu A, Kahan T, Rosei E, de Simone G, Gosse P, Williams B. ESC Council on hypertension position document on the management of hypertensive emergencies. European Heart Journal – Cardiovascular Pharmacotherapy. 2019 Jan; 5(1); 37-46.
- Petrushkin H, Barsam A, Mavrakakis M, Parfitt A, Jaye P. Optic disc assessment in the emergency department: a comparative study between the PanOptic and direct opthalmoscopes. Emerg Med J. 2012 Dec; 29 (12): 1007-8.
- Downie LE, Hodgson LA, Dsylva C, et al. Hypertensive retinopathy: Comparing the Keith-Wagener-Barker to a simplified classification. J Hypertens 2013; 31:960
- Kaplan NM. Management of hypertensive emergencies. Lancet 1994; 344:1335
- Patel K, Young L, Howell E, Hu B, Rutecki G, Thomas G, Rothberg M. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern Med. 2016 Jul; 176(7): 981-8.
- Wolf S, Lo B, Shih R, Smith M, Fesmire F. ACEP Clinical Policy: Critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med. 2013; 62:59-68.
- Anderson T, Jing B, Auerbach A, Wray C, Lee S, Boscardin W, Fung K, Ngo S, Silvestrini M, Steinman M. Clinical outcomes after intensifying antihypertensive medication regimens among older adults at hospital discharge.
- Rastogi R, Sheehan M, Hu B, Shaker V, Kojima L, Rothber M. Treatment and outcomes of inpatient hypertension among adults with noncardiac admissions. JAMA Intern Med. 2021 Mar; 181(3): 345-352.
-



