We’re back this week with some new pediatric content — Managing Pediatric GERD!
Check out our recent peds post on managing pediatric agitation here.
Reflux disease is often considered as a common etiology for infants presenting with vomiting and perceived discomfort or fussiness. This leads to parents commonly seeking medical attention in both the emergency department and family medicine settings.
So what is GERD?
Gastroesophageal reflux (GER) is defined as the passage of gastric contents into the esophagus, which occurs physiologically every day in all humans. Gastroesophageal reflux disease (GERD) is defined as GER + “troublesome symptoms” or “symptoms severe enough to merit medical attention”.1 As you can imagine, this diagnosis relies heavily on a detailed history that fits with the classic presentation of “heart burn” or “chest pain” that is worse at night when laying flat and occurs after eating large meals or eating late at night. In our non-verbal pediatric patients, this diagnosis can be difficult to make and apply to infants whose troublesome symptoms are solely being described by their caregiver. Symptoms are commonly described as recurrent vomiting or regurgitation, choking, coughing, perceived discomfort or sleep interruption.1
Unfortunately, the diagnosis of GERD in an infant really is a clinical one, given the current evidence that shows barium imaging, ultrasound, and biomarkers are not helpful in making this diagnosis. Additionally, specialized testing such as endoscopy, manometry, scintigraphy, and therapeutic trials of post pyloric feeds are specifically reserved for complicated cases.1,2 A specific GERD questionnaire has been validated but is not always practical for use in a busy emergency department.3
As an ED physician, we must have an approach to considering alternative diagnoses so we don’t miss sinister causes of similar presentations. In the absence of alternative causes to account for the patient’s symptoms, we can recommend initial management to parents as they await follow up with their PCP.
This brings us to the objectives of this post:
- Review the red flag signs/symptoms of infants presenting with vomiting
- Provide evidence-based management suggestions for suspected GERD in infants
What red flags should you watch out for?
The presence of red flag features listed below may suggest alternative diagnoses and prompt further investigation or consultation with a pediatric specialist1,2:

- General: weight loss or failure to thrive (FTT), lethargy, fever, excessive irritability or pain
- Timing: onset >6months of age or persistence of symptoms >12-18 months
- Neurological: bulging fontanelle, macro or microcephaly, seizures
- Gastrointestinal: bilious emesis, forceful/projectile vomiting, hematemesis, diarrhea/hematochezia, abdominal distension
A note about atopy…
An astute physician may also consider asking about a strong family/personal history of atopy, eczema, seasonal allergies, or anaphylaxis. Food protein induced proctocolitis, formally referred to as cow’s milk protein allergy, can sometimes present with symptoms indistinguishable from GERD in an infant without noted blood in the stool.2 While more common in children of parents with atopy, the absence of family history does not preclude this as a possibility. A trial of milk-protein free foods is typically part of the recommended management algorithm for infants with suspected GERD.4
What if I’m pretty sure this infant has GERD — how can I advise their family?
GERD management in infants has been the focus of research for over 30 years — resulting in modified practical approaches and a relatively recent practice guideline being published in 2018 by the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition.1
Let’s review the possible yet common discussion points you may encounter when discharging patients home with worried parents.
Positioning recommendations:
While there is some evidence that left lateral decubitus positioning reduces reflux events in infants5,6, adjusting sleeping positioning for infants increases the risk of SIDS so the bottom line recommendation is to discourage inclined sleeping surfaces and continue safe sleeping practice recommendations in infants with GERD. This includes recommending a clutter-free, flat, sleeping surface with the infant placed on their back.
Though no specific research trials have investigated the effect of holding an infant upright for 20-30 minutes following a feed, this has been a common practice recommendation. Many practitioners recognize that frequently feeding infants can sometimes place unrealistic expectations on parents and lead to unsafe situations — such as a parent falling asleep with an infant in their arms. If you do discuss this recommendation with parents, ensure that the parent knows the infant should be held upright in their arms / in a baby wearer and NOT PLACED in a seated position, such as a swing or carseat, as forward flexion can worsen reflux!
Feed thickening:
In 2018, a systematic review & meta-analysis in Pediatrics reviewed 15 RCTs looking at the use of thickened feeds for management of GERD.7
- overall conclusions: thickened feeds significantly increased the proportion of infants without regurgitation (NNT=6) and increased daily weight gain.
- The effect on symptoms of regurgitation were not statistically significant in terms of improving frequency of reflux events.
- If considering feed thickening in infants, the practitioner should be aware that there is an increased risk of NEC in preterm infants so utilize with caution.
Take home point: The expert opinion recommendation is to consider a trial of thickened feeds in infants whose parents report visible regurgitation.1
Probiotics:
- Studies performed in healthy term infants who were given lactobacillus demonstrated a significant reduction in crying time and regurgitation frequency without any safety issues identified.8
- Due to insufficient evidence, experts do not recommend the routine use of probiotics for infants with GERD1
- A caveat to this suggestion is clinicians may practically counsel and undergo shared decision making with parents regarding the little risk of harm to the infant and a potential for benefit in utilizing probiotics.
Acid suppression with PPI or H2RA:
Did you know that 85% of reflux in infants is non-acidic? An infant’s frequent feeding with alkaline milk effectively buffers stomach contents which calls into question the utility of acid-suppressing medications in managing infantile reflux.
- Several studies have found no significant differences between placebo controlled studies looking at PPI use.10–13
- No studies have investigated the use of H2RAs in infants <6 months of age for GERD.1
- 2019 retrospective study looked at >800,000 children exposed to acid suppressive therapy <12 months old & concluded that there was a hazard ratio of 1.23 with PPI exposure and 1.31 with PPI + H2RA exposure for childhood fractures.
- Due to this growing body of evidence and concerns for safety, a judicious approach to acid-suppressive therapy prescriptions is recommended
- Acid suppression therapy should only be considered for a distinct, time-limited therapeutic trial & be stopped if no symptom improvement.1
So what should I specifically recommend for my patient then?
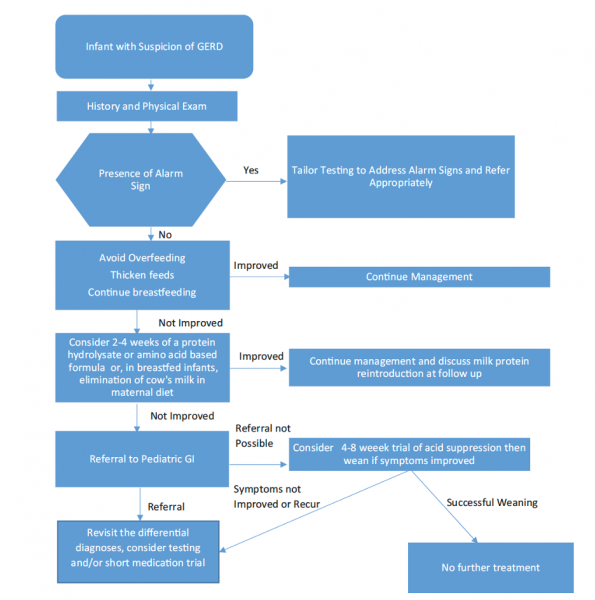
Now that you have been reminded & updated on some of the important evidence around treatment options for reflux, you should be well-equipped to utilize the expert recommended algorithm below when approaching the vomiting infant with suspected GERD in the ED.
Your specific recommendations will depend on what the family has already tried or is willing to explore. Some helpful infant feeding calculations and parent educational resources can also be found at the end of this blog post. We hope this has provided you with some helpful tips when managing these kiddos in the ED!
PRACTICAL PEARLS & RESOURCES:
Assessing feed volumes
- Standard formulas and breast milk have 0.66 kcal/ml
- Fortified formulas or breast milk may have up to 1 kcal/ml, though more commonly 0.83 kcal/ml
- Nutritional requirements for term infant growth: ~100 kcal/kg/day and for preterm infants: ~120 kcal/kg/day
- To determine how much the infant is being fed, use this calculation:
Daily caloric intake (kcal/kg/day) = [total feed volume (mls/day) x caloric density (kcal/ml)] / weight (kg)
Thickening Feeds
- Cereal thickener should be mixed with a 1:4 ratio of cereal:formula volume
- Commercial thickeners are available at most drug stores and have specific instructions on their packaging
- Education for parents:
- Thickened feeds should be prepared immediately before a given feed — to avoid over-thickening
- High flow nipple for bottle must be used (or it will get clogged up!)
- Breast milk should be thickened with carob bean base, a commercially available thickener, as amylase in breastmilk breaks down cereals
Milk-Protein Free Recommendations
- Formula options for hydrolyzed formula include: similac alimentum, progestimil A+, nutramigen A+
- Extensively hydrolyzed formulas such as neocate and puramino are rarely necessary and should be recommended in consultation with a pediatric specialist
- For breastfeeding mothers, McMaster Children’s Hospital has an excellent handout you can access here!
Infant Gastroesophageal Reflux Questionnaire Revised
I-GERQ-R is 14 item tool with questions around food refusal, symptoms of pain, and apnea, that can be used for diagnosis and symptom tracking. Each item of the questionnaire is scored and a total score of >16 is indicative of a clinical diagnosis of GERD.
** This tool has been shown to have a specificity of 100% and a sensitivity of 65%.3
REFERENCES