As global COVID-19 travel restrictions loosen, many people are finally taking the vacations they’ve been putting off for the last two years. As passenger air traffic climbs, in-flight medical emergencies will become increasingly frequent. Will you be ready when the call for a doctor on board goes out during your next flight?
This blog post aims to highlight the key considerations you should be making when responding to a medical emergency at 36,000 feet and help you feel more prepared to act when called upon.
How common are in-flight medical emergencies?
Determining just how commonly in-flight medical emergencies happen is challenging. Pre-pandemic there were approximately 3-4 billion passengers travelling the world’s airspace on an annual basis(1,2). The data on the incidence of in-flight medical emergencies is very limited for several reasons(3):
-
- There’s NO consensus definition on what problems constitute in-flight emergencies. Are flight anxiety, nausea, indigestion, or earache emergencies? There’s variability among studies as to which problems are included and which are not.
- There are NO international or national mandatory reporting systems or databases.
- A lot of this data – if it is recorded – is kept PRIVATE, in corporate airline records with policies prohibiting release for public dissemination and research.
The most recent study attempting to answer this question was a systematic review and meta-analysis published by Nascimento et al. in the American Journal of Emergency Medicine (2021). This study, which ultimately included 18 papers encompassing 1.5 billion passengers worldwide, estimated a global incidence of 18.5 in-flight medical emergencies per million passengers(2). However, the overall quality of evidence was low and variability among studies was high with a 95% confidence interval ranging from 0.5 to 53.4 in-flight emergencies per million passengers.
Despite many inconsistencies between data sets, one thing that all studies agree on is that incidence of in-flight medical emergencies is most probably underestimated in general for reasons including definitional differences and underreporting of less-complicated issues such as flight anxiety.
More importantly, the incidence of in-flight medical emergencies is expected to increase. Commercial airline traffic in Canada and internationally has been increasing and is expected to continue trending up. In fact, between 2009 and 2015, airline passenger traffic in Canada increased 27%(3). There are many reasons for this including cultural globalization and lower costs making air travel more accessible. Furthermore, long haul flights are becoming more common which increase the probability of on-board emergencies occurring and the passenger population is aging. By some estimates, within 10 years, half of all passengers travelling by air will be over 50 years old(4). As a corollary, more travellers will have medical comorbidities.
Physiologic considerations at 36,000 feet
At an average cruising altitude of 36,000 feet, modern commercial aircraft cabins are pressurized to a relative equivalent altitude of around 6000 – 8000 feet [dependent on age of the aircraft]. If you recall your high school chemistry back in 1802, Dalton described a law whereby the pressure of a mixture of gases is equal to the sum of the pressures exerted by all the gases in that mixture.
Ptotal = P1 + P2 + P3 + P4 + …
Or ambient air pressure is equal to the sum of the partial pressures of all the gases mixed into the air we breath.
Pair = PO2 + PN2 + PCO2 + PAr + …1
The physiologic consequence of this is that at altitude, airline passengers experience an arterial partial pressure of oxygen of O2 of 60 mmHg compared to 80 to 100 mmHg at sea level (5, 6). This is essentially equivalent to breathing an FiO2 of 15%. As a result, all passengers, regardless of their level of fitness experience relative hypoxia with normal oxygen saturations hovering around 92-93%. Now if you’re healthy, this isn’t a big deal. But those experiencing illness, such as cardiovascular disease or COPD are at an increased risk for dangerous, rapid desaturation.
The second ideal gas law to consider was described by Boyle back in 1662. Pressure exerted by an idea gas is inversely proportional to the volume it occupies, or
P1V1=P2V2
At altitude, as pressures decrease, volumes increase. Consequently, gas-filled compartments of the body expand as aircraft climb to cruising altitude. Physiologic compartment such as the sinuses, middle ear, and intestines can expand to cause discomfort. Non-physiologic compartments, such as pneumothoraces or post-operative gas collections can expand to cause bigger problems.
Additional stressors of air travel include(7):
-
- Low cabin air humidity that may contribute to dehydration.
- Passengers are often sleep-deprived with disturbed circadian rhythms.
- Passenger may be either hungry or dehydrated having not had time to eat. Conversely, they may have engaged in dietary indiscretion such as increased salt intake or have recently consumed exotic foods that may not agree with them.
- Emotional stress associated with flying such as anxiety or phobias around flying, cramped cabins, lengthy check in lines, delayed flights, enhanced security measures.
- Passengers may have consumed alcohol or other drugs in unwise quantities. Additionally, they may have missed doses or forgotten to pack their usual medications.
- Longer flight durations, particularly greater than 4 hours, with prolonged sitting decreases venous flow increasing the risk of venous thromboembolic events.
Legal and ethical responsibilities
Disclaimer: This is NOT legal advice.
The intricacies around responding to an emergency as a Good Samaritan, whether in the air or on the ground, are convoluted and fraught with pitfalls. Here, I’m going to distill it to the basics that can be applied to most situations, but NOT EVERY SITUATION.
International air travel defies all geographic and political boundaries. The legislation around assisting during in-flight medical emergencies is complex, not clear, inconsistent, and largely inadequate to say the least. There are frequent jurisdictional conflicts(8). Consider an Egyptian doctor, flying on an Air France flight over the Atlantic from Paris to Winnipeg with a stopover in Montreal. Is this doctor subject to Egyptian law, French law, Canadian common law, or Quebec civil law? It’s not clear and there is a great paucity of relevant case law to refer to.
Various international treaties, the Warsaw Convention in 1929, Tokyo Convention in 1969, and most recently the Montreal Convention in 1999 constitute the basis of modern aviation law. But, these treaties were largely established to regulate aircraft-related crimes and don’t really address the liability of volunteer, Good Samaritans acting while flying on non-domestic flights(8). In Canada, outside the province of Quebec, which is regulated by French-heritage civil law, there is in fact NO LEGAL DUTY or OBLIGATION on PHYSICIANS, or anyone for that matter, to provide volunteer emergency medical services to a person in peril. Generally, all jurisdictions around the world have some sort of legislation that protects physicians from liability if they choose to help.
It is worth mentioning that it is highly, highly unlikely that courts anywhere would criticize the conduct of a physician acting in good faith to treat a person in need of urgent medical attention. There has only been one case of an American doctor being sued for assisting in an in-flight emergency: the case was dismissed without a hearing. It’s actually more common for doctors to litigate against airlines for asking for help(8). If you’re at all concerned, remember that the CMPA will provide assistance to you anywhere in the world, including air and sea, whether you’re delivering care to residents of Canada or to residents of other countries. The CMPA further advises that you should treat with the goal of preventing prolonged suffering and addressing imminent threats to life, limb, or health(9). They also acknowledge that the expectations around said care may be different and more basic then what’s expected under normal circumstances.
From an ethical and professional point of view, all the Canadian medical regulatory bodies, state that physicians have an ethical duty to attend to people in need of urgent care. Not doing so, could potentially threaten their standing with the College. Furthermore, the CMA also states that we should “provide whatever appropriate assistance you can to any person with an urgent need for medical care”.
SO WHAT NOW?
Here are some general good practices to follow when volunteering to help(10):
-
- Remember there’s a good chance you’re the most qualified person to help. Introduce yourself. State your qualifications. Recognize and inform the cabin crew of the limits of your medical skills and act within those limits.
- Obtain patient consent, if feasible. It may be helpful to find a language interpreter on an international flight.
- Do not request financial compensation and don’t act with the expectation or pretence that you will be compensated. Doing so would change the relationship from that of a Good Samaritan to that of a vendor providing a professional service and could nullify legal protections. Airlines may offer tokens of gratitude of relatively insignificant value such as a box of chocolate or seat upgrade. These may be accepted as gifts – not as compensation(5,7). If in doubt or feeling uneasy, I would suggest just politely declining. The 10$ bottle of wine is probably not worth the risk of potentially throwing away a legal defence if it came to that.
- Document the event and care provided and keep it in your own locked records.
- If you’ve had something to drink or consumed recreational drugs, it’s best not to volunteer. There is a bit of a judgment call or gut check to make depending on the timing of consumption; you might still be the most qualified and capable person to help.
What in-flight resources are available?
Resources are obviously limited. You don’t have a lab, X-Ray, donut of truth (AKA CT Scan), or ultrasound, unless you packed your handheld in your carry-on.
PERSONNEL: Flight crews are an invaluable resource. In fact, 40-60% of IMEs are managed independently by flight attendants alone(3). They are all trained in basic first aid, CPR, and use of AED. They are familiar with specific aircraft and airline policies and may facilitate communication with the cockpit and/or ground-based support. Other passengers on board can also be recruited to help. There are probably other doctors, nurses, paramedics, or other medical professionals on board happy to lend a hand.
CALL A FRIEND: There’s also ground-based telemedicine support. These are third-party companies contracted by major airlines to assist during in-flight medical emergencies. Some airlines have in-house consultants as well. They are meant to help anyone navigate an emergency on board, including laypersons and health professional not comfortable managing emergencies. These ground crews can provide important logistic information e.g., ground transport time from the nearest landing strip to the nearest PCI or stroke centre. They will also help with making recommendations to the pilot around diversion.
EQUIPMENT/MEDICATIONS: Per Transport Canada Standard 725.91, there is a national standard minimum emergency medical kit that must be carried on all aircraft seating over 100 people, the contents of this minimum kit are listed below. Of note, on board AEDs are not mandated in Canada, but most airlines stock them voluntarily. They also carry oxygen tanks that can be used to administer relatively low flow rates(3).
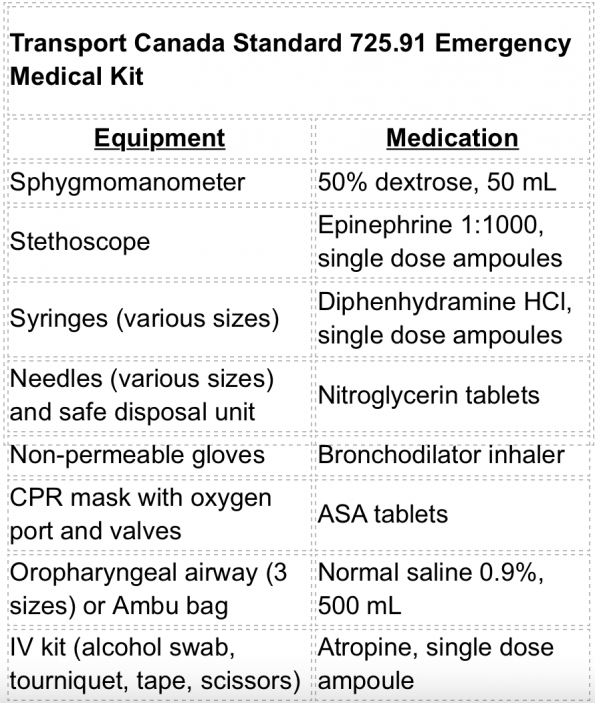
This minimum kit is quite limited in both equipment and medications. The American FAA kit contents are essentially identical(5,11). Fortunately, airlines have taken it upon themselves to stock their own, more comprehensive kits. The contents of Air Canada’s and WestJet’s emergency medical kits have recently been published here (See Table 1). There is quite a bit of variability between kit contents among Canadian airlines and international airlines. Some additional equipment may include: cricothyrotomy kit, burn dressing, foley catheter, glucometer with strips, laryngoscope with blades and ETTs, oximeter, thermometer, tongue depressor, scalpel, suture kit, and/or umbilical cord clamps (good luck if you need to pull those out!). Additional medications may include acetaminophen, diazepam, dimenhydrinate, epinephrine 1:10,000, furosemide, haloperidol, hydrocortisone, ibuprofen, ketorolac, loperamide, lorazepam, methylprednisolone, metoprolol, morphine, naloxone, ondansetron and/or oxytocin. Please be aware that airlines review their kits on an annual basis. They conduct cost-benefit analyses to choose what to include and what to remove, so kit contents are constantly changing.
FLIGHT DIVERSION: Flight diversion is the decision to change a flight’s destination because of an in-flight medical emergency(11). It’s a relatively rare thing to happen with only 4-7% of all in-flight emergencies requiring diversion. The most common causes of diversion, which is a product of the frequency of the problems and their seriousness, are(1):
| Cause for diversion: | % cases diverted | % of total diversions |
| Syncope or presyncope | 5% | 25% |
| Cardiac symptoms | 18% | 19% |
| Seizures | 12% | 9% |
| Respiratory symptoms | 6% | 9% |
| Possible stroke | 16% | 4% |
Flight diversion is a very complicated decision. Diverting a plane will typically cost an airlines 20-500,000 CAD but costs could reach up to a million dollars under certain circumstances(3). In addition to the medical considerations such as disease severity and need for further treatment or assessment there are several system factors that need to be considered including:
-
- The plane’s fuel reserves and ability to dump fuel prior to landing. Commercial aircraft have a maximum landing weight, so if a flight must land early it would need to get rid of its excess fuel.
- The medical capabilities of the nearest diversion site.
- Time-to-treatment benefit, considering landing procedures take around 30 minutes – continuing the course may not result in any meaningful treatment delay.
- There are social and personal issues at play as well. Perhaps a sick patient is on a flight returning home and doesn’t want to be delayed in reaching their destination.
- When responding to an emergency, we also need to be cognizant of our own biases around how diverting the plane would impact our own travel or vacation plans.
In one study, a multivariate analysis indicated that the presence of a physician onboard a commercial aircraft significantly increased the likelihood of diversion and patient post-flight admission(2).
Ultimately, the flight captain decides whether to divert a flight or not. They base that decision on information provided by ground-based supports around system factors, environmental factors, and the facts conveyed to them by volunteer responders about the patient’s state. You may be asked to provide your medical opinion as to whether diversion is warranted and they will expect a firm answer, but the pilot will decide based on multiple factors. That said, a pilot would probably be hard pressed to not divert a flight if a doctor told them it was medically indicated. You must make a recommendation that’s in the patient’s best interest. This akin deciding to call a consultant at 3 o’clock in the morning or advocating for a STAT MRI – resources are limited, but if it has to happen, it has to happen. It’s probably more likely that you recommend against diversion, and they do so anyway for airline liability reasons.
Common onboard medical emergencies (and what you can do about them)
According to a recent systematic review and meta-analysis, which included 18 studies encompassing approximately 1.5 billion commercial airline passengers worldwide, the five most common in-flight medical emergencies were syncope, gastrointestinal conditions, respiratory emergencies, neurological issues, and cardiologic complaints(2).
| Type of emergency | % total emergencies | Incidence (per million passengers) |
| Syncope | 32.7 % | 5 |
| Gastrointestinal conditions | 14.9% | 3 |
| Respiratory emergencies | 8.5% | 3 |
| Neurologic issues | 7.1% | 2 |
| Cardiologic complaints | 5.7% | 2 |
Now let’s highlight some considerations to make when managing the most common conditions seen on a plane – syncope, GI complains, Respiratory Distress, Neuro Emergencies and Cardiovascular complaints. We all know how to deal with these problems in the emergency department, but recall that available equipment and medications vary on an airplane, and even vary between airlines.
SYNCOPE: Syncope including presyncope is by far the most common problem. It’s usually reflex-mediated vasovagal or orthostatic syncope. If you have a glucometer, get a capillary blood glucose – this is an easily reversible cause. You’ll want to get the patient out of their seat, lay them down, and lift their legs. The crew can help you with this – do not lay them in the aisle, there will probably be a lot of onlookers and you want to try to respect patient privacy. Putting them in the aisle will cause an obstruction, interfere with crew movement, and potentially cause a pileup if an emergency landing and disembarking is needed. Good places to move them could be the galley (where the kitchen is), first class where there’s more floor space, in the open area in front of the bathroom, or potentially the crew’s resting quarters. If you recall Dalton’s Law, it’s generally always a good idea to provide oxygen. Available medications to consider are dextrose and normal saline. Most patients recover spontaneously within minutes and don’t need diversion.
GASTROINTESTINAL: Gastrointestinal conditions include nausea, vomiting, diarrhea, dyspepsia, and acute abdominal pain. When dealing with body fluids, remember your PPE. Helpful medications are whatever analgesic is in the kit, fluids, and dimenhydrinate. Depending on airline, you may find ondansetron and/or loperamide. If the patient has a peritonitic abdomen, consider diversion.
RESPIRATORY: Respiratory emergencies most commonly include shortness of breath, asthma, and COPD exacerbations. If there’s concern for an infectious disease, again remember your PPE. Oxygen is the most important treatment. Other treatments are based on clinical impression. Epinephrine is universally carried. The kits are generally stocked with puffers and steroids. There may also be useful medications for heart failure. If for some unusual reason, someone took a flight with a pneumothorax you could perform a needle decompression and recommend diversion for definitive treatment. If you’re fortunate enough to be travelling in a private jet, you could potentially ask the pilot to drop to a lower altitude, but this won’t happen on a commercial aircraft. Instead, the plane would have to be diverted because they can’t fly in an aerodynamically efficient way at an altitude low enough to affect your pneumothorax.
NEUROLOGIC: Neurological issues include possible stroke, weakness, numbness, or paresthesias, and seizures. Again, get a capillary blood glucose. As with syncope, it’s best to find a place to lay these patients down supine, protect their airway, and obtain an advanced airway if necessary. Give everyone oxygen. There are benzodiazepines for seizures. There is also ASA, that may provide some benefit in possible stroke. If you suspect a stroke or a seizure is prolonged or recurring, strongly consider diverting. Early, specialized intervention is paramount in treating these problems.
CARDIOVASCULAR: Cardiovascular complaints include chest pain or angina, persistent bradycardia or tachycardia, arrhythmias, and suspected MI. Follow AHA guidelines as best you can. Oxygen, ASA, nitroglycerin, and atropine are all part of the Transport Canada Emergency Medical Kit so would be available on all Canadian airlines. Air Transat carries metoprolol. This is a common reason for diversion and subsequent hospital admission.
DEATH: I want to briefly discuss death on a plane. Thankfully it’s rare with an incidence of 0.21 per million passengers, but if you consider the number of passengers worldwide that still amounts to about 1 death on an airline per day. First make sure it’s not just vagovagal syncope, then proceed to follow AHA guidelines. Designate a crew member to get the AED and apply it. You may have access to lidocaine if the AED advises shocking. Some Canadian airlines don’t carry cardiac epinephrine so you’d have to dilute the 1 in 1000 ampule in 9 cc of NS, or alternatively you could try just pushing it slowly, but the priority is really good CPR and AED use. The probability of a good outcome in out-of-hospital cardiac arrest is already poor on the ground. The chance of a good outcome in this austere environment is certainly lower. Generally, it’s accepted to terminate resuscitation if ROSC isn’t achieved within 20-30 minutes(11). Only an MD can pronounce death on a flight. In some jurisdictions, death can only be pronounced upon landing. Dead bodies are typically kept in their seat (or switched to a window seat to not box in some unfortunate passenger or flop into the aisle) and are covered with an eye mask, oxygen mask, and bag to collect potential leaking fluids.
To wrap up, I just want to mention some special considerations for pediatric passengers. Some of you may not see kids in the ED regularly and may feel less comfortable in these situations. Overall children account for 5-10 % of all in-flight medical emergencies(12,13). They’re most affected by gastrointestinal symptoms, infectious syndromes such as fever and acute otitis media – again think back to how Boyle’s law could make this specific problem worse, and neurologic problems which are usually seizures. Kids are also more prone to traumatic injuries and burns, especially if they’re seated unrestrained on a parent’s lap or in an aisle seat(13). About 11% of pediatric in-flight emergencies require diversion usually because of prolonged seizure or asthma exacerbation(12).
Conclusions and Take-Home Points
To conclude, I leave you with a few general take-home points:
-
- Given the growth of air travel, and the aging, generally more comorbid population, in-flight medical emergencies are becoming more common.
- We are emergency experts. We’re experts in dealing with uncertainty. Experts in working with limited resources. Experts in chaos. These problems fall squarely in our wheelhouse, and we should be ready to deal with them. I hope this blog post helped you feel a little bit more prepared.
- Trying to navigate the laws is too complicated – don’t worry about it too much. We have ethical and professional duty to help and know that we a well-protected in doing so.
- This is an austere, uncomfortable environment. As you’ve read, the emergency medical kits are limited and vary by airline. Do what you can with what you have. Know your limitations and accept them.
For those who may be interested in learning more, I encourage you to check out the Onboard Medical Emergencies course. This one-day course for health professionals interested in the subject of aviation medicine or in-flight emergencies takes place at Air Canada’s headquarters in Montreal on an annual basis. Check out this video that reviews Air Canada’s emergency medical kit. Finally, consider downloading the free iPhone/Android application airRx, which reviews common in-flight emergencies, national standard medical kit contents, and crew and ground-support roles.
Special thanks to Drs. Simeon Mitchell, Mike Rubin, Vincent Poirier, Andrew Mulloy, and Jason Frank for their contributions and advice.
Safe travels!



