Patients with cirrhosis are complex, with a plethora of comorbidities. They often present to emergency departments (ED) very sick, and there are many complications that emergency physicians need to know about. In this post, we’re going to focus on Spontaneous Bacterial Peritonitis (SBP) in patients with cirrhosis.
There’s a lot to discuss about SBP, so there will be several aspects of this pathology that we don’t touch on in this post, not because they’re not important, but because there are other critical take-home points. Many of the specifics not discussed in this post can be found in the latest 2018 EASL guidelines. (1)
What I want you to get out of this post are the critical actions that Emergency physicians (You!) can do for each of these conditions.
Take-home Point 1: Adopt an extremely low threshold to perform a diagnostic paracentesis in the cirrhotic patient because SBP is an emergency diagnosis with high mortality and subtle presentation.
We have to respect SBP. It is deadly, and is a true emergency. For every four patients that you diagnose with Spontaneous Bacterial Peritonitis and treat with antibiotics, one will still die in hospital. (2,3)
SBP is a bacterial infection of ascites. The theory of how this spontaneous infection occurs is that the bacteria translocate from the GI tract. So naturally, Escherichia coli is the most common pathogen isolated, with Klebsiella pneumoniae as the second most common. (4)
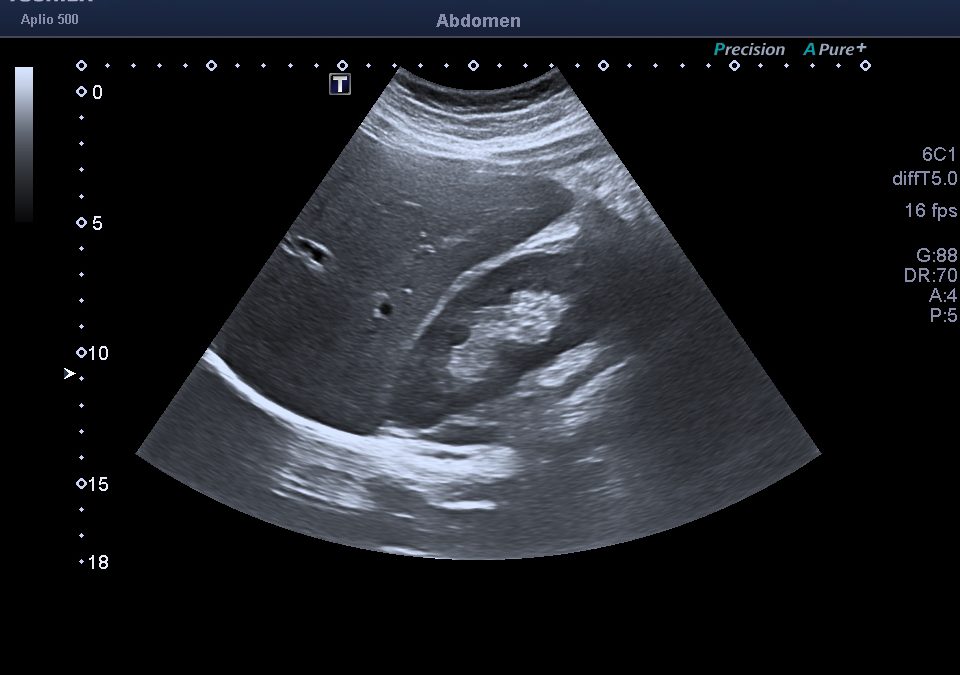
Where there are bugs, there are neutrophils. To diagnose SBP, we must do a diagnostic paracentesis and look at the absolute neutrophil count. The paracentesis findings of SBP are an ascitic absolute neutrophil count of greater than 250 cells/mm3. (5)
But who should we do a paracentesis on?
Well, it depends on how SBP presents. This is how we think SBP presents: fever and abdominal pain. But only about ½ of patients with SBP present with fever and abdominal pain…meaning ½ of your patients won’t have these symptoms. (2)
Rather, SBP can present as any of the following (6):
- Isolated hepatic encephalopathy
- Renal failure
- GI bleeding
- Any abnormal vital signs
- Vomiting
- Metabolic acidosis
- Leukocytosis
One study, which included paracentesis done in outpatient clinics, even found up to 13% of SBP patients were asymptomatic. (2) The fact that something with a mortality of 25% can be that indolent should terrify you.
That’s why the latest EASL guidelines from 2018 recommend that we do a diagnostic paracentesis on every patient with cirrhosis and ascites that requires hospitalization. Every patient. (1)

If you miss this diagnosis and discharge the patient home, their mortality approaches 90%. That’s why it’s a critical diagnosis. (1) Every hour that you delay a diagnostic paracentesis in a patient with SBP increases their mortality by 3.3%. (7) That’s why this is an emergency medicine diagnosis, and why you shouldn’t defer doing the paracentesis to the inpatient team.
This is a critical action that emergency physicians can take. On your next emerg shift, adopt an extremely low threshold to perform a diagnostic paracentesis in the cirrhotic patient, because SBP is an emergency diagnosis with high mortality and subtle presentation.
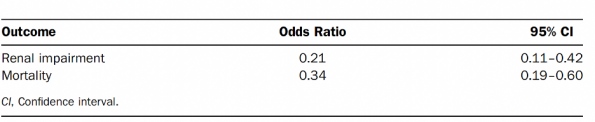
So let’s say you see a patient with ascites from cirrhosis presenting with new renal failure. You do the paracentesis and you diagnose SBP. You know you’ll give them antibiotics (3rd generation cephalosporin for community-acquired SBP in low antibiotic resistance areas) for treatment. (1) Without antibiotics, SBP has a mortality of 90%. With appropriate antibiotics, the mortality is still 25%. (1,3) But what if I told you you’re not done. What if I told you, you could improve that patient’s mortality risk to about 10% with another treatment. That treatment is albumin. The EASL guidelines of 2018 recommend that we give albumin at diagnosis at a dose of 1.5 g/kg. This is a grade I recommendation by the latest guidelines. (1) It’s based on the theory that albumin would increase intravascular volume but also binds endotoxins in patients with SBP and ultimately prevent hepatorenal syndrome and subsequent death. There have been 4 RCTs looking at albumin’s role in SBP. They all showed benefit, but most of these studies were fairly small. (8) A meta-analysis of these studies was done with a total of 288 patients with SBP. (8) In the studies, patients all received a 3rd generation cephalosporin. They then compared renal function and mortality with patients that also received albumin. The dose of albumin used in the largest study was 1.5 g/kg within 6 hours of diagnosis. (8) This was the outcome when patients received albumin in addition to antibiotics within 6 hours of diagnosis. The OR for renal failure was 0.21. The OR for mortality was 0.34. (8) Now there are criticisms of this paper. The trials had small study sizes, and only one of them was blinded. So, there are certainly methodological flaws in the included RCTs. Unfortunately, the fact is that this is the highest quality evidence that we have right now. The best evidence at the moment says that albumin has an NNT of 6 to prevent one death. And it has an NNT of 4 to prevent renal failure. (1,8) So, this is a second critical action you can take on your next shift. Order albumin at 1.5 G/KG within 6 hours of diagnosis for your patients with SBP and help lower the mortality of this dangerous disease.Take-Home Point 2: Order albumin at 1.5 g/kg when you diagnose SBP and confer a mortality benefit to your patient.
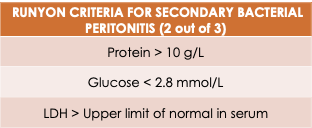
About 1 in 20 cases thought to be spontaneous peritonitis are actually secondary to another source. (1,5) In contrast to spontaneous bacterial peritonitis, Secondary Bacterial Peritonitis is when ascites fluid is infected but it’s due to another intraabdominal infection. It’s secondary to another source, like appendicitis, or cholecystitis, or perforation. When you do the paracentesis, you’ll still have an absolute neutrophil count > 250 cells/mm3, and you will be tempted to call this spontaneous, when in fact, it is secondary from another source. The reason this matters is that secondary peritonitis is a surgical pathology. Without surgery, their mortality is around 100%. Because we wouldn’t be treating the source.(6) We know our disposition decisions matter. Where we send patients matters. If you send a patient with secondary peritonitis to a medical service, that patient will likely die. So how are you going to tell on your next shift it’s secondary or spontaneous peritonitis? Unfortunately, there’s not really much on history that will differentiate spontaneous from secondary bacterial peritonitis. When you look at the physical exam, secondary peritonitis tends to have more abdominal pain in contrast to spontaneous bacterial peritonitis. A multivariate analysis was done to try to differentiate spontaneous from secondary bacterial peritonitis. They found that 80% of the secondary peritonitis patients had abdominal pain – a lot more than normal SBP. (1,6) The abdominal pain in spontaneous bacterial peritonitis tends to be mild, while secondary peritonitis tends to have more severe and focal findings. But it’s not cut and dry. These two pathologies are pretty challenging to differentiate with history and physical. The Runyon Criteria were created to help differentiate the two These criteria have a specificity of 90%, but a sensitivity of 66% for secondary bacterial peritonitis. (6) So, as emergency physicians, we can’t use Runyon criteria to rule out secondary peritonitis. However, applying the Runyon criteria can push you to do a CT when you weren’t going for other reasons. Now just because you can’t use Runyon’s criteria to rule out the disease, I’m not saying you should CT or ultrasound every single patient with cirrhosis and ascites for secondary peritonitis. Ultimately you need to recognize that you’re in a challenging situation and are at high risk of missing a surgical pathology in this patient. In general, you should probably image patients you’ve diagnosed with SBP if they have any of the following:Take-Home Point 3: Always consider the diagnosis of secondary peritonitis in your cirrhotic patients that you have diagnosed with SBP.

Conclusion
So it’s up to you to take action. You have a chance to do something that really matters to these patients. And you now know of the critical actions that you can do on shift. So if you carry even one of these critical actions with you on your next shift, just one, you can make a real difference to the person in front of you.
References


Trackbacks/Pingbacks