Medical Cardiac Arrest – To TOR or Not To TOR?
Base Hospital Physicians Corner – or BHP Corner – is a new web-series we are introducing to be published in a quarterly fashion. Written by RPPEO Base Hospital Physicians, these publications will focus on targeting questions and concerns brought forward by RPPEO paramedics, as they pertain to key topics/actions taken in prehospital medicine.
First up – Termination of Resuscitation.
—
Everyday, EMS providers respond to patients in cardiac arrest who fail to revive during pre-hospital resuscitation. This is the most common reason why a base hospital physician will be consulted. Over the past two decades, prehospital Termination of Resuscitation, or TOR, has become a standard practice for those whom ongoing resuscitation is determined to be futile.
TOR Benefits
The cardiac arrest patch point for Advance Care Paramedics (ACPs) and Primary Care Paramedics (PCPs) has reduced transports with ongoing CPR by more than 40%.
This patch point allows paramedics to call the BHP during active cardiac resuscitation, if certain clinical criteria are met, to request a medical TOR.
The benefits of prehospital TOR are numerous:
-
- Fewer high-speed transports reduces the risk of ambulance collisions;
- Fewer lifting injuries;
- Less CPR performed by unrestrained providers in moving ambulance;
- Paramedics are available for the next call sooner.
Most importantly, prehospital TOR puts the focus at the scene on the interventions that are known to make a difference in outcomes in cardiac arrest:
-
- Early high-quality CPR;
- Defibrillation.
Studies have repeatedly shown that paramedics and families are comfortable with prehospital TOR.
TOR Controversy: Missed Survivors?
With the above mentioned benefits to prehospital TOR, it’s natural that paramedics would hope for and expect their request for TOR to be granted. However, at times, a BHP will leave their EMS colleagues frustrated and questioning why a particular individual has been suggested to be transported to hospital, despite a TOR being requested.
“Why might the Base Hospital Physician recommend transport to the hospital when the paramedic patches and asks to consider prehospital TOR?”
Let’s begin with the premise that we all agree that the benefits of prehospital TOR must be balanced with the imperative to ensure we do not cease resuscitation on a person who would have survived had efforts been continued. Or, in other words, as we embrace the value of prehospital TOR, we don’t want to “miss” a survivor through premature termination of resuscitation.
A look at the Evidence
Next, let’s look at what the studies show us about the predictors of survival in prehospital cardiac arrest.
The initial studies that examined what happens to patients who do not respond to prehospital ACLS were done in the United State’s in the 1990s. These showed that while most patients did not survive despite transport to hospital, there were a few survivors to hospital discharge in the cohort. The survivors either had sustained ROSC at some point in the resuscitation, or shock refractory ventricular fibrillation or tachycardia.
A more recent study performed in Montreal found a survival rate of 8% for patients who had received up to 9 shocks for shock-refractory ventricular arrhythmias. For this reason, patch physicians (and paramedics) are likely to consider continued resuscitation and transport for these patients (refractory VF/VT or sustained ROSC during resuscitation).
For PCPs, we have the world’s best evidence for TOR derived and validated by researchers here in Ontario. In 2006, the TOR researchers found that when paramedics attended the scene of cardiac arrest from presumed cardiac cause and 3 criteria were present:
1. It was not witnessed by a first responder;
2. There was no ROSC during the resuscitation, and;
3. No shocks were delivered.
Most of these patients (772 out of 776) did not survive despite ongoing resuscitation and transport to hospital. However, it is worth noting, that the above criteria to terminate resuscitation were met for 4 patients who did survive – three of these patients had good neurological outcomes.
More recently, in an external validation study, of the BLS TOR rule carried out in British Columbia, the TOR rule recommended termination for 4,367 patients out of 6,994 at the 6-minute mark of the resuscitation (the time of the mandatory patch point in the ALS PCS), and 92 of these patients survived. In other words, for every 100 cardiac arrests, 2 patients could survive at 6 min despite meeting the TOR criteria. Most of these patients had good neurological outcomes, even though the rule predicted they would not survive. If the resuscitation continued and the rule was applied at 20min, <1% survived, and at 30 minutes, the rule performed much better and there were no survivors. Of note, of the survivor for whom the rule predicted termination at 6 minutes, nearly all achieved ROSC prior to transport, indicating the benefit of on-scene efforts rather than transport with CPR in progress.

Some Patients Benefit From More Resuscitation
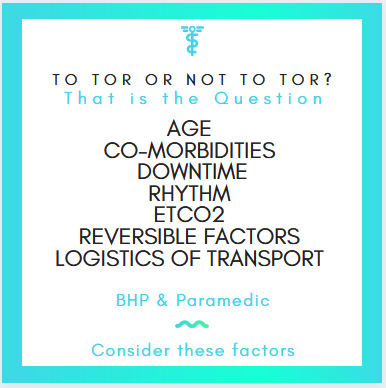
You can see that while the rule is quite accurate at identifying non-survivors, it is not perfect. Clearly there are patients you will encounter for whom the prognosis seems poor, but who will go on to survive if an aggressive resuscitation continues. Unfortunately, there are no black and white rules for identifying survivors with 100% accuracy. This is the reason for the need for early consultation with the base hospital physician. Clinical judgement is required, considering factors such as:
-
- Age;
- Co-morbidities;
- Downtime (was it witnessed?);
- Rhythm;
- EtCO2;
- Reversible Factors;
- The logistics of transport (extrication and transport time).
There might be circumstances where we agree that transport with CPR is not going to be helpful, but we believe further resuscitation is warranted, especially considering the evidence presented above. In these cases, we might recommend further attempts to establish ROSC at the scene before deciding to terminate (i.e. work the patient longer and call the base hospital physician back).
Consider Early Transport
Conversely, some patients might benefit from early transport. Consider causes of arrest that could be reversed with hospital-level care:
-
- Suspected Pulmonary Embolus;
- Certain Overdoses (think cardiotoxic drugs like Digoxin, Calcium Channel Blockers, TCAs);
- Hypothermia;
- Refractory VF.
Some findings could indicate a favourable prognosis and might benefit from early transport – for example a narrow complex PEA AND EtCO2 >20mmHg (is the pulse just too weak to feel?).
Therefore it is important for EMS providers to consult the base hospital physician early if they think the patient would benefit from a different approach than the traditional advanced directive. Unfortunately, there is no one-size-fits-all strategy, and the excellent clinical judgment of EMS providers is required.
Paramedic/BHP Collaboration on TOR Decisions
As much as the base hospital physician must be satisfied that we are dealing with a non-survivor before recommending TOR, the paramedics at the scene must be comfortable with this disposition as well. Prehospital care physicians or BHP understand the medicine and their colleagues capabilities, but are not at the scene. There are factors that a physician cannot fully appreciate that may influence a paramedics comfort with TOR. It is imperative to know that TOR is a collaborative decision between the scene providers and the base hospital physician.
Call Early to Honour Patient’s Wishes
In some cases, paramedics arrive at the scene of a cardiac arrest and are presented with verbal or written instructions indicating the patient would not want resuscitation (DNR). If you believe these instructions are valid and the patient would not want resuscitation, it is imperative that the base hospital physician be consulted early to collaborate on decisions around initiating or withholding resuscitation, or early TOR.
TOR should never be recommended if the on-scene medical providers/paramedics or the family are uncomfortable with the decision, and would prefer to transport. The decision for TOR MUST BE COLLABORATIVE.
References
- Bonnin M, Pepe P, Kimball K, et al.: Distinct criteria for termination of resuscitation in the out-of-hospital setting. JAMA. 1993; September 22; 270:1457-62.
- Cournoyer A, Notebaert E, Cossette S, et al.: The prognostic significance of repeated prehospital shocks for out-of-hospital cardiac arrest survival. CJEM. 2019; 21(3): 330-38.
- Grunau B, Taylor J, Scheuermeyer F, et al.: External validation of the universal termination of resuscitation rule for out-of-hospital cardiac arrest in British Columbia. Annals of Emergency Medicine. 2017; September; 70(3): 374-81.
- Morrison L, Visentin L, Kiss A, et al.: Validation of a rule for termination of resuscitation in out- of-hospital cardiac arrest. NEJM. 2006; August 3; 355:478-87.
- Morrison L, Eby D, D’Souza P, et al.: Basic life support termination of resuscitation guideline implementation trial (TORIT). Circulation. 2009; November 3; 120:S1472.


This is a great article outlining the process. It mentioned key factors such as early CPR and defibrillation, but what about ALS drug interventions? I’m referring to ALS protocol epinephrine Q4 mins for medical arrests. Has epinephrine proven more positive outcomes in pre-hospital medical cardiac arrests? If so, is this a scope to be considered for PCP administration in medical arrests?
Personally, I’ve hit roadblocks with BHP patches for a TOR as a PCP as a result of not being able to administer epinephrine. Lots of great information here!
Great question! Epi in cardiac arrest is still actually quite controversial:
https://emottawablog.com/2018/10/a-randomized-trial-of-epinephrine-in-out-of-hospital-cardiac-arrest/