The acutely injured knee can often be challenging to assess when there is no associated fracture. Identifying the possible non-bony acute pathology is important to help discern the most appropriate approach to treatment for the patient.
Assessment
History
- Mechanism of action
-
- Contact
- Twist/Pivot
-
- Onset of symptoms:
-
- Immediate vs delayed symptoms
- Able to finish their activity?
-
- Symptoms
-
- Where the pain is felt
- Mechanical symptoms; catching, clicking, locking
- Giving out/unstable
-
- Past Medical History for Risk Factors:
-
- Medications (steroids, fluroquinolones), diabetes, connective tissue disease
- What is their baseline function? i.e.: young athlete vs injury during bed to wheelchair transfer
-
Exam
- Position:
-
- Supine
- Bilateral leg exposure
- Most comfortable position for patients
- Support leg as much as possible throughout exam (provide towel under knee for comfort)
- Limit movement
-
- Observe:
- Can they ambulate?
- Analgesia:
-
- Prior to exam
- +/- Procedural sedation for patella reduction
-
- PoCUS:
-
- Helpful to identify fractures, tendon injury, effusions
-
- Arthrocentesis:
-
- Should be considered in patients with acute knee injury with a large effusion, decreased ROM and normal X-Ray
- Arthrocentesis performed in the ED for ACL injury causing effusion, pain and decreased ROM showed improvement in pain, range of motion and accuracy of exam maneuvers at follow-up visit (Wang et al. 2016).
-
- Traumatic Hemarthrosis (Potpally et al 2021)
-
- 70% of ACL tears
- 10% of patella subluxation/dislocation
- 10% of meniscal tears
- 5% of osteochondral fractures
- 5% other (i.e.: PCL tears)
-
- Movements to check:
-
- Check Extensor mechanism while supine, not sitting as ITB is a knee extensor at 30 degrees of knee flexion when it moves from posterior to anterior over the lateral femoral condyle
- Stability (ligaments)
- Intra-articular (meniscal)
-
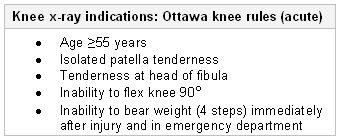
Ottawa Knee Rules
Patients presenting with acute knee injury require X-ray if:
Pathologies
Occult Knee Dislocation
- Mechanism of injury:
-
- Dashboard/MVC
- Ground level falls in elderly or obese patients
- 20-50% of knee dislocations will spontaneously reduce prior to ED arrival
-
- Exam:
-
- Ligamentous instability in at least 3 of the 4 ligatments
-
- ED investigations:
-
- X-Ray to rollout fracture
- Ankle-Brachial index
- CT-A
-
- ED Management:
-
- If hard signs of vascular injury; STAT vascular consult +/- vascular injury
- If abnormal ABI –> CT-A (consult ortho +/- vascular)
- If normal ABI –> consult ortho
-
- Referral:
-
- Consultation in the ED for admission/management
-

Patella Dislocation
- Mechanism of Injury:
-
- Planted foot with internal rotation/twisting on a valgus flexed knee
- Dancing, baseball swing, quick lateral change
- Lateral dislocation most common
-
- Exam:
-
- Laterally displaced patella for lateral dislocation
- Subluxation: positive patella apprehension test
-
- Investigations:
-
- X-Ray with skyline views to rollout acute fracture (osteochondral fractures commonly missed)
- X-Ray not required prior to reduction (Krause et al, 2013)
-
- ED Management
-
- Reduce by straightening leg and gently tip & tilt patellar laterally then medially
- Immobilize
- Counsel
-
- Brief immobilization for comfort (3-4 days)
- Ice and elevate
- Weight bearing as tolerated
- Limit walking, standing, repetitive bending
- Use a patella restraining brace
- Physiotherapy for retraining/strengthening quads
- Athletes return to play in 4-6 weeks
-
- Referral:
-
- Plater clinic if: associated fracture, recurrent dislocations, associated injury (eg: ACL, MCL tears)
- All reduced dislocations can be referred to plaster clinic/orthopedics, or if there are absolutely no concerns for other injuries they can be sent to their family physician or sports medicine specialist.
- Physiotherapy
-
-
Patella Tendon Rupture
- Mechanism of injury:
-
- Jumping sports
- Sudden quadriceps contraction with flexed knee (patellar tendon injury)
- Sudden quadriceps contraction when landing from a jump with a flexed knee (Quads tendon injury)
-
- Exam:
-
- Extensor mechanism will not be intact, therefore unable to complete straight leg raise
- Defect distal to the patella (defect proximal to patella suggests quads tendon rupture)
-
- ED Investigations:
-
- X-Ray to rule out fracture – patella alta (patella tendon rupture), patella baja (quad tendon rupture)
- PoCUS: identify the tendon defect
-

Patelle Baja
- ED Management:
-
- Immobilize in zimmer
- Consult ortho in ED to book for surgery
-
- Referral:
-
- Surgical intervention required
-
Ligamentous Injury
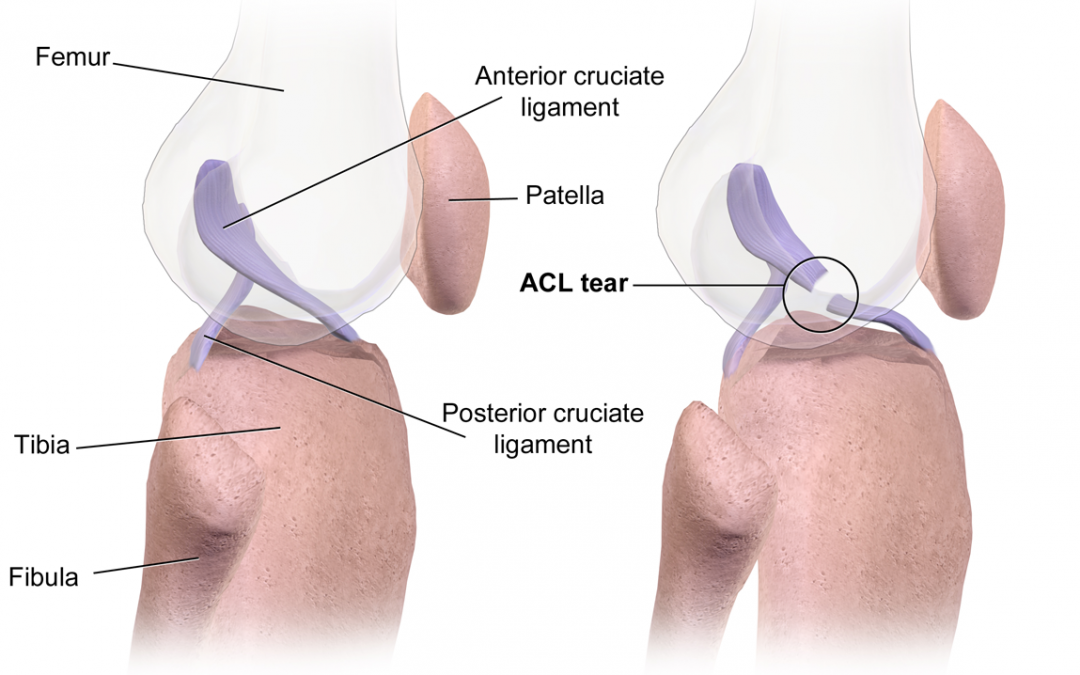
Anterior Cruciate Ligament:
- Mechanism of injury:
-
- Non contact: pivot
- Contact: blow to lateral aspect of knee
-
- Exam:
-
- Lachman
- Anterior Drawer
- Lever Sign
- Pivot Shift Test – not accurate in the ED
-
- ED Investigations:
-
- X-Ray to look for Segond or tibial spine fracture
-
- ED Management:
-
- Crutches, WBAT, RICE
-
- Referral:
-
- In young athletes that you are confident have an ACL tear -> outpatient MRI + ortho referral
- If you are not confident that there is a significant injury, they need to be re-examined in ~1wk -> family physician or sports medicine referral
- Minor injury or poor baseline -> family physician
-
Medial Collateral Ligament
- Mechanism of injury:
-
- Contact: blow to lateral aspect of knee
-
- Exam:
-
- Laxity/soft end feel with valgus stress test at 30 degrees of knee flexion for isolated MCL injury
-
- ED Investigations:
-
- X-Ray to rule out fracture
-
- ED Management:
-
- Crutches, WBAT, RICE
-
- Referral:
-
- In young athletes that you are confident have at least a MCL tear -> outpatient MRI + ortho referral
- If you are not confident that there is a significant injury, they need to be re-examined in ~1wk -> family doctor or sports medicine referral
-
Lateral Collateral Ligament
- Mechanism of injury:
-
- Contact: blow to medial aspect of knee
-
- Exam:
-
- Laxity/soft end feel with varus stress test at 30 degrees of knee flexion for isolated LCL injury
-
- ED Investigations:
-
- X-Ray to rule out fracture
-
- ED Management:
-
- Crutches, WBAT, RICE
-
- Referral:
-
- Family physician or sports medicine specialist for re-examination +/- imaging
- Isolated LCL injuries are rare
-
Posterior Cruciate Ligament
- Mechanism of injury:
-
- Dashboard
- Hyperflexion with plantar flexion of foot
-
- Exam:
-
- Posterior Sag Sign
- Posterior Drawer
- Could have valgus/varus laxity at 0 degrees of knee flexion
- Dial test to differentiate isolated PCL vs associated injuries (PLC)
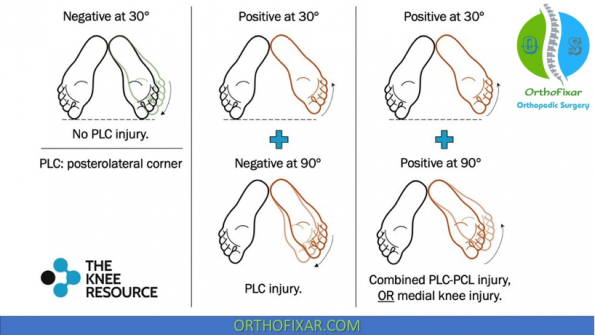
- ED Investigations:
-
- X-Ray to rule out fracture
-
- ED Management:
-
- Crutches, WBAT, RICE
-
- Referral:
-
- Family physician or sports medicine specialist for re-examination +/- imaging.
- In young athletes that you are confident have at least a high grade PCL tear -> outpatient MRI + ortho referral
-
-
Posterolateral Corner
- Mechanism of injury:
-
- Non contact: external rotatory/twisting
- Contact: blow to anteromedial aspect, hyperextension, MVC (knee dislocation)
-
- Exam:
-
- Varus and Valgus stress at 0 degrees of knee flexion
- Dial test
- Reverse pivot shift test (not accurate in the ED)
-
- ED Investigations:
-
- X-Ray to rule out fracture
-
- ED Management:
-
- Unstable knee (at least 3 ligaments torn) -> ortho in the ED
- Crutches, WBAT, RICE
-
- Referral:
-
- Sports medicine specialist or family physician for re-examination +/- imaging
-
Meniscus
- Mechanism of injury:
-
- Non contact: sudden change in direction – commonly seen in soccer, basketball, football and rugby
-
- Exam:
- ED Investigations:
-
- X-Ray to rule out fracture
-
- ED Management:
-
- Crutches, WBAT, RICE
-
- Referral:
-
- If mechanical symptoms (locking) -> Outpatient MRI + ortho referral
- If no mechanical symptoms -> family physician or sports medicine specialist for re-examination +/- imaging
-
References
Cardone, D. A., & Jacobs, B. C. (2022). Meniscal injury of the knee. UpToDate. http://aplicacionesbiblioteca.udea.edu.co:4560/contents/meniscal-injury-of-the-knee?source=search_result&search=lesión+de+meniscos&selectedTitle=1~45
Chahla, J., Moatshe, G., Dean, C. S., & Laprade, R. F. (2016). Posterolateral Corner of the Knee: Current Concepts. The Archives of Bone and Joint Surgery, 97(9), 97–103.
Guillodo, Y., Rannou, N., Dubrana, F., Lefèvre, C., & Saraux, A. (2008). Diagnosis of anterior cruciate ligament rupture in an emergency department. Journal of Trauma – Injury, Infection and Critical Care, 65(5), 1078–1082. https://doi.org/10.1097/TA.0b013e3181469b7d
Guiraud, K., Silvestre, G., Bastin, C., Lecouvet, F. E., Benitez Masip, A., Boyadzhiev, D., Meert, P., & Thienpont, E. (2022). Higher sensitivity with the lever sign test for diagnosis of anterior cruciate ligament rupture in the emergency department. Archives of Orthopaedic and Trauma Surgery, 142(8), 1979–1983. https://doi.org/10.1007/s00402-021-04154-x
Koster, C. H., Harmsen, A. M. K., Lichtenberg, M. C., & Bloemers, F. W. (2018). ACL injury: How do the physical examination tests compare? Journal of Family Practice, 67(3), 130–134.
Krause, E. A., Lin, C. W., Ortega, H. W., & Reid, S. R. (2013). Pediatric lateral patellar dislocation: Is there a role for plain radiography in the emergency department? Journal of Emergency Medicine, 44(6), 1126–1131. https://doi.org/10.1016/j.jemermed.2012.11.014
Lelli, A., Di Turi, R. P., Spenciner, D. B., & Dòmini, M. (2016). The “Lever Sign”: a new clinical test for the diagnosis of anterior cruciate ligament rupture. Knee Surgery, Sports Traumatology, Arthroscopy, 24(9), 2794–2797. https://doi.org/10.1007/s00167-014-3490-7
Maffulli, N., Binfield, P. M., King, J. B., & Good, C. J. (1993). Acute haemarthrosis of the knee in athletes. A prospective study of 106 cases. Journal of Bone and Joint Surgery – Series B, 75(6), 945–949. https://doi.org/10.1302/0301-620x.75b6.8245089
McQuivey, K. S., Christopher, Z. K., Chung, A. S., Makovicka, J., Guettler, J., & Levasseur, K. (2019). Implementing The Lever Sign in the Emergency Department: Does It Assist In Acute Anterior Cruciate Ligament Rupture Diagnosis? A Pilot Study. 57(6), 805–811.
Meserve, B. B., Cleland, J. A., & Boucher, T. R. (2008). A meta-analysis examining clinical test utilities for assessing meniscal injury. Clinical Rehabilitation, 22(2), 143–161. https://doi.org/10.1177/0269215507080130
Orlando Júnior, N., de Souza Leão, M. G., & de Oliveira, N. H. C. (2015). Diagnosis of knee injuries: comparison of the physical examination and magnetic resonance imaging with the findings from arthroscopy. Revista Brasileira de Ortopedia (English Edition), 50(6), 712–719. https://doi.org/10.1016/j.rboe.2015.10.007
Parwaiz, H., Teo, A. Q. A., & Servant, C. (2016). Anterior cruciate ligament injury: A persistently difficult diagnosis. Knee, 23(1), 116–120. https://doi.org/10.1016/j.knee.2015.09.016
Potpally, N., Rodeo, S., So, P., Mautner, K., Baria, M., & Malanga, G. A. (2021). A Review of Current Management of Knee Hemarthrosis in the Non-Hemophilic Population. Cartilage, 13(1_suppl), 116S-121S. https://doi.org/10.1177/1947603520942937
Rossi, R., Dettoni, F., Bruzzone, M., Cottino, U., D’Elicio, D. G., & Bonasia, D. E. (2011). Clinical examination of the knee: Know your tools for diagnosis of knee injuries. Sports Medicine, Arthroscopy, Rehabilitation, Therapy and Technology, 3(1), 1–10. https://doi.org/10.1186/1758-2555-3-25
Sharareh, B., Skaggs, D., & Taylor, B. (n.d.). Knee & Sports High-yield topics. Orthobullets. Retrieved September 10, 2022, from https://www.orthobullets.com/topic/dashboard?id=225&specialty=225&expandLeftMenu=true
Strudwick, K., McPhee, M., Bell, A., Martin-Khan, M., & Russell, T. (2018). Review article: Best practice management of common knee injuries in the emergency department (part 3 of the musculoskeletal injuries rapid review series). EMA – Emergency Medicine Australasia, 30(3), 327–352. https://doi.org/10.1111/1742-6723.12870
van Eck, C. F., van den Bekerom, M. P. J., Fu, F. H., Poolman, R. W., & Kerkhoffs, G. M. M. J. (2013). Methods to diagnose acute anterior cruciate ligament rupture: A meta-analysis of physical examinations with and without anaesthesia. Knee Surgery, Sports Traumatology, Arthroscopy, 21(8), 1895–1903. https://doi.org/10.1007/s00167-012-2250-9
Wang, J. H., Lee, J. H., Cho, Y., Shin, J. M., & Lee, B. H. (2016). Efficacy of knee joint aspiration in patients with acute ACL injury in the emergency department. Injury, 47(8), 1744–1749. https://doi.org/10.1016/j.injury.2016.05.025