I read around pacemakers SO often throughout my residency, but it was a topic that I found was often a struggle to absorb. So, here we’re going to tackle what the ED Physician should know about managing patients with pacemaker and ICDs:
- Pacemaker Basics
- Electrical Concepts
- Pacemaker Complications
- Dysfunctional Pacemakers
- Indications, complications and malfunctions of ICDs
Part 1 – Pacemakers 101
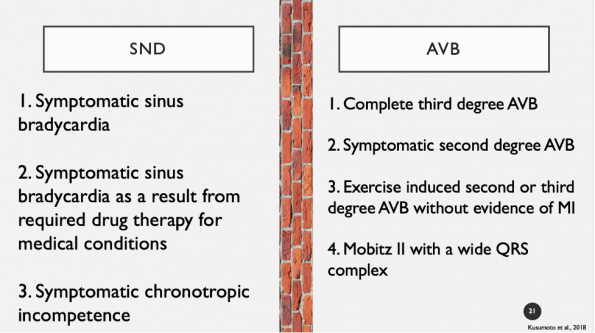
1. Indications for Pacemaker Implantation:
- Guidelines for pacemaker insertion have been established by a task force formed by the American College of Cardiology (ACC), American Heart Association (AHA), and the Heart Rhythm Society (HRS).
- They divide the indications for pacemaker implantation into 3 specific classes:
- Class 1: Conditions where implantation is necessary and beneficial
- Class 2: Conditions where they are indicated by there is conflicting evidence
- Class 3: Conditions where implantation is not recommended and may be harmful
- Below is a brief list of class 1 and 2 indications specifically sinus node dysfunction (SND) and AV blockade – which represent the vast majority of implanted pacemakers
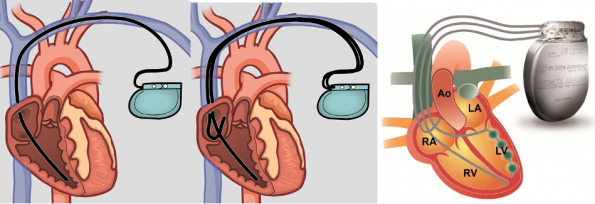
2. Types of Pacemakers
There are 3 main types of pacemakers:
- Single chamber system
- Single lead in either
- Right atrium – detect P waves
- Right ventricle (most common) – detects R waves
- This is rare to see
- Vast majority of patients will have a dual chamber system
- Single lead in either
- Dual chamber system
- Two leads
- One in the right atrium and one in the right ventricle
- Provides AV synchrony and pacing support in both atrium and ventricle
- Used in sinus node disease
- Two leads
- Triple chamber system
- Aka bi-ventricular pacemaker or Cardiac Resynchronization Therapy (CRT-P)
- Three leads
- Right atrium
- Right ventricle
- Left ventricle (via the coronary sinus vein)
- Paces both ventricles together to resynchronize the beat
- Used exclusively in certain types of heart failure with reduced ejection fraction
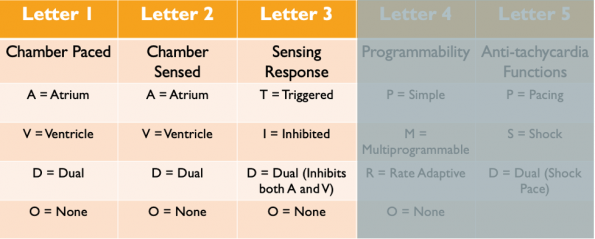
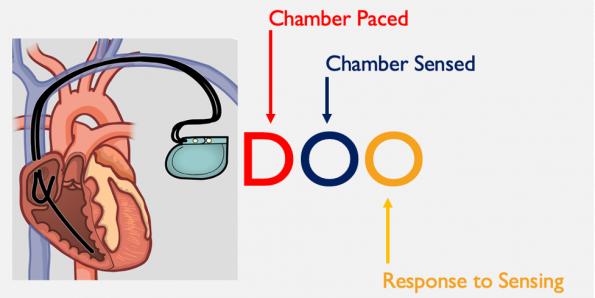
3. Pacemaker Code
- Pacemaker code is broken down into 5 letters
- These 5 letters tells us what the different pacemaker settings are and what the pacemaker can do
- First 3 letters are most relevant to us – we are only going to focus on those
- First letter: Chamber paced
- Second letter: Chamber sensed
- Third letter: Sensing response – that is, what the pacemaker does in response to a sense beat
- Triggered – occurs when there is no sense beat so the pacemaker will trigger an impulse (not used in current PPMs)
- Inhibited – occurs when an intrinsic depolarization is sensed which results in inhibition of the pacemaker
- Dual – dual inhibition of both atria and ventricular pacing in response to intrinsic ventricular depolarization
- None – does not trigger or inhibit regardless of native activity
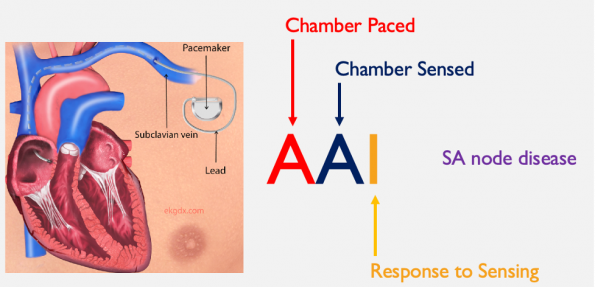
AAI
- Single lead system where the atria is both paced and sensed
- Response is to inhibit the pacemaker from firing
- If there is no intrinsic depolorization detected, this pacemaker will send an electrical discharge and cause atrial contraction
- These pacemakers are primarily used for sinus node disease and sinus bradycardia
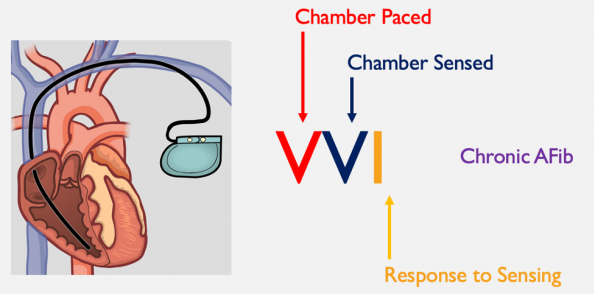
VVI
- Single lead system where the ventricle is both paced and sensed
- When ventricular depolorization is sensed, the pacemaker is inhibited from discharging
- If there is no sensed depolorization, the pacemaker sends an impulse down the lead to the RV causing ventricular contraction
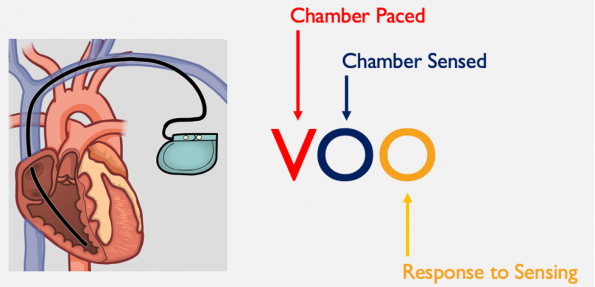
VOO
- Here the ventricle is paced with no sensing and thus no response to sensing
- Also called asynchronous pacing where the pacemaker will continuously depolarize at a set pre-programed rate regardless of intrinsic activity
- This is the default setting for all single chamber pacemakers
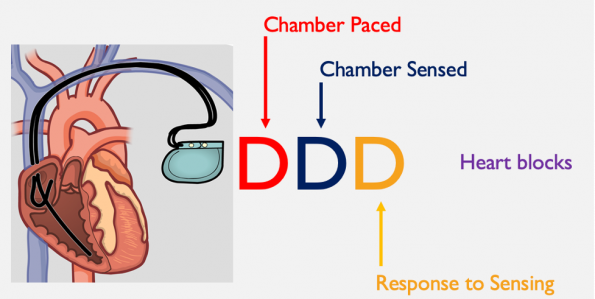
- Here both atria and ventricles are paced and sensed
- There can be a combination of atrial sensing or pacing or ventricular sensing or pacing
DOO
- This is the default setting for dual chamber pacemakers and the setting when a magnet is applied
- Equivalent to VOO for single system pacemakers
Components of a Pacemaker
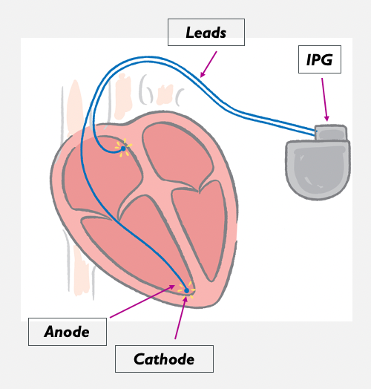
- Implantable pulse generator (IPG)
- Delivers an electrical charge down the lead to the heart which triggers a heartbeat
- To do this there needs to be a battery, sensing circuit, and microprocessor
- These components are housed within the IPG
- Sensing circuit
- This detects any naturally occurring electrical activity and brings this information to the microprocessor
- Microprocessor
- Brain of the pacemaker that controls what the pacemaker does in response to sensing
- Connectors
- Leads
- These connect the pacemaker to the heart muscle itself
- Function of leads
- Delivers electrical impulses from the pulse generator to the heart
- Senses cardiac depolarization
- Leads are fixed into the myocardium
- Electrodes are implanted on fixation ends
- Unipolar vs bipolar leads
- Most leads have two electrodes
- Can alter whether one is used (unipolar) or both are (bipolar)
- Unipolar pacing system
- One electrode (cathode) at the tip
- IPG functions as the anode
- With pacing
- Impulse flows through the electrode tip
- Stimulates the heart
- Returns through cardiac or body tissue to the IPG
- Bipolar pacing system
-
- Lead has both an anode and cathode
- With pacing
- Impulse flows through the electrode tip (cathode)
- Stimulates the heart at the electrode tip
- Travels to the ring electrode (anode) which is a few inches from the lead tip
- Returns to the IPG via the lead wire
-
- Most leads have two electrodes
- Important to know what type of lead is implanted because it can be helpful for diagnosing a problem and determining solutions
Part 2: Electrical Concepts
- Physics 101
- Ohm’s law
- V=IR
- Voltage – potential difference between two electrodes
- Provided by PPM battery
- Can also be referred to as amplitude
- Current – the flow of electrons through a completed circuit
- Calculated by the voltage that is programed and the impedance of the pacing system
- Impedance – resistance to current flow
- For our sake this is the same thing as resistance
- High impedance occurs with lead fractures or displacements
- Low impedance occurs with breaks in insulation
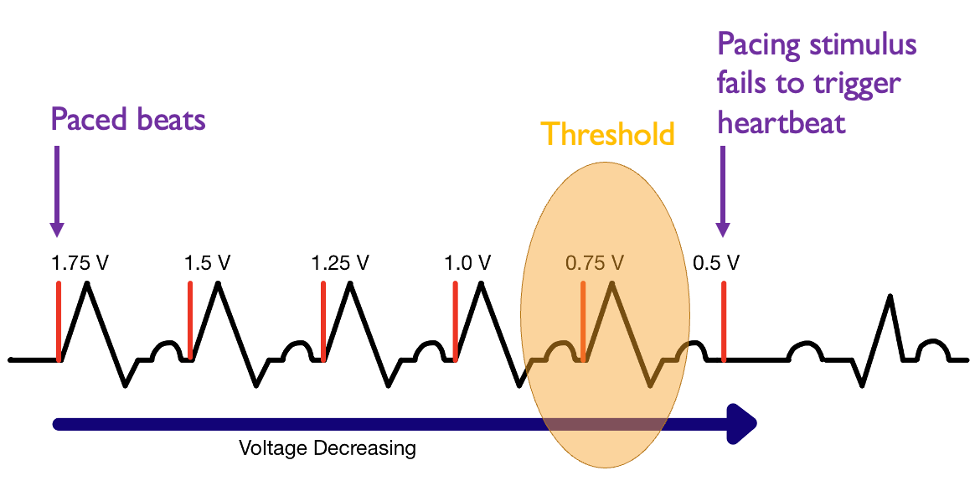
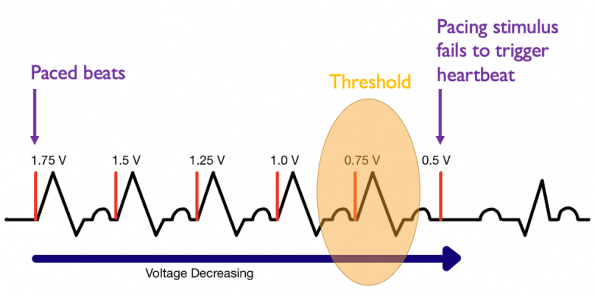
- Capture and Threshold
- Capture: The minimum electrical stimulus needed to consistently capture to trigger a heartbeat
- Dependent on both voltage and pulse width
- Threshold: the minimum electrical stimulus needed to trigger a heartbeat, regardless of consistency
- Capture: The minimum electrical stimulus needed to consistently capture to trigger a heartbeat
- For our sake this is the same thing as resistance
- Here we see paced beats at 1.75 volts
- As we slowly decrease the voltage to 0.5 volts we no longer see ventricular contractions
- 75 volts was the amount of voltage needed to get a ventricular contraction – this is the threshold
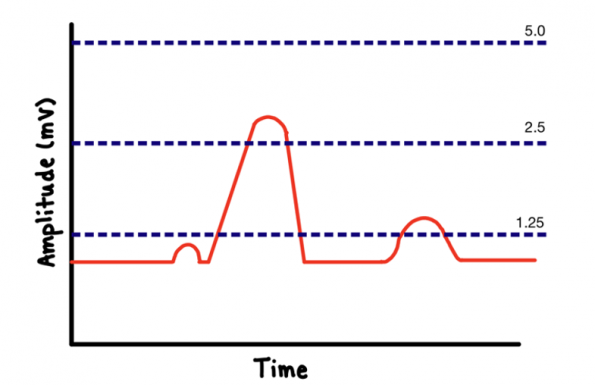
- Sensing
- Is the ability of the pacemaker to detect whether or not the heart is beating
- If the pacemaker receives an intrinsic electrical signal, it will be satisfied that the heart just contracted
- If it did not receive a signal, it will assume that the heart has failed to beat when it should have and would initiate an impulse
- On the above graph, we have programed out pacemaker to have a maximum sensitivity of 2.5 mV
- If we increased our sensitivity above 2.5 mV, the pacemaker would not see intrinsic activity and would initiate impulses
- If we decrease our sensitivity below 2.5 mV, the pacemaker would see more incoming signals and would not initiate impulses
- Adequate sensitivity is important
- Filters out extraneous signals
- T waves
- Skeletal muscle myopotentials
- Sensing accuracy affected by
- Pacemaker lead integrity
- Insulation break
- Wire fracture
- Electrode placement within the heart
- Electrophysiologic properties of the myocardium
- Electromagnetic interference
- Pacemaker lead integrity
- Filters out extraneous signals
- Role of Magnets in Pacemakers
- Magnets can be placed over pacemakers to facilitate interrogation or troubleshooting
- For us, as emergency physicians, we place magnets over pacemakers when the pacemaker is malfunctioning
- This changes the pacemaker to asynchronous mode
- VOO or DOO
- Pacemaker here will pace at a rate of 85 beats per minute regardless of intrinsic cardiac activity
When the magnet is removed, the pacemaker returns back to its programmed operation within 2 seconds.
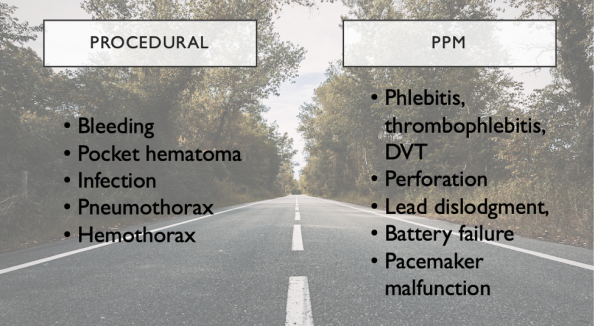
Part 3: Pacemaker Complications
- Complications can arise at any time following device implantation
- This can be directed from the procedure itself or a complication of the pacemaker
- Bleeding occurs in 3% of patients
- Most hematomas can be treated with a local compressive dressing
- A pocket hematoma (above), should not be drained in the ED as there is an increased risk for infection
- This warrant a cardiology consultation
- Pocket infections or systemic infections occur in 1-3% of patients
- These warrant a cardiology consultation as these patients often require IV antibiotics and device removal
- Lead displacement or perforation
- This is fairly common occurring in 5% of patients
- Leads may perforate through the myocardium
- An ECG may show evidence of failure to capture
- A chest XR may be helpful in visualizing the fracture or displacement
Part 4: Dysfunctional Pacemakers
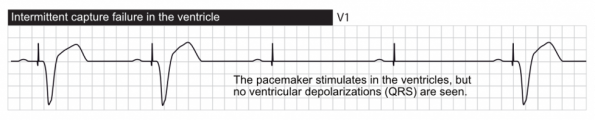
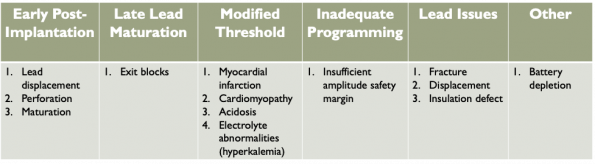
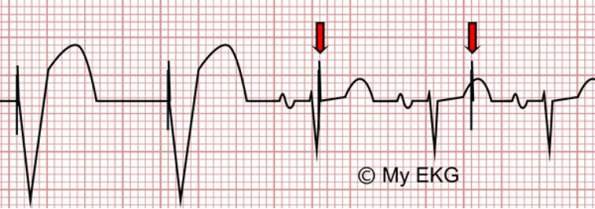
1. Failure to Capture
Electrical stimulus does not result in depolarization of the myocardium
- ECG: shows pacemaker spikes throughout the strip
- Some are followed by QRS complexes and others are not
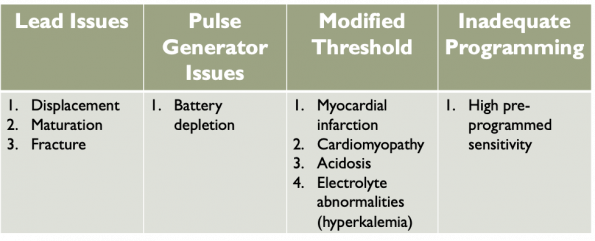
- Causes:
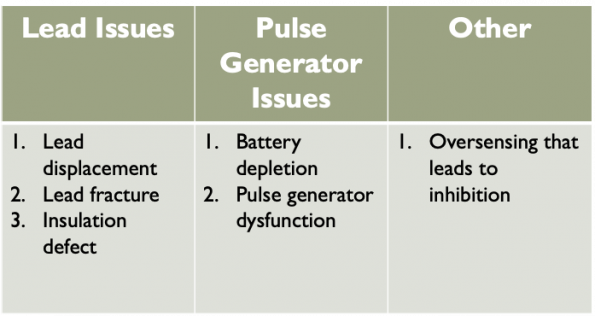
2. Failure to Pace
- No paced stimulus is generated from the device resulting in either decreased or absent pacemaker function
- ECG: shows decreased or no pacer spikes or pacer-induced QRS complexes but rather the native rhythm
- Causes:
3. Undersensing
- This occurs when the pacemaker does not see the intrinsic beat and thus delivers a scheduled pace
- Undersensing = overpacing
- ECG: shows pacer spikes within the QRS complexes
- Causes:
4. Oversensing
- Here the sensitivity threshold is set too low, so electrical signals are inappropriately recognized as native cardiac activity and pacing is inhibited
- Oversensing = under-pacing
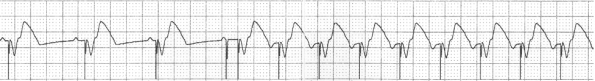
5. Pacemaker Mediated Tachycardia (PMT)
- Ventricular depolorization conducts backwards into the atria leading the atrial lead to detect activity as an incoming p wave resulting in ventricular depolorization
- Paced ventricular complex then results in further retrograde conduction with retrograde p wave generation thus forming a continuous cycle
- For sequence to be maintained
- AV node and atrium need to be able to conduct retrograde
- Pacemaker must be able to sense this retrograde depolarization
- Similar to a re-entrant tachycardia with the pacemaker forming part of the re-entrant circuit
- Treatment
- Magnet application
- If this was truly PMT, the tachycardia would be instantly abated
- AV blocker – Adenosine, BB, CCB
- Magnet application
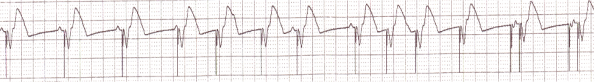
6. Runaway Pacemaker
- Seen in older generation pacemakers
- Results from low battery voltage
- Pacemaker delivers runs of spikes in excess of 200 bpm which can provoke VF of cause FTC causing bradycardia as the pacing spike are low in amplitude
- Today pacemakers have security designed to prevent runaway
- Maximum rate, hermetic sealing and a decrease in pulse amplitude at high rate with concomitant loss of capture
- ECG shows intermittent ventricular capture at a rate slower than normal with numerous spikes at a very high rate with different voltages and often without capture beats, simulating an ECG artifact
- Treatment
- Apply magnet
- Replace pacemaker
7. Pacemaker Induced Extra-Cardiac Stimulation
- Diaphragmatic stimulation
- Lead close to phrenic nerve
- Lead incorrectly positioned
- Cardiac vein, myocardial perforation, migration
- Pectoralis muscle
- Intercostal muscle
8. Twiddler’s Syndrome
- Occurs when the patient self-manipulates the pulse generator that is implanted in the skin
- Causes the pulse generator to rotate on itself which subsequently pulls on the leads and displaces them
- Can result in extra-cardiac pacing
- These need to be replaced
Part 5: Approach to the Dysfunctional Pacemaker in the ED
There are a variety of tools that we can use at our disposal to diagnose and manage dysfunctional pacemakers in the ED
- Patient history and physical exam
- PoCUS
- Pacemaker device card
- Provides details on who implanted the device, indication, manufacturer, type, model and date of implantation
- Cardiac Device Check (this is specifically under the Media tab in Epic)
- 12-lead ECG +/- a rhythm strip
- CXR
- Leads – number, kinks, fractures, displacement
- Assess the pulse generator location
- Assess for the presence of a pneumothorax and/or hemothorax
- Compare to previous CXR
- Blood work – electrolytes, VBG and lactate, TSH, Digoxin level (if appropriate)
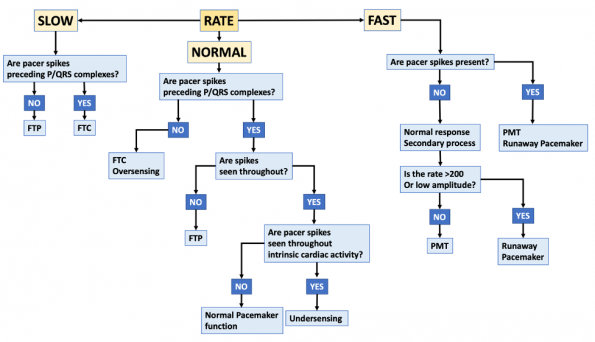
- Below is an approach to interpreting an ECG
- If the patient is unstable, proceed down standard ACLS
- Consider magnet application
- Cardiology consultation for device interrogation and troubleshooting




Excelente artículo. Y practico. Gracias!