Drug rashes are fairly common, but like much of dermatology, diagnostic clarification can be hard to achieve. Here, we present a standardized approach to drug rashes in the Emergency Department.
Differential Diagnosis
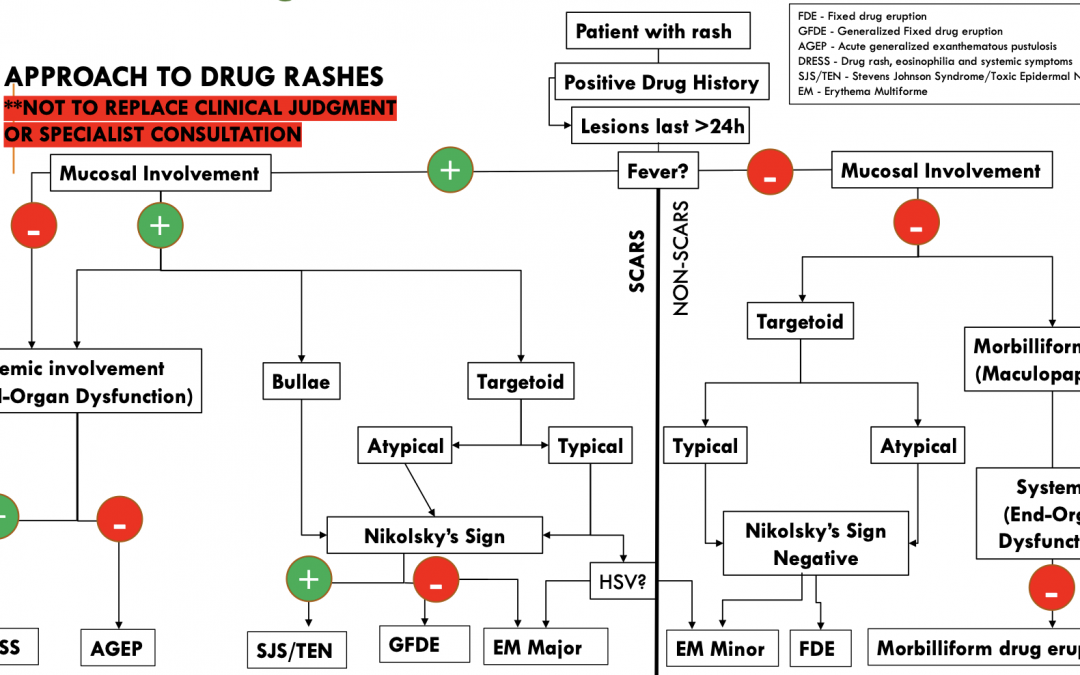
Clinical Approach
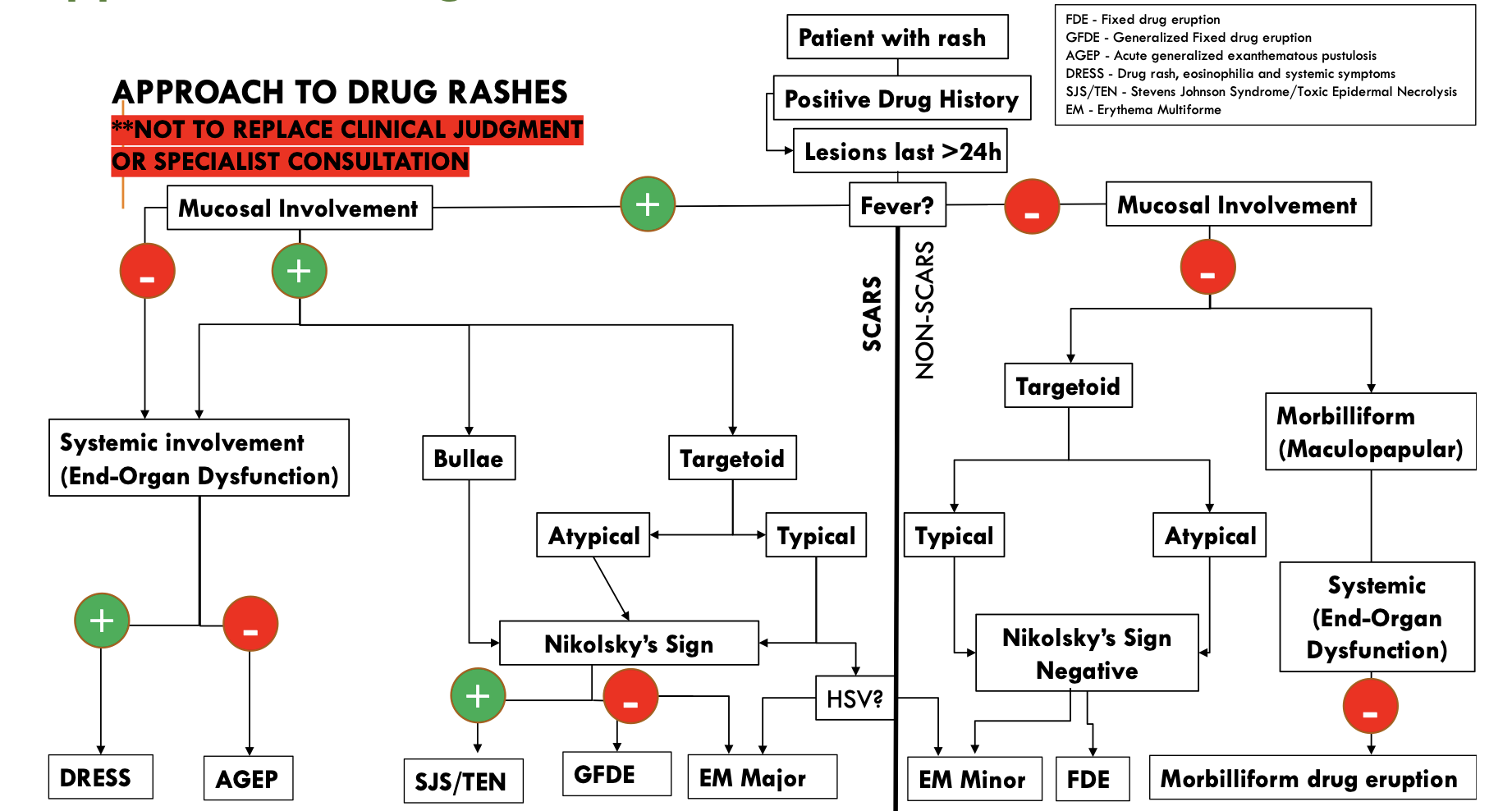
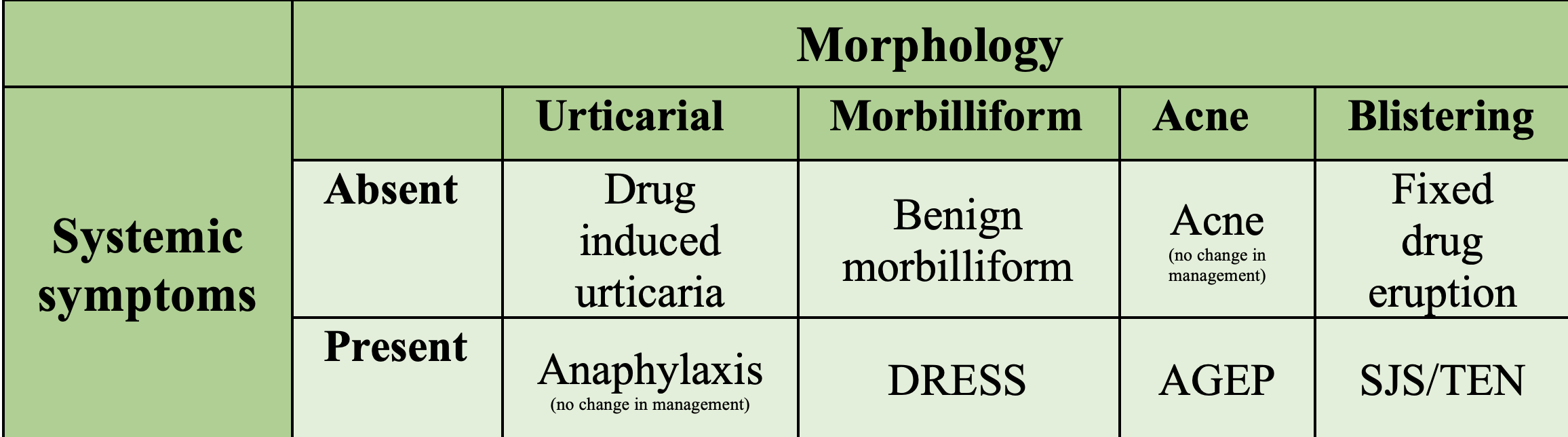
Figure 1. Figure created by Dr. Reetesh Bose (Dermatology, University of Ottawa); Included with permission. Note: This does NOT replace clinical judgement or specialist consultation.
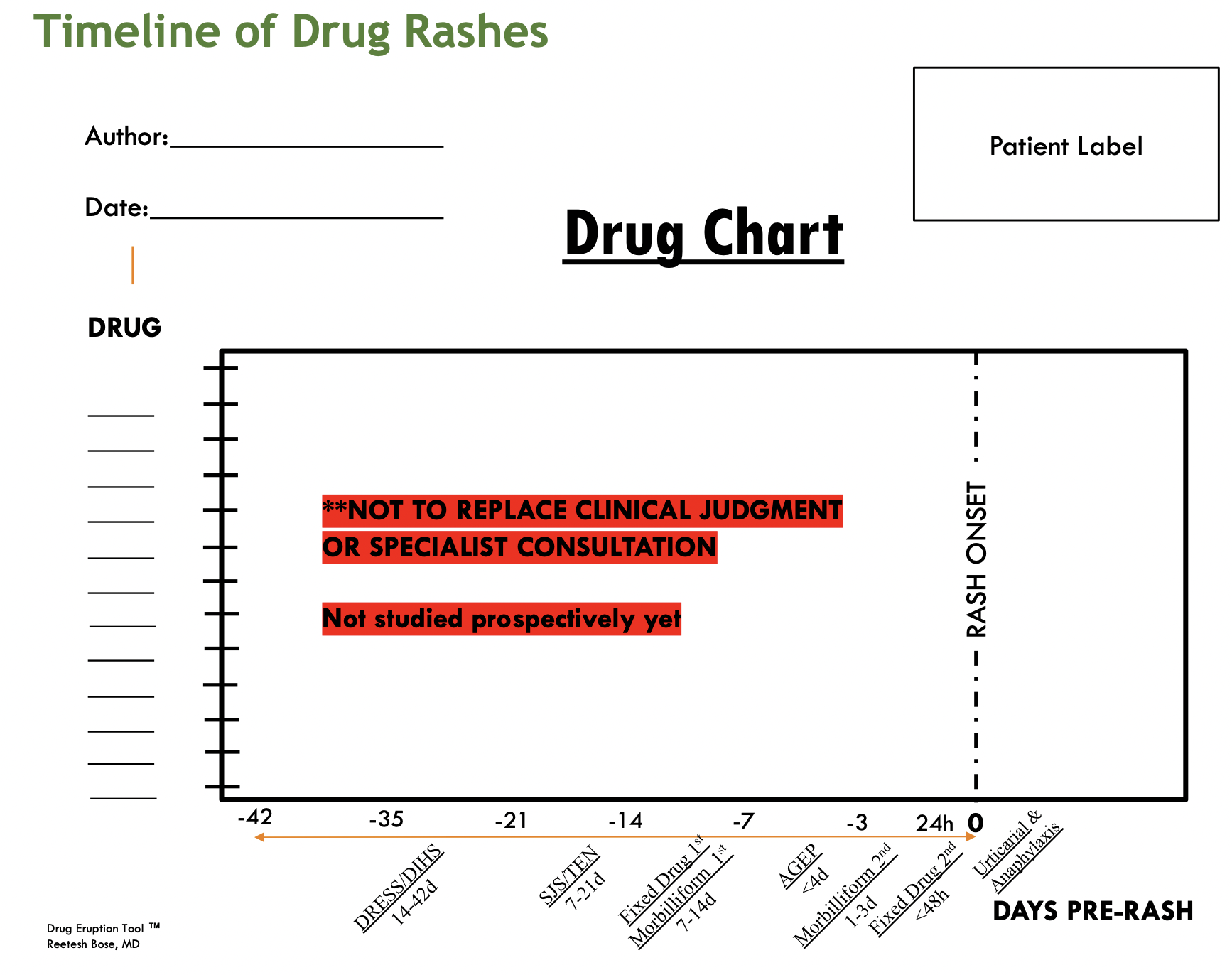
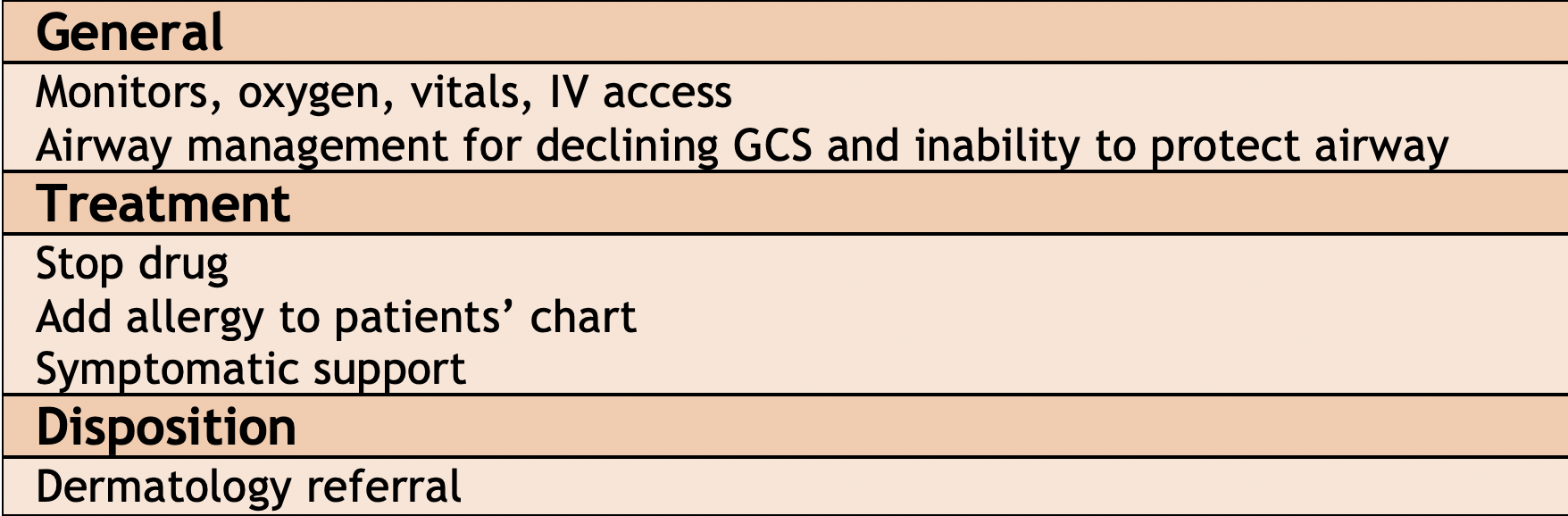
Figure 2. Drug Eruption Tool ™ created by Dr. Reetesh Bose (Dermatology, University of Ottawa); Included with permission. Note: This does NOT replace clinical judgement or specialist consultation.
Assessment
History
Distribution and progression, recent exposures, new meds
Physical Exam
Dangerous features: abnormal vital signs; full examination of patient including palms/soles/mucous membranes; touch skin with gloved hand to determine if raised/flat; press on lesions to see if it blanches; rub erythematous areas to see if it peels
Investigations (if systemic symptoms present)
- Labs:LFT’s, Cr, UA, CK, CBC, lactate+VBG, TSH, glucose
- Imaging: CXR
- Other: ECG, +/- ECHO
Management
Specific Conditions
1. Drug Induced Urticaria

Figure 3. Images taken from DermNet NZ (https://creativecommons.org/licenses/by-nc-nd/3.0/nz/legalcode
Rash: Widespread wheals, pruritic
Timeline: Occurs soon after drug ingestion
Mangement:
- Stop the drug; Cool the area with a fan, ice pack or refrigerated moisturizing lotion
- Use a non-sedating, second-generation antihistamine
- Example prescription for cetirizine
- Take 10mg PO OD x2 weeks
- If rash persists or is relapsing/remitting, then increase intermittently up to 4x the base dose (max 20mg BID)
- Once rash is well controlled then stay on the dose that controlled the rash for 2 weeks (maintenance dose)
- After being on maintenance dose, taper down the cetirizine every two weeks
- Take 10mg PO OD x2 weeks
- Add allergy to medical chart; advise patient to avoid causative drug; Consider medical alert bracelet and epinephrine
- Example prescription for cetirizine
- Follow up:
- Family physician is symptoms don’t resolve, or referral to Allergy and Immunology for consideration of prick testing or alternative therapy
- Can also consider referral to Dermatology if not responding to initial therapy, or if atypical presentation
2. Benign Morbiliform Reaction
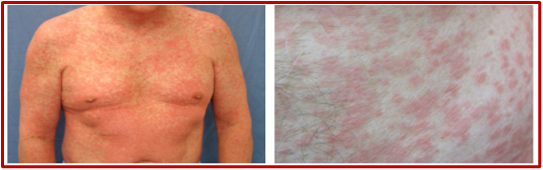
Figure 4. Images taken from DermNet NZ (https://creativecommons.org/licenses/by-nc-nd/3.0/nz/legalcode)
Risk Factors: Family history of drug eruptions; underlying viral infections; immunodeficiency; multiple medications
Timeline: occurs 1-2 weeks after starting a new drug, can occur 1 week after stopping drug; on re-exposure rash can occur within 1-3 days; rare for a drug used >3 months to be culprit drug
Rash: Many morphologies, but commonly: erythematous macules, papules, coalescing into patches and plaques; Mucous membranes, hair, nails, are typically not affected; Usually starts on trunk and spreads to limbs
How to Make the Diagnosis: new drug + classic rash; Investigations can show eosinophilia; Investigations should be considered if patient has vital sign abnormalities or extensive involvement
Management:
- Stop the culprit drug
- Once drug is stopped, the rash begins to improve within 48hrs and clears within 1-3 weeks
- Wet wraps for red, inflamed skin and oral antihistamines can help with sleep and itch
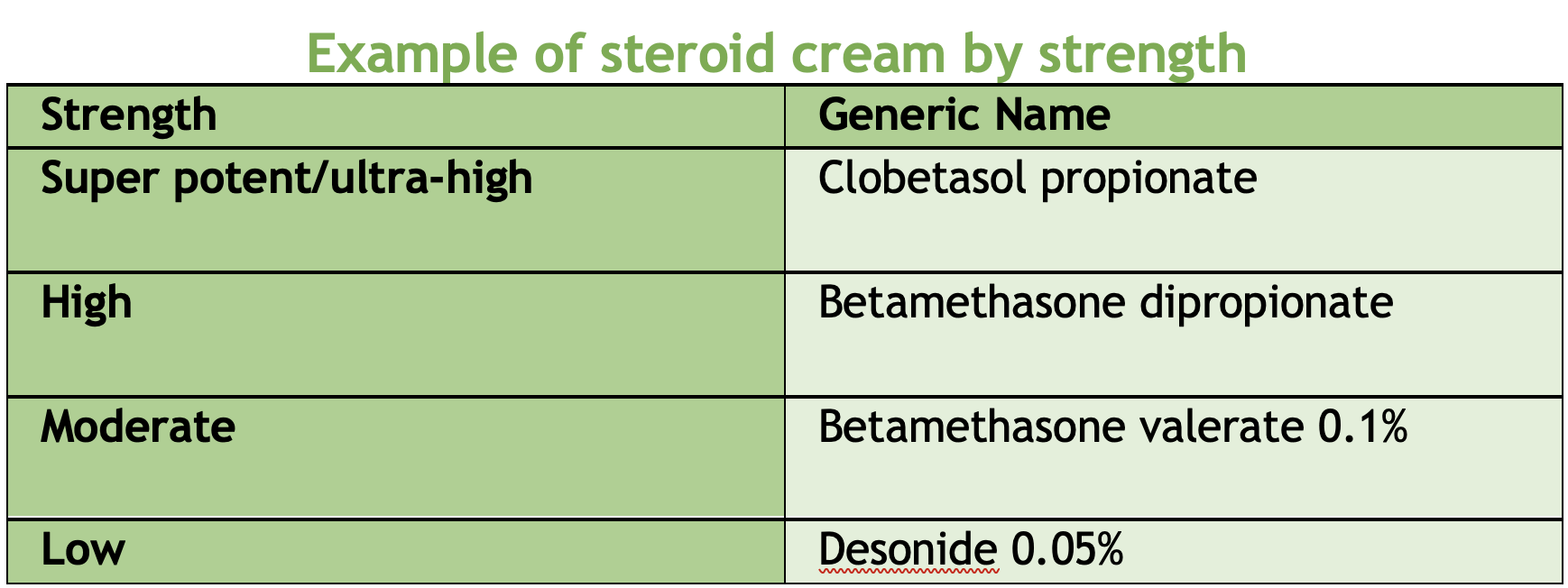
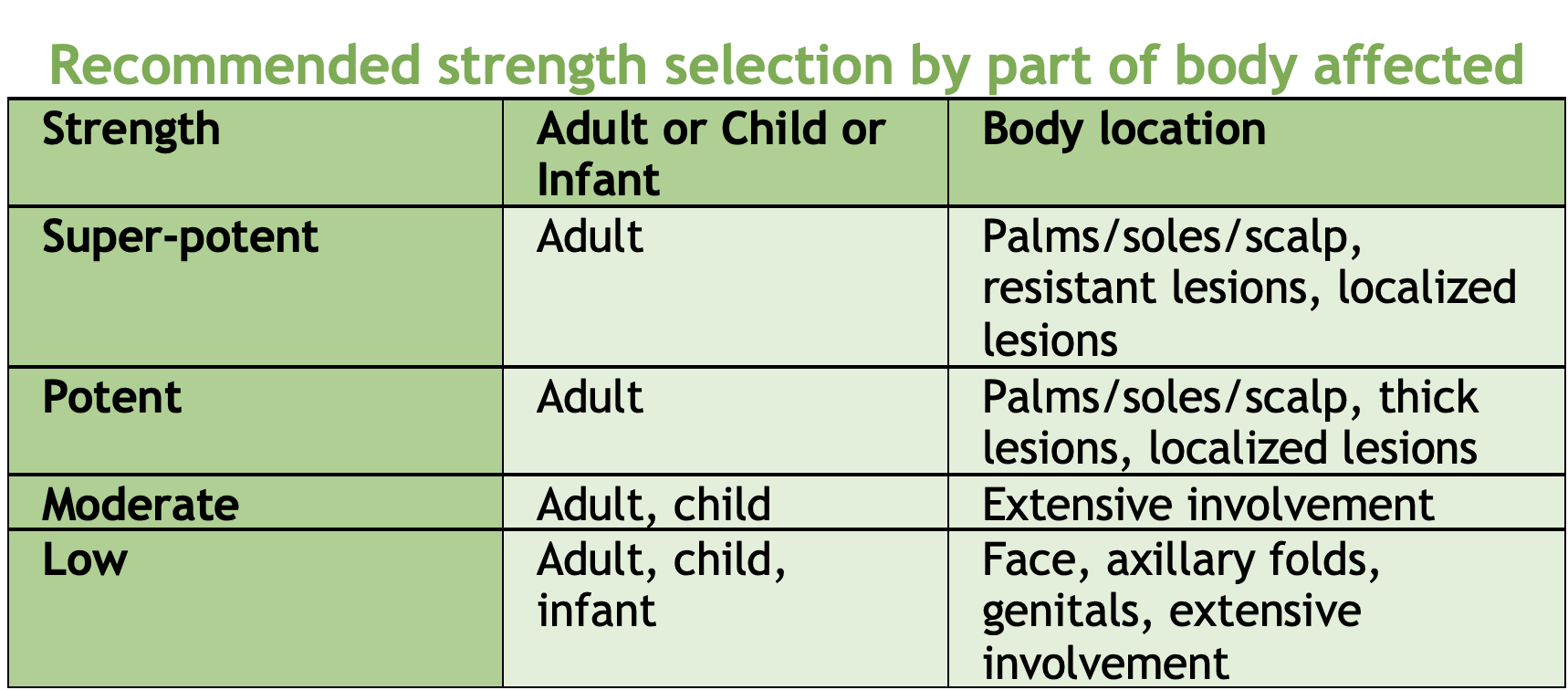
- For symptomatic rashes (i.e., pruritic, burning) – apply emollients or topical steroid creams twice daily
- List allergy in patient’s medical chart
- Follow up: GP
- Prognosis: Usually completely resolves, sometimes have post-inflammatory hyperpigmentation
3. Fixed Drug Eruption

Figure 3. Images taken from DermNet NZ (https://creativecommons.org/licenses/by-nc-nd/3.0/nz/legalcode)
Risk Factors: Family history of drug eruptions; underlying viral infections; immunodeficiency; multiple medications
Timeline: occurs 1-2 weeks after starting a new drug
Rash: Can be single or multiple lesions; Patches or plaques; Can develop vesicles/bullae; Itchy or painful, but can be asymptomatic
Areas affected: Hands and feet, eyelids, and oral mucosa, anogenital areas; In females, typically effects extremities; In males, typically affects the genital area
Subtypes:
- Localizing pigmenting type: One lesion that leaves hyperpigmentation once resolves;
- Bullous: Less common, May be associated with fever, malaise, arthralgia, Develops post-inflammatory hyperpigmentation, May need burn or ICU unit care;
- Mucosal: Lips, tongue, hard palate, genitalia,
- Non-pigmenting: Most common cause is pseudoephedrine, Non-pigmenting lesion that does not leave hyperpigmentation;
- Generalized: Generalized lesions that can be targetoid or patch
Management: Stop the drug; avoid the drug in the future; List allergy in patient’s medical chart; Topical or systemic steroid for symptomatic rashes; Generalized bullousmay require ICU or burn unit care+typically requires admission or close monitoring
Follow up: Can consider referral to dermatology for diagnostic clarity (e.g., biopsy, patch testing)
4. DRESS

Figure 4. Images taken from DermNet NZ (https://creativecommons.org/licenses/by-nc-nd/3.0/nz/legalcode)
Risk Factors: genetic susceptibility; reactivation of HHV 6, HHV 7, EBV or CMV
Timeline: occurs 2-8 weeks after starting a new medication
Common drugs: anticonvulsants, allopurinol, olanzapine, sulfa
Rash: High fever followed by rash; Morbilliform – 80% of patients; Facial swelling – 30% of patients; Mucosal involvement – 25% of patients; Lymphadenopathy
Investigations: LFT’s, Cr, UA, CK, CBC, lactate + VBG (Blood work may show: Eosinophilia, Elevated LFT’s (x3 ULN), Elevated Cr), TSH, glucose, ECG, ECHO, CXR
Management: Stop causative medication; Add allergy to patient’s medical record; In ED referral to dermatology; Blood tests as soon as possible; Supportive treatment (Dressings, Emollients); Medical treatment (in consultation with dermatology): Topical corticosteroids; Systemic corticosteroids (e.g. prednisone, IV methylprednisolone); Cyclosporine; Intravenous immunoglobulin
Future considerations: Cross-reactions are common among phenytoin, carbamazepine, phenobarbital, lamotrigine thus patients must avoid all four; First degree relatives are at risk
5. AGEP

Figure 5. Images taken from DermNet NZ (https://creativecommons.org/licenses/by-nc-nd/3.0/nz/legalcode)
Timeline: within 4 days of exposure
Rash: Pustular rash rapidly starts on face/armpits/groin and then spreads throughout the body; Most prominent in skin folds; 50% of the time there is mucosal involvement; Facial swelling is common; Fever can occur
Investigations: LFT’s, Cr, UA, CK, CBC, lactate + VBG, CRP/ESR, (Blood work may show: neutrophilia, eosinophilia, raised ESR/CRP, renal and/or hepatic abnormalities), TSH, glucose
Management: Most important factor in the ED is to recognize it as it is rare; Discontinue new meds; Supportive treatment; Add allergy to patient’s medical record
Future considerations: Rash resolves in ~10 days; Can recur with re-exposure to same medication and second episode may be more severe
6. SJS/TEN

Figure 6. Images taken from DermNet NZ (https://creativecommons.org/licenses/by-nc-nd/3.0/nz/legalcode)
Investigations: LFT’s, Cr, UA, CK, CBC, lactate + VBG (Blood work may show anemia, leukopenia, lymphopenia, neutropenia, electrolyte abnormalities), TSH, glucose, woundswabs, and blood cultures
Management:
The only two things done in the ED that have the most positive impact on the patient is:
- Discontinue the drug
- Consult dermatology and admit to burn center or ICU
‘Cherry on top’ treatment to think about
- Warm ambient room temperature
- Pain relief (consider PCA)
- Sterile handling and reverse isolation procedure
- Swab + culture 1 or 2 desquamated areas
- Aim for urine output 0.5 – 1 cc / kg / hr
If febrile
- Do blood cultures
- Do not start antibiotics unless convinced there is an infection
Treatments in dermatologist’s arsenal (do not order without consultation)
- IVIG
- Cyclosporin
- Etanercept
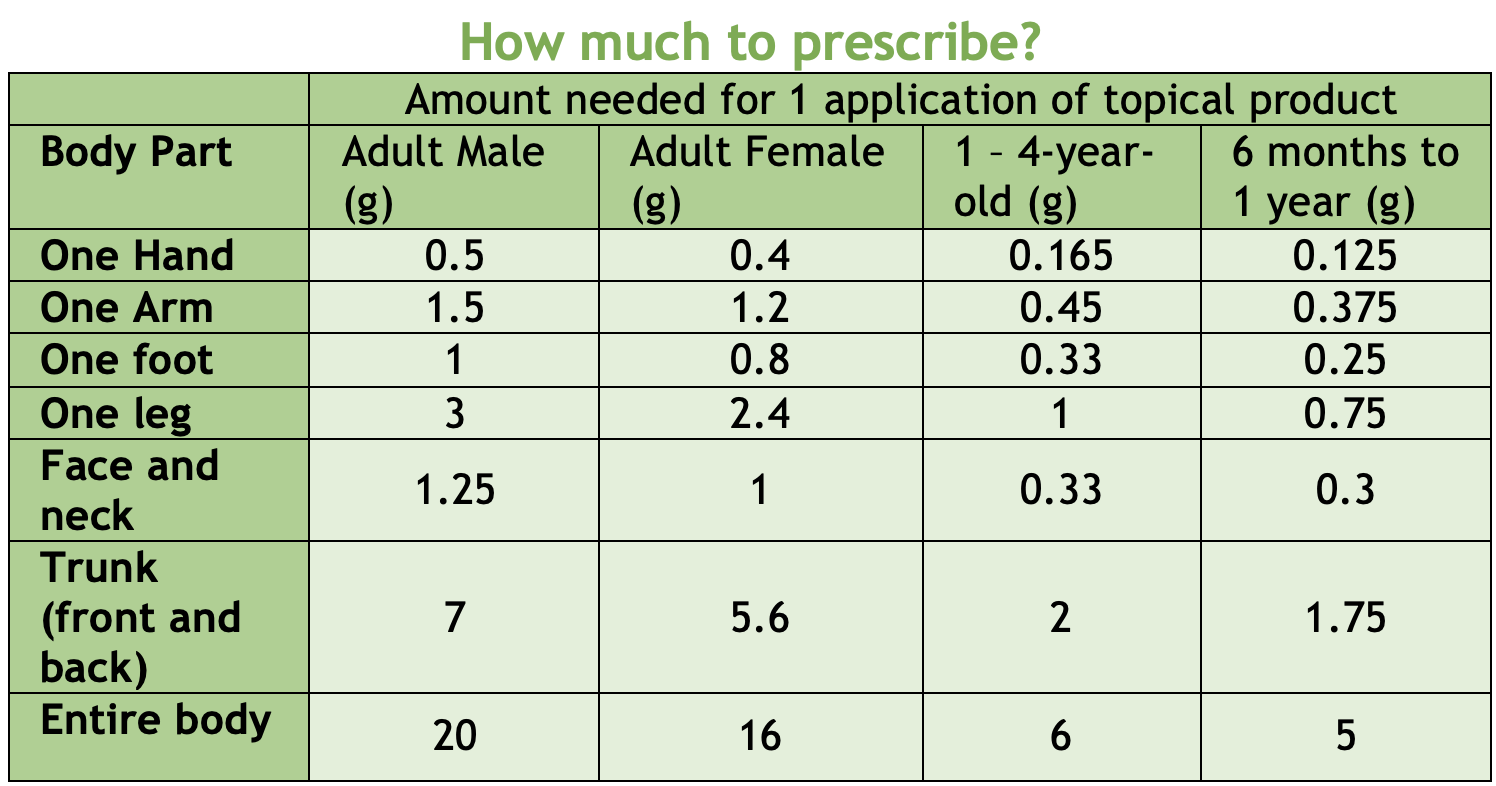
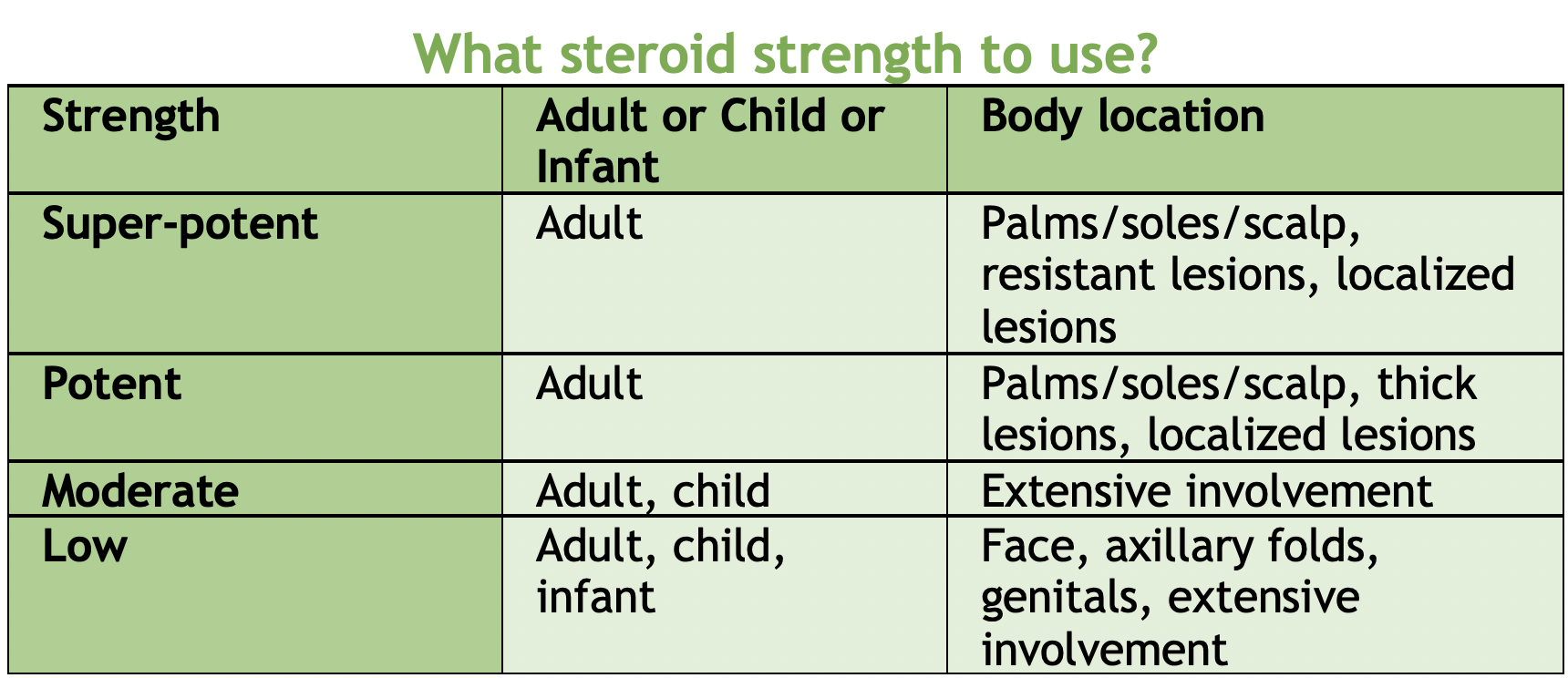
BONUS: Steroid Creams
References
1.Shipley, D. & Ormerod, A. D. Drug-Induced Urticaria: Recognition and Treatment. American Journal of Clinical Dermatology 2, 151–158 (2001).
2.Hoetzenecker, W. et al. Adverse cutaneous drug eruptions: current understanding. Semin Immunopathol 38, 75–86 (2016).
3.Anderson, H. J. & Lee, J. B. A Review of Fixed Drug Eruption with a Special Focus on Generalized Bullous Fixed Drug Eruption. Medicina (Kaunas) 57, 925 (2021).
4.Shiohara, T. & Mizukawa, Y. Drug-induced hypersensitivity syndrome (DiHS)/drug reaction with eosinophilia and systemic symptoms (DRESS): An update in 2019. Allergology International 68, 301–308 (2019).
5.Szatkowski, J. & Schwartz, R. A. Acute generalized exanthematous pustulosis (AGEP): A review and update. Journal of the American Academy of Dermatology 73, 843–848 (2015).
6.Lerch, M., Mainetti, C., Terziroli Beretta-Piccoli, B. & Harr, T. Current Perspectives on Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clinic Rev Allerg Immunol 54, 147–176 (2018).
7.Jacobsen, A. et al. Systemic interventions for treatment of Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and SJS/TEN overlap syndrome. Cochrane Database of Systematic Reviews 2022, (2022).
8.Oakley, A. Fingertip unit. DermNetZ https://dermnetnz.org/topics/fingertip-unit (2001).


This is a wonderful post, and I am will certainly reference it many times in the future, however it doesn’t address what I think is the real difficulty for clinicians: How do I know the rash is drug related? If the patient is on a drug, especially a new drug, the rash could just as easily be related to the underlying condition that prompted that new drug, or something completely unrelated. Any tips on making that distinction, or thoughts on making a similar algorithm that doesn’t include the assumption that the rash is drug related?