Note: This grand rounds presentation and summary had contributions from Dr. Anne-Marie Abe, a neuropsychiatrist specializing in functional neurological disorders in Ottawa.
Patients living with functional neurologic disorders (FND) have been deeply stigmatized by the medical system. In a patient survey by FND Hope (an international organization for the research and advocacy around FND) 82% of patient respondents felt they had been treated poorly due to stigma relating to their FND diagnosis, primarily by emergency physicians [1]
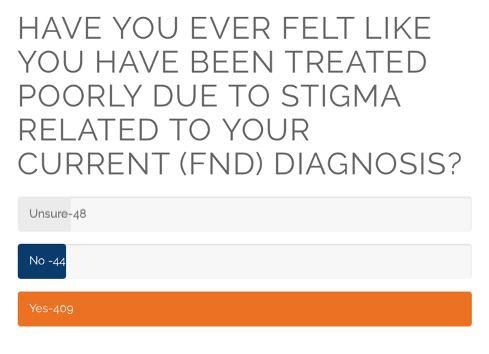
FND Hope
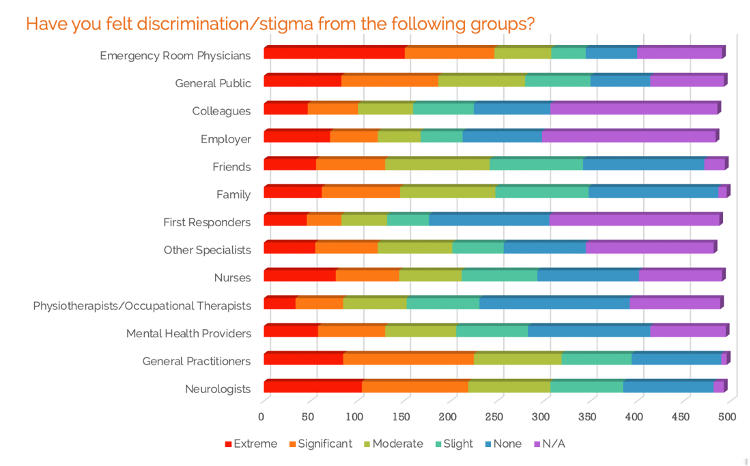
FND Hope
There are likely multiple contributing factors to these challenges from an ED provider perspective, ranging from the time constraints we face in patient care, a lack of concrete emergent treatment options for FND, and a lack of prior education on FND. A study out of Cleveland Clinic in Ohio demonstrated that 95% of EM providers noted a knowledge gap relating to FND. [2]
This is a significant deficit as EM physicians have the potential to play a vital role in the diagnosis and timely management of patients with FND.
-
- EM physicians can assess for comorbid structural neurological conditions
- EM physicians can refer a patient to appropriate outpatient therapies, bypassing prolonged wait times for an outpatient neurology consultation
- An earlier diagnosis is associated with improved prognosis [3]
- An earlier diagnosis is associated with decreased ED return-to-care visits [4]
What is Functional Neurologic Disorder (FND)?
FND is described by [5,6]:
- A disorder of brain-body connection
- Neurological symptoms that do not follow a pattern of known disease
- Inconsistent signs and symptoms without evidence of organic disease on investigation
- Is involuntary and not caused by malingering or factitious disorder
- Reliable findings on fMRI with stress-mediated neuroplasticity
FND is a common disorder [7,8,9]:
- The incidence of FND in the general population is comparable to the prevalence of MS in Canada.
- FND is the second most common reason for referral to outpatient neurology clinics.
- Present in up to 30% of people with a diagnosed neurological disorder followed by outpatient neurology.
- Functional seizures make up 10-26.5% of all seizures seen in the ED, as well as 25% of refractory status epilepticus.
History and Causes:
FND has no one cause or predisposing factor.
You may have heard of FND being referred to as “stress-induced” or “psychosomatic”, however many patients with FND have no single identifiable stressor or pre-existing psychiatric condition. This is why the DSM-5 no longer contains a preceding stressor as a diagnostic requirement [10].
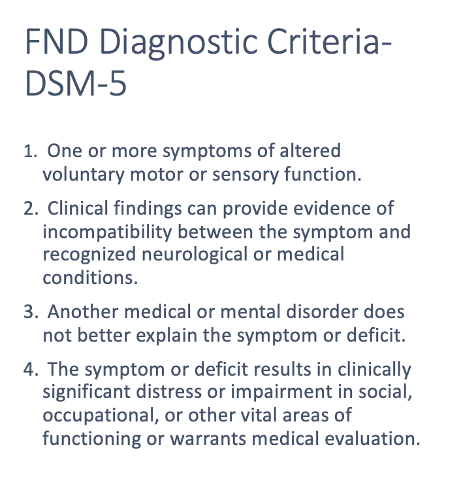
Figure 3. DSM Criteria for Functional Neurological Disorder [10]
FND can be caused by a physical or psychological insult to a brain which is vulnerable to developing a functional disorder.
Some predisposing factors for FND include:
-
- Pre-existing neurological condition
- Female sex
- History of stress or trauma
- History of sexual abuse (specifically in women)
- Pre-existing psychiatric condition
In Dr. Abe’s practice, some additional characteristics that she sees in her patients include:
-
- Anxiety
- Perfectionism
- Post viral syndrome
- Chronic fatigue
- Injury with prolonged recovery period (for example post-concussion syndrome)
On history, patients with FND will typically describe their symptoms as:
-
- Sudden onset
- Persistent or intermittent
- Fluctuating in intensity
- Worse with anxiety or pre-occupation
- Better with distraction or re-direction
- Potentially related to a specific stressor
Despite the fluctuance some patients may describe in their symptoms, the patient does not have voluntary control over them.
While we should consider whether a patient’s presentation may be related to feigning or malingering, a patient with unexplained neurologic symptoms is more likely to have a functional disorder rather than feign their symptoms. [11]
Functional Neurologic Disorder subtypes
FND symptoms can be categorized into four main subtypes which can have cross-over:
-
- Motor
- Sensory
- Movement
- Seizure
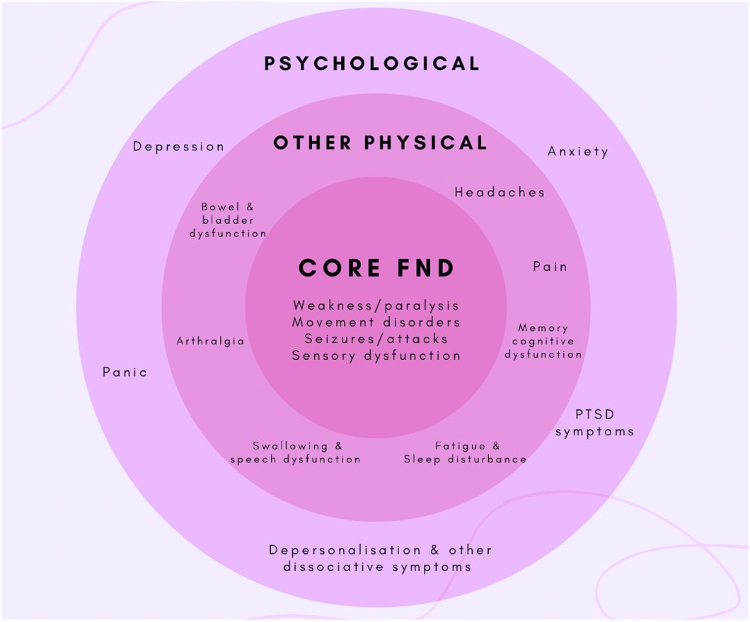
Figure 4. FND Signs and Symptoms [12]
Physical Exam
One misconception of FND is that it is often considered to be a diagnosis of exclusion, however, FND is a diagnosis with positive physical exam features.
The FND physical exam typically demonstrates:
-
- Positive physical exam findings
- Distractibility of findings
- Inconsistency of findings
Here is a breakdown of the common positive physical exam findings for FND:
| Subtype | Description | Physical Exam Findings |
| Motor | Weakness or paralysis |
|
| Sensory | Numbness, tingling, sensory deficit |
|
| Movement | Difficulty with coordination, tremor, gait |
|
| Seizure | Episode of impaired reactivity to external stimuli, episode of abnormal body movements/control |
|
Let’s review some videos and images that demonstrate the above physical exam findings:
Hoover Sign:
Give Way Weakness:
Giveaway weakness is also often present in FND. The patient initially demonstrates good strength in their affected limb which goes away with ongoing movement. Remember that give-way weakness can also be pain mediated to make sure to ask your patients if they are in pain during the examination.
Arm Drift without Pronation:
Arm drift without pronation describes a dropping of the arm due to weakness without the typical finding of preserved supinator strength from a UMN lesion. It is more likely to be present in FND.
Dragging Monoplegic Leg:
A dragging monoplegic leg can be present in functional weakness and is a finding of inconsistent weakness. Patients with an upper motor neuron lesion compensate by using their hip muscles and body positioning. A patient with FND has preserved strength in their quadriceps and can drag their foot forward as part of their gait.
Platysmal Hyperactivity:
Platysmal hyperactivity is a sign that facial droop is related to FND. You may notice a deviation of the mouth, rather than a pure droop as well as tension and activation of the platysma muscle on the affected side of the neck.
Inconsistency in Weakness:
Finally, Inconsistency of weakness is an important finding in FND-related motor weakness. As an example, a patient may not be able to plantarflex their feet while lying supine but be able to stand on their tiptoes. Additionally, a patient may have limb weakness that improves as part of a more complex movement, such as putting on a jacket.
Sensory
The sensory subtype of FND can be more complicated to diagnose. The likely findings are sensory losses that are patchy, inconsistent with dermatomes, or crossing the midline. However, these findings are not very specific for FND and can be present in other conditions.
Movement
Tremor entrainment and amplitude:
Click picture to watch video
A variable tremor amplitude is more likely to be present in FND whereas an essential tremor or Parkinson’s tremor would have a more consistent amplitude. Tremor entrainment describes distractibility in a patients tremor. When the patient is asked to perform a movement with their unaffected limb, the affected limb’s tremor will resolve or adapt.
Non-economic gait
Click picture to watch video
Click picture to watch video
Non-economic gait describes patients that use movements that take a large amount of energy or balance to compensate for their unstable gait. It is an indication of preserved muscle strength and stability.
Distractability
Click picture to watch video
FND gait disorders can also be distractible and improve when the patient shifts their attention away from their instability, whether through a task or a mobility aid. You can see in this video that the person’s gait improves drastically when using a cane.
Seizure
Functional seizures are often defined by an absence of typical seizure course and presentation. The patients who experience functional seizures often describe some degree of retained awareness during generalized episodes and typically do not have a post-ictal phase after their seizure.
Asynchronous Limb Movements:
Asynchronous limb movements are common in functional seizures however they can also be present in frontal lobe epilepsy, thus this characteristic is not specific for FND.
Retained Awareness, Absence of post-ictal phase:
Click picture to watch video
In this video, a patient advocate living with FND films her seizure episode. She discusses that she has retained awareness during the episode and we can see other features of FND–related seizures, such as closed eyes during the episode and an absence of post-ictal phase.
Eyes Closed, side to side head shaking
In this video we see a person with FND having side to side head shaking and eyes closed during their episode.
Red Flags and Comorbidities
FND is comorbid with other neurological disorders so while a patient may experience some or many features of FND on physical exam, an EM provider must assess for red flags that may point towards a concurrent structural neurological disorder.
Generally speaking, red flags include:
-
- Upper motor neuron signs on exam
- Stereotyped gait abnormalities
- Seizures that have impaired awareness and/or post-ictal phase

It can be hard to tell apart FND from temporal lobe epilepsy (TLE). Can you tell which patient is having an epileptic seizure?
Answer: The patient in the first video is having an FND seizure and the patient in the second video is having TLE.
Functional Neurologic Disorders Treatments
We have diagnosed our patient with FND based on their history and physical examination. Now what treatment options are available and how can we best facilitate them?
Most FND treatments are done in the outpatient setting and include:
Psychological counselling
CBT as a treatment for FND showed tremor improvement in 73.3% of FND patients [29], and improvement in motor functioning in 63.5% of patients. [30]
Physical rehabilitation
Current literature showed that an outpatient physiotherapy program led to both clinical and psychosocial improvements for patients with FND. [31]
Patient self-help
Patients who are informed about their condition and symptom management options tend to have improved recovery.
Patient resources:
Neurology consultation
To evaluate for concomitant neurological conditions. [31]
Treatments are not done to the patient, they are all opt-in and the patient must accept or at least consider the diagnosis for the treatments to be helpful.
Remember- you can initiate treatments for FND without being 100% confident in the diagnosis.
Prognosis and Recovery
There is a myth that FND will “go away on its own” if the patient is reassured and directed to psychotherapy.
The research on FND prognosis is sparse and estimates recovery rates between 40-60%. [2] It is estimated that 50% of patients will recover, 25% of patients will have symptom stability, and 25% will have symptom worsening.

FND Prognosis
The most well-studied prognostic factor is the duration of symptoms. Patients who start treatments after having symptoms for longer than a year are less likely to have a complete recovery.
Other poor prognostic factors that are seen in practice include:
-
- High degree of deconditioning
- Anxiety around symptoms
- Co-occurring pain syndromes
- Litigation proceedings or other things that “draw out” the recovery process
- Perceived lack of control over symptoms and recovery
Delivering the Diagnosis
A diagnosis of FND can carry significant stigma and must be delivered in a sensitive and empowering manner. At its core, your diagnosis disclosure should validate the patient’s experience and emphasize FND as a diagnosis in its own right. Dr. Sarah Lidstone is a movement disorders neurologist in Toronto who specializes in treating patients with FND.
At her appearance at the 2023 FND in Focus Meeting, she made the following recommendations [33].
-
- Give clear diagnosis
- Do not overemphasize what the patient “doesn’t have”
- Demonstrate rationale for diagnosis/discuss
- Convey potential for reversibility
- Arrange for follow up for the patient/additional outpatient supports

Summary
-
- FND is a common disorder with positive exam findings on focused neurological exam
- It is not a diagnosis of exclusion and can be concurrent with structural neurological disorders
- Assess for red flags- UMN signs, stereotyped gait, progression, post-ictal or other signs of epileptic seizure
- Stress can be a trigger but is not necessary for a diagnosis of FND
- Treatment is multidisciplinary and requires patient buy-in
- Language used for delivering diagnosis is important for all subsequent healthcare interactions
Additional Resources:
TedTalk Patient experience, TEDx- Steph Blanco:
References
References – Grand Rounds Berliant
1.FND Hope Research [Internet]. FND Hope International. Available from: https://fndhope.org/fnd-hope-research/
2.Yu JRT, Shuaib U, Mate KKV, Kaur H, Sonneborn C, Hogue O, et al. Identifying misconceptions and knowledge gaps in functional neurological disorders among emergency care providers. Journal of Clinical Neuroscience. 2023 Aug 1;114:81–8.
3.Gelauff J, Stone J. Prognosis of functional neurologic disorders. Handbook of Clinical Neurology. 2016;523–41.
4.Stefan Williams, Clea Southall, Samantha Haley, Thamer Ba Dhafari, Steven Kemp, Samuel D. Relton, Jane E. Alty, Owen Johnson, Christopher D. Graham, Melissa Maguire, To the emergency room and back again: Circular healthcare pathways for acute functional neurological disorders, Journal of the Neurological Sciences, Volume 437, 2022, 120251, ISSN 0022-510X, https://doi.org/10.1016/j.jns.2022.120251.
5.Roelofs JJ, Teodoro T, Edwards MJ. Neuroimaging in Functional Movement Disorders. Current Neurology and Neuroscience Reports. 2019;19(3):12.
6.Perez DL, Edwards MJ, Nielsen G, Kozlowska K, Hallett M, W Curt LaFrance J. Decade of progress in motor functional neurological disorder: continuing the momentum. Journal of Neurology, Neurosurgery & Psychiatry. 2021 Jun 1;92(6):668–77.
7.Mishra A, Pandey S. Functional Neurological Disorders. The Neurologist. 2022 Jul 18;27(5).
8.Finkelstein SA, Cortel‐LeBlanc MA, Cortel‐LeBlanc A, Stone J. Functional Neurological Disorder in the Emergency Department. Academic Emergency Medicine. 2021 Apr 18;28(6).
9.Lehn A, Watson E, Ryan EG, Jones M, Cheah V, Dionisio S. Psychogenic nonepileptic seizures treated as epileptic seizures in the emergency department. Epilepsia. 2021 Aug 15;62(10):2416–25.
10.Peeling JL, Muzio MR. Conversion Disorder [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551567/
11.Edwards MJ, Yogarajah M, Stone J. Why functional neurological disorder is not feigning or malingering. Nature Reviews Neurology. 2023 Feb 16;19(4):1–11.
12.the.annegirl. Instagram [Internet]. Available from: https://www.instagram.com/p/Cy3_HpjAS_p/
13.StrokeSciences. Functional Neurological Disorders & Stroke Mimics: Hoover Sign [Internet]. 2019. Available from: https://www.youtube.com/watch?v=BEtLcfikzPI&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=5
14.Pliers N. Try walking when you can’t #21 [Internet]. 2020. Available from: https://www.youtube.com/watch?v=qVWIsO8HX-c&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=5
15.Espay AJ, Aybek S, Carson A, Edwards MJ, Goldstein LH, Hallett M, et al. Current Concepts in Diagnosis and Treatment of Functional Neurological Disorders. JAMA Neurology. 2018 Sep 1;75(9):1132.
16.Anderson JR, Nakhate V, Stephen CD, Perez DL. Functional (Psychogenic) Neurological Disorders: Assessment and Acute Management in the Emergency Department. Semin Neurol. 2019;39:102–14.
17.Aybek S. Functional Limb Weakness and Paralysis. Current clinical neurology. 2022 Jan 1;53–65.
18.Sensory Deficits Image [Internet]. Available from: https://www.researchgate.net/figure/Localization-and-frequency-of-sensory-deficits-in-all-patients-at-initial-visit-either-by_fig1_42768892
19.Functional Tremor – Functional Neurological Disorder (FND) [Internet]. Functional Tremor. Available from: https://neurosymptoms.org/en/symptoms/fnd-symptoms/functional-tremor/
20.jonstone69. How am I running when I cant walk ? Recovery from FND gait disorder [Internet]. 2021. Available from: https://www.youtube.com/watch?v=Y2kwQrhxttU&t=208s
21.Downstate Neurology. David L. Perez, MD, MMSc. Motor Functional Neurological Disorders. [Internet]. 2021. Available from: https://www.youtube.com/watch?v=Fk8-T0yvI5c&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=7
22.the.annegirl. Instagram [Internet]. Available from: https://www.instagram.com/p/CngR70hKGyn/
23.Dr Sudhir Kumar MDDM Neurologist; Lifestyle Expert. Psychogenic Non-epileptic Seizures [Internet]. 2020. Available from: https://www.youtube.com/watch?v=VVjqgmH0aZo&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=7
24.the.annegirl. Instagram [Internet]. Available from: https://www.instagram.com/reel/C00VNfOM3wC/?igsh=M2J6MzVqeWIzY2ho
25.F.N.D. Functional neurological disorder-seizure [Internet]. 2018. Available from: https://www.youtube.com/watch?v=-tBC75Iw0Yw&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=2
26.Asymmetric Neuropathies [Internet]. neuromuscular.wustl.edu. 2020. Available from: https://neuromuscular.wustl.edu/nanatomy/asymmetric.html
27.Dr Sudhir Kumar MDDM Neurologist; Lifestyle Expert. Psychogenic Non-Epileptic Seizures (PNES) [Internet]. 2022. Available from: https://www.youtube.com/watch?v=MD721IH5gT4&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=3
28.clinical neurology. Frontal lobe seizures [Internet]. 2022. Available from: https://www.youtube.com/watch?v=gc-BkEyoon4&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=4
29.Espay AJ, Ries S, Maloney T, Vannest J, Neefus E, Dwivedi AK, et al. Clinical and neural responses to cognitive behavioral therapy for functional tremor. Neurology. 2019 Oct 4;93(19):e1787–98.
30.Faul L, Knight LK, Espay AJ, Depue BE, LaFaver K. Neural activity in functional movement disorders after inpatient rehabilitation. Psychiatry Research: Neuroimaging. 2020 Sep;303:111125.
31.Kola S, LaFaver K. Updates in Functional Movement Disorders: from Pathophysiology to Treatment Advances. Current Neurology and Neuroscience Reports. 2022 Apr 19;22(5):305–11.
32.Lacelle J. My Functional Neurological Disorder (FND) Recovery Story [Internet]. 2018. Available from: https://www.youtube.com/watch?v=9USepwToLqk&list=PL2nRSOCNG2XOWhhARVzcYHdMdebUNDutv&index=10&t=294s
33.Lynch P. Neurology Update Meeting 2023 – FND in focus [Internet]. Medical Independent. 2023. Available from: https://www.medicalindependent.ie/in-the-news/conference/neurology-update-meeting-2023-fnd-in-focus/





![Figure 9. Patch sensory deficits. [18]](https://emottawablog.com/wp-content/uploads/2024/04/figure10.png)






Trackbacks/Pingbacks