You deftly sweep the tongue aside, slide into the vallecula, lift the epiglottis, and have a great view of the cords. You smoothly pass the tube, secure it, and walk away – a superstar. Meanwhile your nurses wonder “what now?” as your patient begins to wake up pulls their ET tube out. Your job is not over after intubation – here we will go over how to keep your patients comfortable and safe with appropriate sedation and analgesia.
Post-intubation Analgesia:
- Being intubated is painful. So, all intubated patients should receive analgesia.
- Analgesia might be more important than sedation; in studies comparing analgesia-only to standard sedation, patients in the analgesia-only arm had better outcomes.
- Practically speaking:
- Use a pain scale validated in intubated patients (eg: Critical-Care Pain Observation Tool).
- User your preferred IV opioid.
- Boluses initially, and then start an infusion.
- Remember to give boluses for painful procedures (eg: suctioning, wound exploration, repositioning, etc).
- For agitation/restlessness: titrate analgesia first, before increasing sedation.
Post-intubation sedation: avoid benzodiazepines!
- Benzodiazepines don’t work as well as an infusion, as their half-lives increase significantly as the duration of infusion increases.
- Patients sedated with benzodiazepines had worse outcomes, including more days intubated, and more days in the ICU, when compared to patients sedated with other agents.
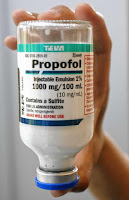
- Good alternatives include; Propofol and Etomidate.
Post-Intubation sedation: light sedation
- In the ICU, light sedation resulted in better outcomes than deep sedation, and was at least as good as daily sedation vacations.
- A recent study suggested that deep sedation within 4 hours of intubation was an independent predictor of increased mortality. Thus, our initial ED management has a larger impact than we likely perceive.
- Use a validated sedation scale; ideally patients should wake easily to verbal stimulus but remain calm.
- Important exceptions include patients with: increased ICP, status epilepticus, ongoing paralysis, or patients undergoing transportation to another facility. These populations should all likely receive deep sedation.
Take home points:
- All intubated patients should receive analgesia.
- Titrate analgesia first, then add sedation.
- Avoid benzodiazepines for post-intubation sedation.
- Target light sedation in the majority of patients.



A recent study suggested that deep sedation within 4 hours of intubation was an independent predictor of increased mortality
Great info….reference?
Sorry for the late reply. Here’s the link for that reference: Shehabi et al. Early Intensive Care Sedation Predicts Long-Term Mortality in Ventilated Critically Ill Patients. Am J Respir Crit Care Med. 2012 Oct 15;186(8):724-31