This post is a continuation of Borderline Personality Disorder – Part 1. In this second post, Dr. Beamish discusses the management of BPD in the emergency department and shares some valuable resources.
Borderline Personality Disorder – Part 2
Case 2
A 22 year old female with chronic suicidal ideation is brought to the ED by police after her roommates called with concerns about her wellbeing. A chart review reveals multiple previous visits for suicidal attempts. She has also previously been admitted to medicine and psychiatry a total of 5 times in the past 2 years.
The physical examination reveals a GCS of 15, and no signs of intoxication. She admits to a large consumption of acetaminophen. The acetaminophen level is positive (>1000 micro/L), and well above the level requiring treatment as per the reported time of ingestion.
She tells you that she does not want to live any longer and does not consent to any treatment. She understands after a lengthy discussion that a lack of treatment may result in liver failure and death. However, she is adamant and requests to leave the emergency department with no further management.

- What is capacity?
- As per the Health Care and Consent Act (1996):
- 4 (1) A person is capable with respect to a treatment, admission to or confining in a care facility or a personal assistance service if the person is able to understand the information that is relevant to making a decision about the treatment, admission, confining or personal assistance service, as the case may be, and able to appreciate the reasonably foreseeable consequences of a decision or lack of decision. 2017, c. 25, Sched. 5, s. 56.
- We are not allowed to treat someone if we believe they have the capacity to refuse treatment.
- A mental health disorder does not mean you lack capacity. There is even a case of a patient with psychosis being deemed capable to consent (Starson Swayze Supreme Court Canada 2003)
- A patient can be incapable to make some decisions and not others.
- Capacity may change over time.
- As per the Health Care and Consent Act (1996):
- Does the patient in Case 2 have capacity to consent?
- If the management of the acetaminophen overdose is started against her will (e.g. NAC for this overdose), the decision must be made that she is incapable to make decisions. This ultimately invokes this aspect of the law:
- Emergency treatment without consent: incapable person
- (2) Despite section 10, a treatment may be administered without consent to a person who is incapable with respect to the treatment, if, in the opinion of the health practitioner proposing the treatment,
- (a) there is an emergency; and
- (b) the delay required to obtain a consent or refusal on the person’s behalf will prolong the suffering that the person is apparently experiencing or will put the person at risk of sustaining serious bodily harm. 1996, c. 2, Sched. A, s. 25 (2).
- Emergency treatment without consent: incapable person
- This patient should therefore be placed on a medical hold (Form 1) for treatment of the overdose and a psychiatric assessment.
- If the management of the acetaminophen overdose is started against her will (e.g. NAC for this overdose), the decision must be made that she is incapable to make decisions. This ultimately invokes this aspect of the law:
- What does documentation outlining a patient’s incapability to consent look like?
- The below statement has not been read by a lawyer or clarified by the CMPA, but this is a blog and not a legal text. Emergency physicians are forced into imperfect decisions daily.
- Many patient interactions present issues in a medical-legal “grey zone”. At 3 AM, finding a substitute decision-maker or ethics consult is not practical.
- Here is an example:
- “I do not believe this patient currently has the capacity to refuse treatment for this overdose. I believe they are suffering from a treatable condition and have a negative emotional state that is influencing their refusal of treatment. As this is a time-sensitive medical emergency I will be commencing treatment to prevent this patient from sustaining serious bodily harm”
Management of Borderline Personality Disorder
What can we offer our patients with BPD in the emergency department? Particularly, those presenting with non-lethal overdoses, self harm behaviours or the consequences of impulsivity?
A few key points:
- Draw a line from the relationship to self-harm and suicidality.
- Inquire about relationships and how events have led to an emergency department visit.
- Validate their experience and the importance in seeking support.
- Discuss their current treatment and its effectiveness.
- Provide advice on continuing to follow up with an outpatient psychiatrist, psychologist or therapy group.
- Provide them with resources for crisis resources in the area.
- Invite them to inquire about available services at their place of work or education.
- Provide local outpatient therapy options.
Suicide risk factors
- Risk factors for suicide completion:
- Male
- Impulsivity
- Substance abuse
- Failed outpatient treatment
- Axis I psychiatric disorders
- Access to firearms
- Risk factors for suicide attempt:
- Female
- Younger
- Early in disease
- Risk factors for suicide specific to patients with BPD:
- Median age of 37 (>30 yo typically)
- Failed outpatient treatment
Suicide risk assessment
- Many physicians feel uncomfortable in completing a suicide risk assessment.
- A helpful resource:
- Suicide Assessment Five Step Evaluation and Triage Tool ” SAFE-T “which aims to assign a patient risk level. It includes the following items and then assigns a risk level based on these factors and your clinical judgment.
- Risk factors (psychiatric diagnosis, substance abuse, stressors)
- Protective factors (family, supports, religion, resilience)
- Suicide inquiry (active plan, previous attempts, intent lethal vs self injurious)
- Suicide Assessment Five Step Evaluation and Triage Tool ” SAFE-T “which aims to assign a patient risk level. It includes the following items and then assigns a risk level based on these factors and your clinical judgment.
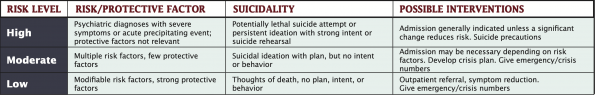
- It is important to recognize that these assessments have limitations.
- To learn more about ED interventions for suicide risk assessment refer to the Suicide Resource Prevention Centre.
Dialectical behavioural therapy (DBT)
- DBT was developed by a psychologist Dr. Marsha Linehan 9. DBT is the most well known and researched form of treatment for BPD.
- DBT begins with targeting life-threatening behaviours:
- Therapy interfering behaviours that may prevent a client from receiving effective treatment are then targeted.
- Quality of life behaviours surrounding relationships, housing, and other disorders are addressed.
- Skills acquisition allowing replacement of negative behaviour with adaptive behaviours to help patients achieve goals.
- Patients move through different stages and use a variety of techniques to help them such as:
- Mindfulness – living in the present.
- Distress tolerance – accepting yourself and the situation.
- Regulation of emotions – how to identify and adjust your emotions and intensity to the situation.
- Interpersonal effectiveness – helping people become more assertive in relationships.
- DBT has been evaluated and found to be efficacious for the treatment of BPD in multiple randomized control trials.
- It has been shown to reduce suicide attempts, emergency department visits, inpatient admissions and increases treatment retention.
- One study showed 10:
- 50% less suicide attempts
- 25% fewer ED visits
Patient resources
- Consult your psychiatric department for local or hospital-based resources.
- Local resources and community-based services can be found:
- E-Mental Health website
- The ConnexGO application
- Canadian Association for Mental Health and Addiction (CAMH)
- Ottawa specific resources:
- Mental health crisis line
- Ottawa: 613-722-6914
- Toll-free: 1-866-996-0991
If you are still searching for a more nuanced approach to borderline personality disorder in the emergency department? Dr. Victor Hong published an article with an excellent overview of BPD in the emergency department.
References
- Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533-545. doi:10.4088/JCP.v69n0404
- Goodman M, Roiff T, Oakes AH, Paris J. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79-85. doi:10.1007/s11920-011-0249-4
- Paris J. Is hospitalization useful for suicidal patients with borderline personality disorder? J Pers Disord. 2004;18(3):240-247. doi:10.1521/pedi.18.3.240.35443
- Personality Disorders. In: Diagnostic and Statistical Manual of Mental Disorders. DSM Library. American Psychiatric Association; 2013. doi:doi:10.1176/appi.books.9780890425596.dsm18
- Crowell SE, Beauchaine TP, Linehan MM. A Biosocial Developmental Model of Borderline Personality: Elaborating and Extending Linehan’s Theory. Psychol Bull. 2009;135(3):495-510. doi:10.1037/a0015616
- Hong V. Borderline personality disorder in the emergency department: Good psychiatric management. Harv Rev Psychiatry. 2016;24(5):357-366. doi:10.1097/HRP.0000000000000112
- Shaikh U, Qamar I, Jafry F, et al. Patients with borderline personality disorder in emergency departments. Front Psychiatry. 2017;8(AUG):1-12. doi:10.3389/fpsyt.2017.00136
- Fox D. Self Harm and Borderline Personality Disorder – BPD. Youtube. https://www.youtube.com/watch?v=rDOl0iZi2wA. Published 2019.
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-Behavioral Treatment of Chronically Parasuicidal Borderline Patients. Arch Gen Psychiatry. 1991;48(12):1060-1064. doi:10.1001/archpsyc.1991.01810360024003
- Linehan MM, Comtois KA, Murray AM, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757-766. doi:10.1001/archpsyc.63.7.757
- Washington U of. Dialectical Behavior Therapy. Behavioral Research and Therapy Clinics. https://depts.washington.edu/uwbrtc/about-us/dialectical-behavior-therapy/. Published 2019



