You’re starting your shift, and you’re only moderately caffeinated. You meet your resident and they tell you that their goal for the shift is to “work on flow”. You think, cool – let’s see how many patients they see today.
At least, that’s how I thought about it the first time a resident wanted to work on their flow with me. Over time, however, I am finding that the number of patients seen on a shift is not a particularly good marker for assessing a learner’s flow – is 12 abdominal pains and 2 procedures a good shift? What about 18 ‘urgent care’ patients? Should residents be seeing as many patients as their staff? Are these numbers even helpful to residents, and how is this going to make them better?
Shift Rhythm
I think the number of patients seen on shift is a surrogate marker for what we are trying to capture. A better way of truly assessing a learner’s flow (or even, your own flow, when self-reflecting) is through assessing their ‘shift rhythm‘ (not to be confused with rhythm and flow). Every shift you’ve ever worked had a tempo to it – whether it was chaotic, choppy, or easily flowing. Sometimes you have no control over the rhythm, but when you can recognize it, it can be considered as a tool to enhance productivity.
Terry Francona (Red Sox manager, responsible for the greatest comeback in baseball playoff history) used to talk about ‘setting up an inning’ to try and get the game to play out how they want it to – which you can do by anticipating your flow as segments throughout the shift.
Divide your shift in half – see that halfway mark as a reset, if you can minimize your cognitive load by dealing with reassessments, and then grabbing a snack, you’ll enhance your productivity on the later half of your shift by having a ‘clean slate’. (Don’t eat on shift? Snacks are good for you! They help to mitigate the decision making fatigue that is inherently present at the end of any shift and will help you to avoid making bad decisions, so just do it. Seriously).
In each quarter of your shift, you want to ensure that you are constantly picking up new patients to see. You won’t be able to maintain a good shift rhythm or pace without constantly picking up new patients. I’ve talked about it before, but getting stuck in ‘reassessment’ land‘ is a major hindrance to flow attempts – the key is that you always want to be seeing new patients while doing reassessments so that you never get stuck in a dead zone where you see no new patients for an extended period of time.
Situational awareness
You must also have situational awareness when it comes to the resources in your department. For example, on night shifts – I try to save procedures for around the time when a new casino shift will start, as another fresh doc in the department is more able to help push flow while I am tied up doing a procedure. Likewise – seeing a few patients, starting their workups, and then going to do a procedure is a far more productive use of time, and by the time you’re done the procedure, you’re often able to do some dispositioning.
Situational awareness is also important when it comes to the number of patients seen. If you’re working in a particular area of an Emergency Department where your flow is limited by bed-space, the number of patients available to be seen may be the biggest driver of your flow, so keep this in mind as the best time to do procedures, reassessments, etc. may be when there are no new patients to be seen in beds, and disposition decisions become a major priority.
Triaging reviewing with residents or students is also an important cornerstone of shift rhythm – whether you want them to review one or two at a time, sneaking off to see a new patient or do a reassessment while they’re writing up their chart, having learners review back to back, etc. Considering how you want to triage reviewing your learner’s cases can have a significant impact on shift rhythm, and is a variable worth considering in advance, especially if you find it to be a limitation to your flow.
Setting up your shift, and anticipating your flow apriori will make you more productive, and will help eliminate some unnecessary chaos within our shifts. Another added benefit is that as your time management skills improve – you’ll find you are able to wrap up your shift with greater efficiency (i.e.: fewer handovers, or staying late).
Feedback
When it comes to evaluating/providing feedback on a resident’s flow, I actually pay close attention to what they’re doing on shift and what they have on the go. On a piece of paper, every hour, I write down the number of patients the resident has taken in handover, has newly assessed, has active or dispositioned. I keep track of what they’re doing, when they’re doing it, and how it is impacting their efficiency. i.e.: they saw 6 patients in the first two hours, but none in the next two hours as all they did were reassessments. Having that information is far more useful to the learner as you can demonstrate tangible areas of improvement.
Here’s an example of how I document a resident’s shift rhythm:
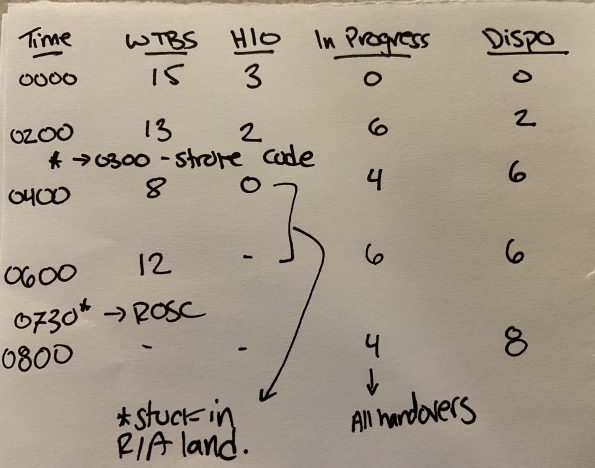
When keeping track of this kind of information, it is important to also note relevant disruptions. i.e.: were they derailed by 3 stroke codes and a major trauma? These things can influence the number of patients seen, so are relevant variables. It is also key for the learner to keep track of factors that they found to be limitations to their flow on shift, as there is a lot of potential learning from unboxing this to help find strategies to optimize whatever was disrupting their shift rhythm.
The last thing is, you need to have some semblance of knowledge regarding your own metrics. If you don’t keep track of your own shift rhythm and numbers, it is hard to know if you are performing to the standard you want to be, and if there are areas where you can make gains. The number of patients seen is a variable to consider in the overall arc of your shift rhythm, but being mindful of it will help ensure you are more productive, and better able to provide meaningful feedback to learners when you’re paying attention to it.


