Pulmonary embolism is often a nebulous diagnosis with various nuances.
-
- COMMON: They affect 25-100 people per 100,000, or approximately 30,000 Canadians every year
- Potentially FATAL: 3rd most deadly cardiovascular disease, after Heart Attack and Stroke
- Associated with LONG-TERM CONSEQUENCES: survivors are at high-risk for pulmonary hypertension
As such, prompt identification of at-risk patients is IMPORTANT.
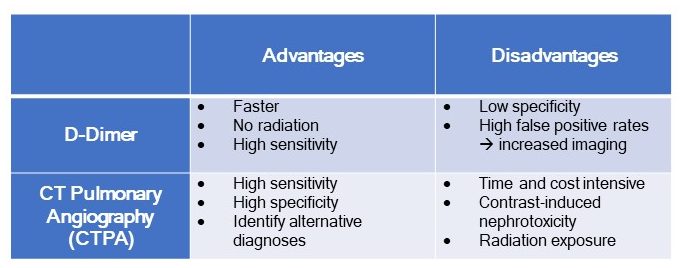
Diagnostic Testing:
Currently, two primary diagnostic tests are readily available in the emergency department to assist with the identification of Pulmonary Embolisms: D-Dimer and CT Pulmonary Angiography (CTPA). Both offer advantages and disadvantages as described below. Note that VQ Scanning is another option, but this is often less accessible within an acute care setting.
CTPA Radiation:
-
- Amounts to approximately 3x the annual baseline radiation for an average Canadian.
- Radiation effects are most prominent in young females – breast tissue is highly sensitive to carcinogenic effects of radiation.
- A fewer number of CTPA’s are required compared to other commonly ordered CT’s (i.e. Head CT) to cause a single-radiation induced cancer.
|
The challenge remains – How can we reduce unnecessary imaging for patients without missing a critical PE diagnosis? The D-Dimer offers a solution! It can be used as a risk stratification tool to identify individuals requiring imaging. |
D-Dimer: Current Evidence
Over the past few decades, there have been many developments with regards to the application and use of D-Dimer in the investigations of patients presenting with possible Pulmonary Embolism.
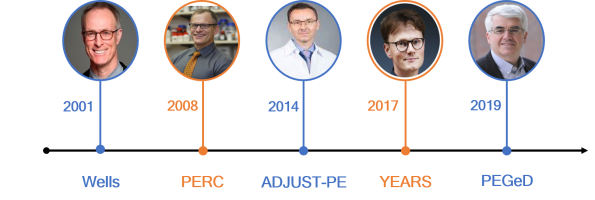
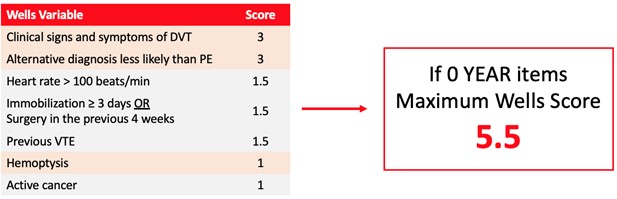
1. Wells Score (2001):
-
- Authors: Dr. Philip Wells et al.
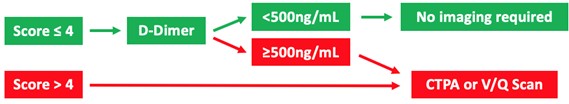
- A score of ≤ 4 using the Wells Score identifies a patient as LOW-RISK. D-Dimer becomes the next step in investigations.
- If D-Dimer ≤ 500: CTPA imaging is not required
- If D-Dimer >500 or Wells Score >4: CTPA imaging indicated
2. PERC Rule (2008):
-
- Authors: Dr. Jeffrey Kline et al.
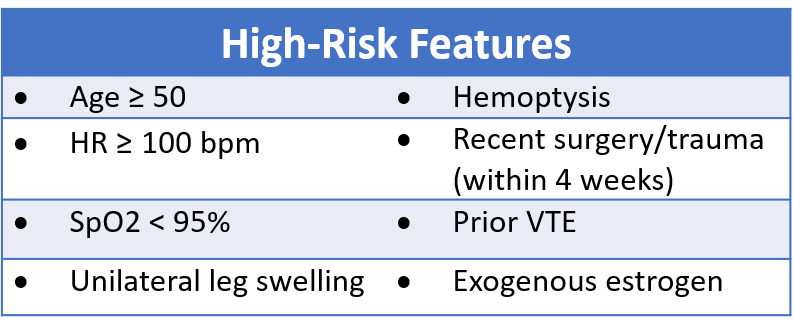
- If the patient’s pre-test probability for PE is low (<15%)
- AND the patient does not demonstrate any high-risk features
- NO INVESTIGATIONS are required
- Authors: Dr. Jeffrey Kline et al.
3. ADJUST-PE (2014):
-
- Authors: Dr. Marc Righini et al.
- The premise is that D-Dimer levels naturally rise with age. Consequently,
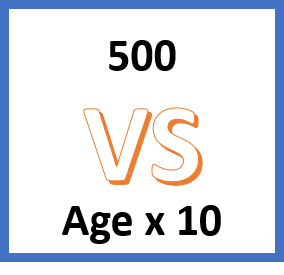 few elderly patients can have PE rule out using a D-Dimer cutoff of 500.
few elderly patients can have PE rule out using a D-Dimer cutoff of 500. - Age-Adjusted cutoff for D-Dimer set as AGE X 10
- Lead to a 12% reduction in CTPA when compared to Wells
- 0.3% miss rate
Pushing the Boundaries – Is 1,000 safe?
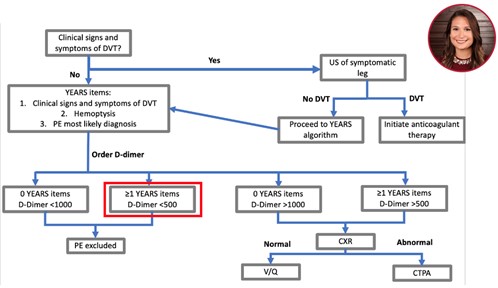
4. YEARS Algorithm Study (2017):
-
- Authors: Dr. Van der Hull et al.
- A prospective multi-centre cohort study of twelve hospitals in the Netherlands
- n=3,465 consecutive inpatients and outpatients with clinically suspected acute PE
- YEARS Algorithm: consists of three items from the Wells score that were found to be most predictive for PE (OD approx.3)
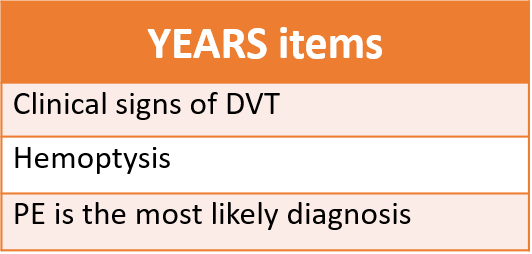
-
- Exclusion Criteria:
- Age <18
- Pregnant
- Anticoagulated (for at least 24 hours)
- Life expectancy <3 months
- Geographic inaccessibility preventing follow-up
- Research Outcomes:
- Primary: Assess the number of independent VTEs within the 3-month follow-up period for patients who were excluded from definitive imaging using the YEARS criteria
- Secondary: Number of required CTPAs compared to Wells Score
- YEARS Study Design:
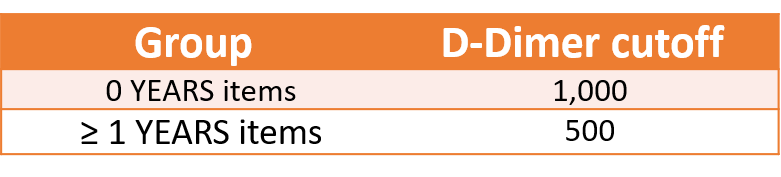
- Patients with 0 YEARS items + D-Dimer <1000 = PE excluded
- Patients with ≥ 1 YEARS items + D-Dimer <500 = PE excluded
- Exclusion Criteria:
-
- YEARS Results:
- 1,320 patients with 0 YEARS items + D-Dimer <1000 (negative D-Dimer)
- 4 VTE noted in 90 day follow-up
- 331 patients with ≥ 1 YEARS items + D-Dimer <500 (negative D-Dimer)
- 3 VTE noted in 90 day follow-up
- Miss rate of 7 out of 1,651 (0.4%) for patients in whom PE ruled-out using D-Dimer
- 14% decrease in CTPA compared to Wells
- Conclusion: D-Dimer cutoff of 1000 should be used for low-risk patients (0 YEARS items) undergoing workup for PE.
- 1,320 patients with 0 YEARS items + D-Dimer <1000 (negative D-Dimer)
- YEARS Results:
5. Pulmonary Embolism Graduated D-Dimer (PEGeD) Study (2019):
-
- Authors: Dr. C Kearon et al.
- A prospective, multi-centre cohort study from Canadian academic centres
- n = 2,017 patients with signs and symptoms of PE presenting to the ED or outpatient clinics
- Exclusion Criteria:
- Same as PEGeD study above
- Research Outcomes:
- Primary: compared PEGeD algorithm (adjusts D-Dimer threshold to clinical probability) to Wells Score
- Measured number of VTE events in 90 day follow-up period
- Secondary: Compared efficacy of PEGeD algorithm to both Age-Adjusted and YEARS algorithms
- Primary: compared PEGeD algorithm (adjusts D-Dimer threshold to clinical probability) to Wells Score
- PEGeD Study Design:
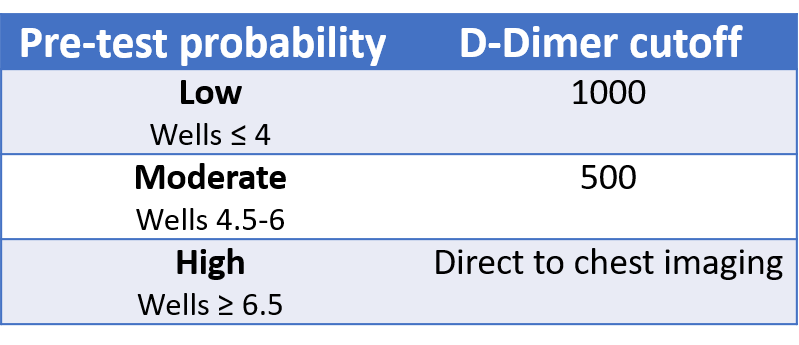
- Low Pre-Test Probability: Defined as Wells Score ≤ 4
- Evaluated use of 1,000 as D-Dimer threshold
- Moderate Pre-Test Probability: Defined as Wells Score 4.5-6
-
- Suggested use of 500 as D-Dimer threshold
-
- High Pre-Test Probability: Defined as Wells Score ≥ 6.5
- Recommend immediate CTPA
- Low Pre-Test Probability: Defined as Wells Score ≤ 4
-
- PEGeD Results:
- 1,258 patients categorized Low-Risk with PEGeD and had a negative D-Dimer
- 40 patients categorized Moderate-Risk and had a negative D-Dimer
- 0 VTE noted within 90 day follow-up
- 17.6% decrease in CTPA compared to Wells
- Conclusion: D-Dimer cut-off of 1,000 should be used for low-risk patients (Wells ≤ 4) undergoing workup for PE
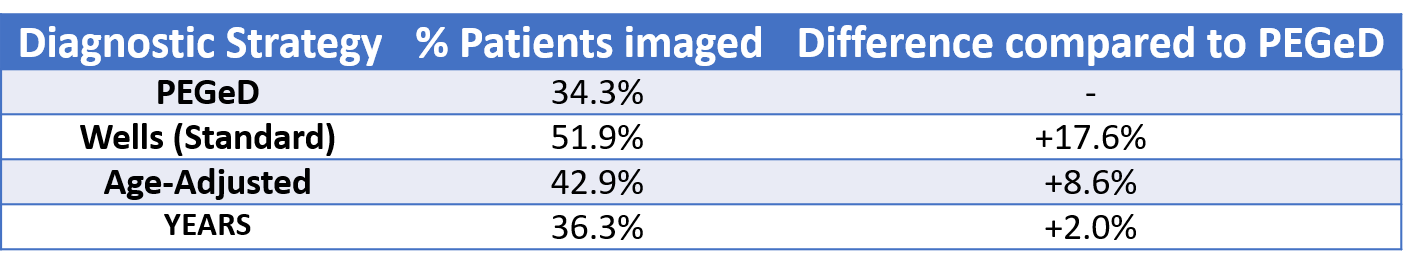
- Comparison of Imaging Rates Between Algorithms:
- Within the PEGeD study they evaluated their patient population with all the above algorithms to determine the % of patients who would undergo CTPA
- Determined highest rates of CTPA was with Wells (51.9%), and lowest with PEGeD (34.3%)
- Concluded with their study that PEGeD allows for decreased adverse effects for patients without a significant increase in missed PEs.
- Within the PEGeD study they evaluated their patient population with all the above algorithms to determine the % of patients who would undergo CTPA
- PEGeD Results:
Benefits of 1,000 as a D-Dimer Threshold:
-
- Reduces unnecessary imaging for patients, but studies have also shown benefits for EDs
- Study done in Ottawa assessed n = 972 patients over 26 months
- Found that use of 1,000 as D-Dimer threshold saved 310 hours (ED LOS) and $167,000 (CAD)
Caution Ahead: Use of D-Dimer in Moderate Risk Patients:
-
- Moderate risks patients were studied in both the PGMeD and YEARS
- PEGeD:
- Only 40% patients with moderate risk and a negative D-Dimer
- 0% of these patients had a VTE at follow-up
- **Broad confidence intervals (95% CI: 0-8.8%)
- YEARs:
- 331 patients had ≥1 YEARS items and D-Dimer < 500
- A portion of these patients with ≥1 YEARS items likely fell into the moderate Wells group (4.5-6)
- However, if they only presented with 1 YEARS item, they would be deemed low risk as per PEGeD
- Bottom Line:
- Unclear if many of these patients would have truly fallen into moderate risk PEGeD groups
- But, certainly < 331
With < 331 moderate risk patients in YEARs and 40 in PEGeD = inconclusive evidence to suggest changes in management.
Not yet validated to use a D-Dimer threshold of 500 in moderate-risk patients. Suggested that these patients continue to go directly to CTPA
Mounting Evidence:
-
- In patients with 0 YEARS items, the maximum Wells Score you can get (while also meeting all non-YEARS criteria) is 5.5
- Based on the prevalence of these characteristics, it’s very rare for patients to present with all of these features and yet not have PE as the most likely diagnosis
- Therefore, the Wells score is likely high enough that individuals are going straight to CTPA
- If missing even one of the non-YEARS items, your Wells score would automatically drop to 4 (at most 4.5)
- Therefore, closer to Low-Risk category
-
- Both YEARS and PEGeD suggest a D-Dimer cutoff of 1,000 for Low-Risk patients
- YEARS study: 1,743 patients
- Vast majority likely had Wells score ≤ 4
- Miss rate: only 0.6%
- PEGeD study: additional 1,752 patients
- Only 2 missed VTEs
- Both in patients who initially underwent CTPA (whereby imaging did not initially identify a PE)
- In total > 3,500 patients worth of data to suggest this practice change is safe
- New International guidelines from the European Society of Cardiology and European Respiratory Society published in 2019
- Advocate that D-Dimer adjusted to age or clinical probability should be considered.
Proposed Algorithm for use of D-Dimer
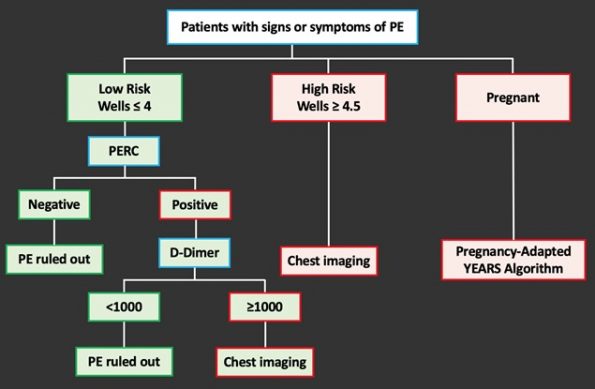
-
- First Step: Identify Wells Score for patients presenting with signs and symptoms of PE
- Second Step: Identify further investigations based on risk category
- Practice change mainly reserved for low-risk category
- Low-Risk Patients (Wells ≤ 4): Perform PERC
- PERC negative: PE ruled out
- PERC positive: order a D-Dimer
- Threshold of 1,000 or the minimum age adjusted should be used to rule out PE
- D-Dimer > 1,000 or High-Risk Patients: Direct to CTPA
- If pregnant patient, Pregnancy-Adapted YEARS algorithm recommended as presented by Dr. Renée Bradley’s in an earlier post.
Pregnancy Adapted YEARS Algorithm:
-
- We mostly agree with this approach – but recommend caution using D-Dimer to rule out a PE in a pregnant patient if Wells > 4 or ≥ 1 YEARS criteria
- Only 242 patients had ≥ 1 YEARS items of which only 31 of these patients had a D-Dimer < 500
- Most emergency physicians may be uncomfortable managing the pregnant patient this way, and may instead elect to have a discussion with Thrombosis
Expert Commentary: Is a D-Dimer appropriate
Dr. Grégoire Le Gal: Thrombosis expert and leading researcher at The Ottawa Hospital Research Institute
-
- Agrees that we should be adjusting our D-Dimer threshold
- At the minimum, he suggests using an Age-Adjusted D-Dimer threshold
- However, there is also evidence to use 1,000 as the new cutoff in low-risk patients
- Exceptions:
- Patients already on anticoagulation
- No acceptable threshold for a “negative D-Dimer” result
- Patients with prolonged symptoms (> 1 week)
- D-Dimer, like troponin, rises and falls
- Both populations excluded from the above studies
- If you have a clinical suspicion for PE go direct to CTPA
- Patients already on anticoagulation
- Dr. Le Gal agrees that the use of D-Dimer to rule out PE in moderate/high-risk pregnant patients is not yet ready for primetime due to low patient numbers
References
tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern
Med. 2009;169(22):2078-2086. doi:10.1001/archinternmed.2009.427
diagnostic imaging: Management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and D-dimer. Ann Intern Med. 2001;135(2):98-107. doi:10.7326/0003-4819-135-2-200107170-00010




Trackbacks/Pingbacks