In Part 1 of our 2-series on Elevated ICP in the ED, Dr. Hashim Kareemi described the pathophysiology of elevated ICP and compared the options for diagnosis. Click here to review Part 1. In this Part 2 post, Dr. Kareemi takes us through a phased approach to managing and treating elevated ICP for your next emergency department shift.
Guidelines for Elevated ICP
There are a variety of management guidelines available for particular etiologies of elevated ICP, which include some considerations for patients with elevated ICP.
- Trauma:
- Brain Trauma Foundation – Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition (2016)
- Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC) – A management algorithm for patients with intracranial pressure monitoring (2019)
- Intracerebral Hemorrhage:
- Subarachnoid Hemorrhage:
- AHA/ASA – Guidelines for the Management of Aneurysm Subarachnoid Hemorrhage (2012)
- Acute Ischemic Stroke:
In 2020, the Neurocritical Care Society recently published more generalized guidelines for acute treatment of cerebral edema (1), in addition to their treatment algorithm for intracranial hypertension and herniation as part of their Emergency Neurological Life Support program (2).
Unfortunately, these guidelines have limited applicability to the ED where the underlying etiology and diagnosis of elevated ICP are uncertain. Additionally, they do not provide a practical progression in care for patients in the ED and lack specific instructions.
I propose the following phased approach to treatment of patients in the ED with suspected elevated ICP. It stratifies the components of the different guidelines by the phases of care that we typically work through.
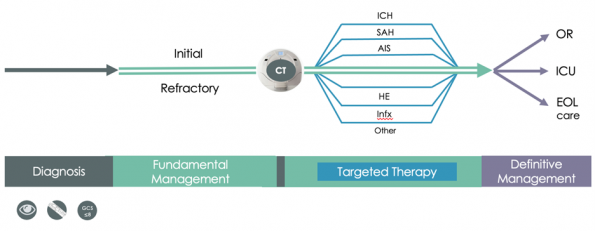
Figure 1: Phased approach to diagnosis and management of elevated intracranial pressure in the emergency department.
Maintain fundamental management (highlighted in green) instead of precipitous focus on a particular etiology (highlighted in blue), which may not yet be known. The CT scan may provide diagnostic clarity, but as we discussed it has limited diagnostic accuracy in isolation, so the onus of recognizing elevated ICP remains on the clinician using new information as the case unfolds.
The final step is “definitive management” and pertains to the ultimate disposition of the patient, whether that be an operating room, ICU, or end of life care. This must be tailored to the patient’s particular situation and informed by consulting services and the patient’s family. Much of this discussion is beyond the scope of this topic review.
The management recommendations discussed below are distilled from the previously mentioned guidelines and supplemented by expert opinion from a variety of specialties including neurocritical care, critical care, neurosurgery, and emergency medicine.
Management of Elevated ICP: Initial
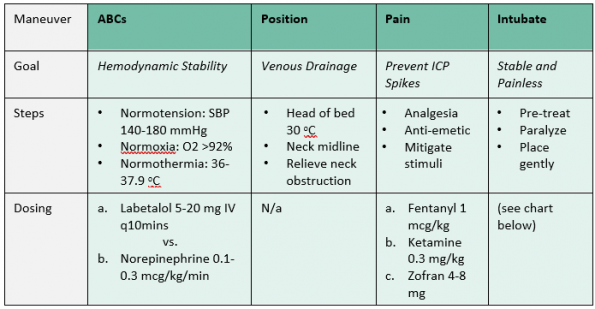
Initial management involves basic resuscitation steps with consensus across guidelines and should thus be instituted for all patients with suspected elevated ICP. It is ultimately geared towards tight hemodynamic stability and preventing spikes in ICP related to pain.
Management of Elevated ICP: Neuroprotective Intubation
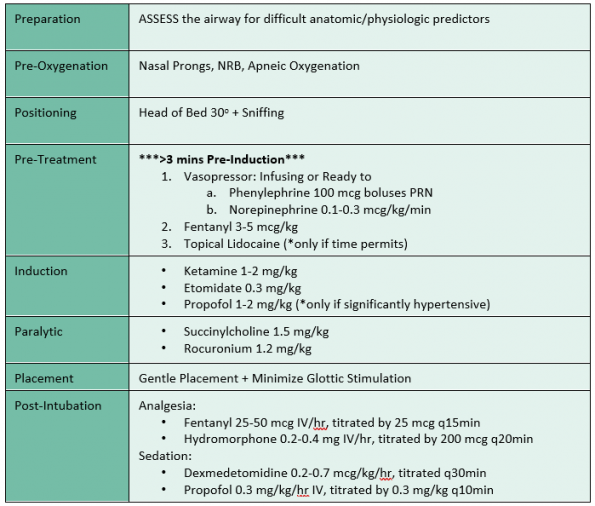
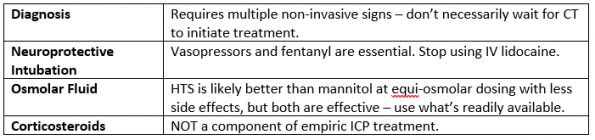
Intubation will likely be indicated for decreased level of consciousness and/or facilitation of safe transfer and imaging. As with the other initial management steps, neuroprotective intubation focuses on tight hemodynamic control while treating pain. While there is limited evidence and guidance from the management guidelines, RSI is commonly used in these scenarios and many experts agree that using these medications is safe.
Remember that despite a decreased GCS, these patients may have some degree of awareness and are likely in significant pain. A common mistake is to give smaller doses or avoid sedation altogether in patients who are unresponsive.
Some of the medications included above have been called into question for patients with elevated ICP. Based on the available evidence, let’s clarify three important points:
1. IV Lidocaine should NOT be used as a pre-treatment for neurologically injured patients
- The oft-quoted paper supporting this practice is a small trial of 20 patients undergoing elective neurosurgery for cerebral neoplasms (3).
- Since then, several studies and 2 subsequent systematic reviews of TBI patients undergoing RSI did not show any benefit of IV lidocaine for decreasing ICP elevation (4,5).
- Furthermore, lidocaine may not be a benign medication. While there isn’t good evidence to show harm with elevated ICP, a Cochrane review of pretreatment in mostly elective ORs showed a high odds ratio for adverse events such as bradycardia and hypotension (6).
- At best, IV lidocaine provides little to no benefit. At worst, it may contribute to hemodynamic instability. In either case, it serves to add complexity in an already high-risk situation.
2. Topical lidocaine may be a safe pre-treatment for neurologically injured patients, granted there is TIME for it to take effect and no additional risks (e.g. actively vomiting patient)
- There is limited evidence for topical lidocaine in this context. A trial assessing lidocaine instillation through an endotracheal tube prior to suctioning in patients with TBI showed mitigation in the increase in ICP with no adverse effects compared to no pre-treatment (7). While that is obviously a very different procedure than laryngoscopy, it may point to a potential benefit of topical lidocaine in blunting sympathetic response.
- Be aware that the time to maximal effect is 4-5 minutes (8).
3. Ketamine is a safe induction agent for neurologically injured patients, and does NOT appear to significantly increase ICP
-
- A recent systematic review only found two small studies that showed increases in ICP, in addition to two small studies that showed decreases in ICP, with no evidence of harm in patients with acute brain injury (9).
- Furthermore, a retrospective study of adult TBI patients undergoing RSI with either ketamine or etomidate showed no difference in mortality or patient outcomes between the two groups (10).
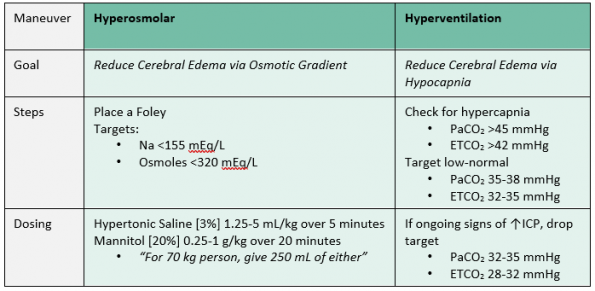
Management of Elevated ICP: Refractory
If the patient continues to show signs of elevated ICP, you should move on to these refractory management steps. Although the evidence behind these treatments is less clear, there is expert consensus amongst the guidelines that they can be beneficial, but their potential benefits must be balanced with their inherent risks.
Management: Corticosteroids
Despite being used by many physicians as an empiric treatment for elevated ICP, corticosteroids are contraindicated in many of the potential underlying conditions.
I would therefore recommend against the empirical use of corticosteroids in the undifferentiated patient with elevated ICP, and only as a targeted therapy in particular etiologies such as bacterial meningitis and CNS tumors after ruling out hemorrhagic conditions with a CT scan.
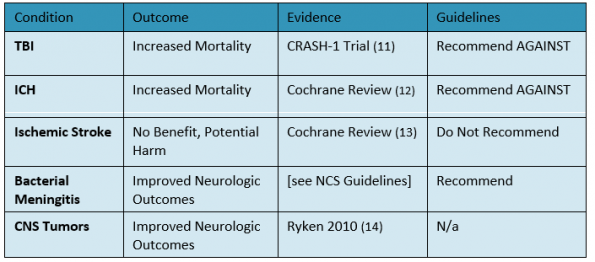
Table 4: Summary of evidence for corticosteroid use in several etiologies of elevated intracranial pressure.
Take-Home Points
References
- Cook AM, Morgan Jones G, Hawryluk GWJ, Mailloux P, McLaughlin D, Papangelou A, Samuel S, Tokumaru S, Venkatasubramanian C, Zacko C, Zimmermann LL, Hirsch K, Shutter L. Guidelines for the Acute Treatment of Cerebral Edema in Neurocritical Care Patients. Neurocrit Care. 2020 Jun;32(3):647-666. doi: 10.1007/s12028-020-00959-7. PMID: 32227294; PMCID: PMC7272487.
- Ratcliff J, Morrison C, Tran D, Ruzas C. Emergency Neurological Life Support: Intracranial Hypertension and Herniation. 2020 March.
- Bedford R, Winn H, Tyson G. Lidocaine prevents increased ICP after endotracheal intubation. In: Shulman K., Mamorou A., Miller J. (Eds.), Intracranial pressure IV (pp. 595-598). 1980. Berlin, Germany: Springer-Verlag.
- Robinson N, Clancy M. In patients with head injury undergoing rapid sequence intubation, does pretreatment with intravenous lignocaine/lidocaine lead to an improved neurological outcome? A review of the literature. Emerg Med J. 2001 Nov;18(6):453-7. doi: 10.1136/emj.18.6.453. PMID: 11696494; PMCID: PMC1725712.
- Qi DY, Wang K, Zhang H, Du BX, Xu FY, Wang L, Zou Z, Shi XY. Efficacy of intravenous lidocaine versus placebo on attenuating cardiovascular response to laryngoscopy and tracheal intubation: a systematic review of randomized controlled trials. Minerva Anestesiol. 2013 Dec;79(12):1423-35. Epub 2013 Jul 9. PMID: 23839320.
- Khan FA, Ullah H. Pharmacological agents for preventing morbidity associated with the haemodynamic response to tracheal intubation. Cochrane Database Syst Rev. 2013 Jul 3;(7):CD004087. doi: 10.1002/14651858.CD004087.pub2. PMID: 23824697.
- Bilotta F, Branca G, Lam A, Cuzzone V, Doronzio A, Rosa G. Endotracheal lidocaine in preventing endotracheal suctioning-induced changes in cerebral hemodynamics in patients with severe head trauma. Neurocrit Care. 2008;8(2):241-6. doi: 10.1007/s12028-007-9012-4. PMID: 17928962.
- Schoenemann N. K, van der Burght M, Arendt-Nielsen L, Bjerring P. Onset and duration of hypoalgesia of lidocaine spray applied to oral mucosa: a dose response study. Acta Anaesthesiologica Scandinavica. 1992;36(7):733-735. https://doi.org/10.1111/j.1399-6576.1992.tb03554.
- Gregers MCT, Mikkelsen S, Lindvig KP, Brøchner AC. Ketamine as an Anesthetic for Patients with Acute Brain Injury: A Systematic Review. Neurocrit Care. 2020 Aug;33(1):273-282. doi: 10.1007/s12028-020-00975-7. PMID: 32328972; PMCID: PMC7223585.
- Upchurch CP, Grijalva CG, Russ S, Collins SP, Semler MW, Rice TW, Liu D, Ehrenfeld JM, High K, Barrett TW, McNaughton CD, Self WH. Comparison of Etomidate and Ketamine for Induction During Rapid Sequence Intubation of Adult Trauma Patients. Ann Emerg Med. 2017 Jan;69(1):24-33.e2. doi: 10.1016/j.annemergmed.2016.08.009. PMID: 27993308; PMCID: PMC5180365.
- Roberts I, Yates D, Sandercock P, Farrell B, Wasserberg J, Lomas G, Cottingham R, Svoboda P, Brayley N, Mazairac G, Laloë V, Muñoz-Sánchez A, Arango M, Hartzenberg B, Khamis H, Yutthakasemsunt S, Komolafe E, Olldashi F, Yadav Y, Murillo-Cabezas F, Shakur H, Edwards P; CRASH trial collaborators. Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet. 2004 Oct 9-15;364(9442):1321-8. doi: 10.1016/S0140-6736(04)17188-2. PMID: 15474134.
- Feigin VL, Anderson N, Rinkel GJ, Algra A, van Gijn J, Bennett DA. Corticosteroids for aneurysmal subarachnoid haemorrhage and primary intracerebral haemorrhage. Cochrane Database Syst Rev. 2005 Jul 20;(3):CD004583. doi: 10.1002/14651858.CD004583.pub2. PMID: 16034939.
- Sandercock PA, Soane T. Corticosteroids for acute ischaemic stroke. Cochrane Database Syst Rev. 2011 Sep 7;2011(9):CD000064. doi: 10.1002/14651858.CD000064.pub2. PMID: 21901674; PMCID: PMC7032681.
- Ryken TC, McDermott M, Robinson PD, Ammirati M, Andrews DW, Asher AL, Burri SH, Cobbs CS, Gaspar LE, Kondziolka D, Linskey ME, Loeffler JS, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Kalkanis SN. The role of steroids in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010 Jan;96(1):103-14. doi: 10.1007/s11060-009-0057-4. Epub 2009 Dec 3. PMID: 19957014; PMCID: PMC2808527.