The Emergency Department is no stranger to the acutely agitated patient. Agitation remains a broad and multifactorial syndrome with a high potential for significant morbidity or mortality if not recognized and managed appropriately. This can be tricky at times when there is a lack of agreement among practitioners as what is considered first line treatment.
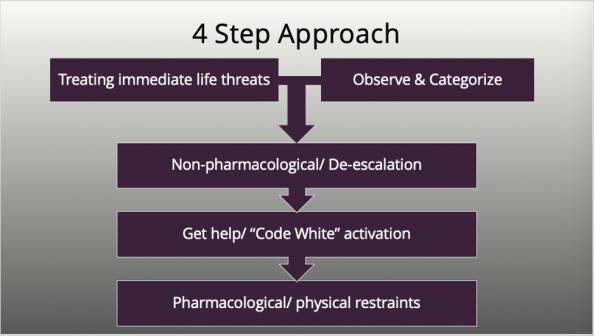
This post aims to provide a four-step approach to managing the acutely agitated patient in the Emergency Department based on expert consensus with the goal of ensuring safety of the patient, staff, and others, minimizing use of coercive interventions, and encouraging patients to regain control to manage their emotions.
First and foremost, ensure you are safe, be mindful of your environment and potential choking hazards (e.g., stethoscope, hair, pens, lanyards etc.) and have an exit strategy. Don’t hesitate to call for help if at any time you feel unsafe.
Step 1a: Differential Diagnosis/Treating life threats
Agitation is an acute issue that needs to be addressed but it’s important to ensure immediate life-threatening conditions are not overlooked. At times it can be obvious, but sometimes a bit of detective work is needed. Keep a broad differential and complete a thorough history and physical exam, review medications, obtain a set of vitals and initiate investigations.
There are many mnemonics out there that can help you be more organized in your approach (e.g., AEIOU TIPS, DIMS), use what works best for you.
Step 1b: Observe and Categorize
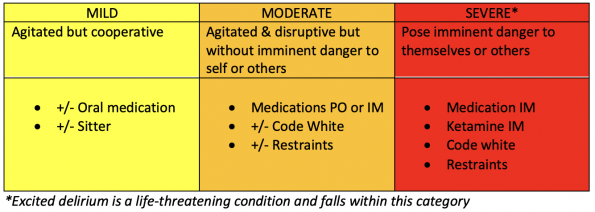
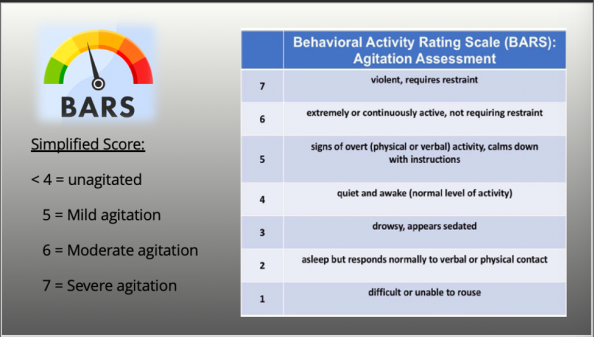
How should we categorize the degree of agitation? There are quite a few agitation scales created out there, none of which have been developed for use in the Emergency Department specifically but consensus from the American Association for Emergency Psychiatry (AAEP) identified “BARS” as a reliable and easy scale to employ, particularly in an emergency setting. For the Emergency Department, we can likely simplify the scale into 4 main categories as identified by Feng (2002):
Step 2: De-escalation
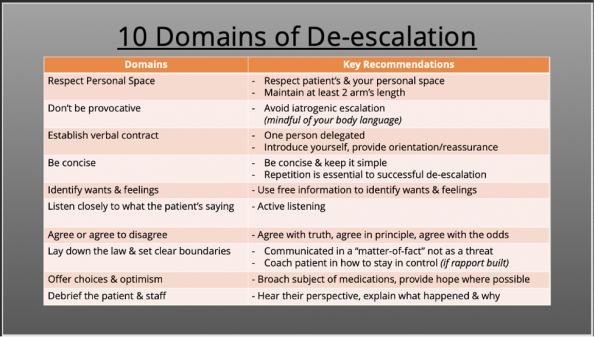
If it is safe to do so, non-pharmacological interventions should be your first line approach. The goal is to help patient’s calm themselves in order to cooperate in their care. Whether we are aware of it, we utilize de-escalation techniques daily in the emergency department. Despite its potential to decrease agitation and reduce escalation to violence there is little discussion surrounding teaching regarding verbal methods.
A consensus statement put forth by American Association of Emergency Psychiatry identified 10 domains of de-escalation that assist clinician’s in providing care of agitated patients.
Highlights from the article by Richmond et al. are summarized below:
To further simplify it, Windover et al outlines responses that may be helpful by using the mnemonic “SAVE”
- Support
- “Let’s work together…”
- Acknowledge
- “I see this has been hard for you”
- Validate
- “I’d probably be reacting the same way if I was in your shoes”
- Emotion naming
- “You seem upset”
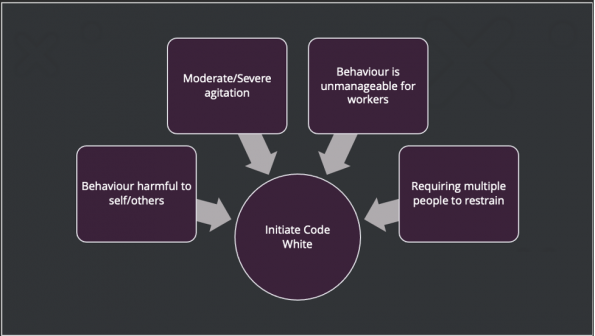
Step 3: Get Help (Code White)
There are no hard-set rules when it comes to activating a code white, but there is a general agreement in things that may prompt you to activate one.
Keep in mind that a code white should not be used as a threat for an uncooperative patient, because the code in itself can further amp up an already tense situation and can traumatically impact both patients and staff involved. If safe to do so, a great alternative would be utilization of a “concealed code white” by paging security directly rather than overhead paging for those patient’s that you feel are moderately agitated.
Step 4: Restraints
Despite best efforts to calm the situation escalation in the acutely agitation patient can be unpredictable leading to imminent danger to everyone. Restraints are considered a treatment of last resort but at times they are needed to control situations that have gotten out of hand.
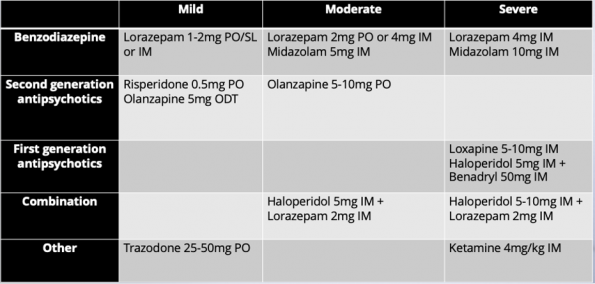
Pharmacological interventions
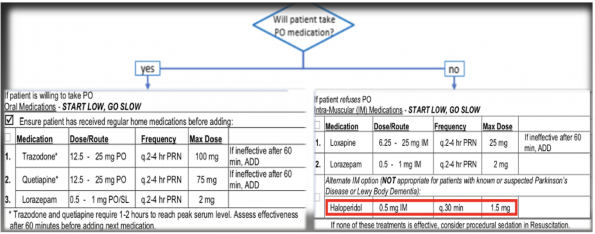
Agitation is quite the unique clinical situation as often treatment is initiated before we’ve identified the underlying cause. Despite substantial literature reviewing medications used in management of acute agitation, there is still no consensus on the ideal first line agent. Rather, current recommendations are drawn from expert consensus and can vary depending on practitioner and situation.
Things to consider when selecting your agent of choice:
- Category of agitation
- Speed of medication onset required
- Route of administration
- Special considerations
Below is a table summarizing common medications used, route of administration and for what category of agitation:
What about Ketamine for agitation? This remains up for debate and at this time it’s dependent on clinician judgement.
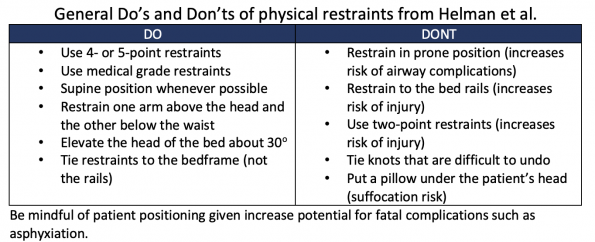
Physical restraints
Restraint use carry an elevated risk to staff and patients when implemented. Therefore, we consider this as a “treatment of last resort”. So, if initiated, keep in mind least restrictive restraint is to be used for the shortest time to reduce harm.
Special Populations
Acutely Agitated Pediatric Patient
Agitation can start with tantrums and quickly escalate to aggressive behaviour, when possible, family and caregivers may provide help, but it is important to ensure that they are not the source of the agitation. As always with any agitated patient, verbal de-escalation is first line, particularly with kids but at times chemical and physical restraints may be required.
For a review of the Approach to the acutely agitated Pediatric patient, refer to this excellent grand rounds.
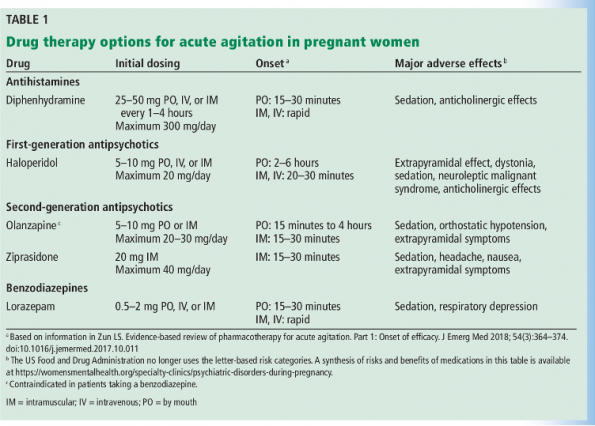
Acutely Agitated Pregnant Patient
At the best of times, we are very cautious to administer medication to pregnant patients. This adds another level of difficulty when faced with an acutely agitated pregnant patient. There’s no surprise that there is insufficient data assessing management and treatment of agitation in this population. Based on an expert consensus conducted in 2001 by Allen et al general recommendations were provided regarding therapies.
Suggested safe therapy options:
- Risperidone – Safe, no known teratogenic effects
- Haloperidol – commonly used acute, short-term setting
- Benzodiazepine – may be safe in acute setting, short-term use
- Diphenhydramine – safe, low risk of major malformations
Also, keep in mind use of physical restraints should be considered as a last resort, particularly in pregnant patients. If physical restraints are required, consider these points:
- Avoid 4-point restraints in 2nd & 3rd trimester for risk of IVC compression
- Place left lateral decubitus or right hip positioned 10-12cm off bed
- Frequent reassessments
Acutely Agitated Elderly Patient
Though agitation is not always present in delirium, with only 1/3 of cases of altered mental status presenting with agitation in the Emergency Department. We recognize that delirium is not only distressing to patients, caregivers, and health care providers but it can be a medical emergency with hospital mortality rates approaching 33%, as it can be under-recognized in the Emergency Department.
A general thought to keep in mind when encountering the older adult that’s agitated is “Old and altered, presumed delirium until proven otherwise”. Keep a broad differential diagnosis, obtain a complete history and thorough physical examination.
To assist providers in management of the agitated older adult, based on expert opinion and literature review ADEPT (Assess, diagnose, evaluate, prevent, and treat) tool was created in 2017 for use in the ED.
So, which treatment is best?
It can be tricky, treatment options can vary depending on clinician, environment, and patient factors. It’s important to consider a patient’s neurologic co-morbidities along with current medications when selecting a drug. As there is quite a variety of treatment options, here are some recommendations based on expert consensus:
- Non-delirious agitation
- Delirious agitation
- 1st line: de-escalation
- Drug choice is variable, factors to consider:
- Dementia, heart disease, respiratory failure etc.
I recognize there will be variation in practice with preferences towards different therapy choices. Below is an overview of recommended medications and route of administration.
*smaller dosing reminder with older adults
Acute agitation is an important presentation that requires early recognition and treatment.
Older adults can be complex, so, it’s important to remember to review active medications, give what they are usually given first and be cognizant of your therapy choice to avoid unwanted drug to drug interactions. Just remember the good old saying of “start low, go slow” that way you’ll know.
References
- Garriga M, Pacchiarotti I, Kasper S, Zeller SL, Allen MH, Vázquez G, Baldaçara L, San L, McAllister-Williams RH, Fountoulakis KN, Courtet P, Naber D, Chan EW, Fagiolini A, Möller HJ, Grunze H, Llorca PM, Jaffe RL, Yatham LN, Hidalgo-Mazzei D, Passamar M, Messer T, Bernardo M, Vieta E. Assessment and management of agitation in psychiatry: Expert consensus. World J Biol Psychiatry. 2016;17(2):86-128. doi: 10.3109/15622975.2015.1132007. PMID: 26912127.
- Gottlieb M, Long B, Koyfman A. Approach to the Agitated Emergency Department Patient. J Emerg Med. 2018 Apr;54(4):447-457. doi: 10.1016/j.jemermed.2017.12.049. Epub 2018 Feb 1. PMID: 29395692.
- Caplan LR. Delirium: a neurologist’s view—the neurology of agitation and overactivity. Rev Neurol Dis 2010;7:111–8.
- Naughton BJ, Moran MB, Kadah H, et al. Delirium and other cognitive impairment in older adults in the emergency department. Ann Emerg Med 1995;25:751–5.
- Stowell KR, Florence P, Harman HJ, et al. Psychiatric evaluation of the agitated patient: consensus statement of the American Asso- ciation for Emergency Psychiatry Project BETA Psychiatric Eval-uation Workgroup. West J Emerg Med 2012;13:11–6.
- Grupp-Phelan J, Harman JS, Kelleher KJ. Trends in mental health and chronic condition visits by children presenting for care at U.S. emergency departments. Public Health Rep 2007;122:55–61.
- Roppolo LP, Morris DW, Khan F, Downs R, Metzger J, Carder T, Wong AH, Wilson MP. Improving the management of acutely agitated patients in the emergency department through implementation of Project BETA (Best Practices in the Evaluation and Treatment of Agitation). J Am Coll Emerg Physicians Open. 2020 Jul 3;1(5):898-907. doi: 10.1002/emp2.12138. PMID: 33145538; PMCID: PMC7593430.
- ,ZellerSL.OverviewofProjectBETA:bestpracticesin evaluation and treatment of agitation. West J Emerg Med. 2012;13(1):1- 2.
- Richmond JS, Berlin JS, Fishkind AB, et al. Verbal De-escalation of the agitated patient: consensus statement of the American Association for Emergency Psychiatry Project BETA De-escalation workgroup. West J Emerg Med. 2012;13(1):17-25.
- Richmond JS, Berlin JS, Fishkind AB, Holloman GH Jr, Zeller SL, Wilson MP, Rifai MA, Ng AT. Verbal De-escalation of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA De-escalation Workgroup. West J Emerg Med. 2012 Feb;13(1):17-25. doi: 10.5811/westjem.2011.9.6864. PMID: 22461917; PMCID: PMC3298202.
- Richmond JS, Berlin JS, Fishkind AB, Holloman GH Jr, Zeller SL, Wilson MP, Rifai MA, Ng AT. Verbal De-escalation of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA De-escalation Workgroup. West J Emerg Med. 2012 Feb;13(1):17-25. doi: 10.5811/westjem.2011.9.6864. PMID: 22461917; PMCID: PMC3298202.
- Allen MH, Currier GW, Carpenter D, et al. The expert consensus guideline series: treatment of behavioral emergencies 2005 [quiz in J Psychiatr Pract. 2005;11(suppl 1):110–112]. J Psychiatr Pract. 2005; 11(suppl 1):5–108.
- Mavandadi V, Bieling PJ, Madsen V. Effective ingredients of verbal de-escalation: validating an English modified version of the ‘De-Escalating Aggressive Behaviour Scale’. J Psychiatr Ment Health Nurs. 2016 Aug;23(6-7):357-68. doi: 10.1111/jpm.12310. Epub 2016 Jun 8. PMID: 27271938.
- Allen MH, Currier GW, Hughes DH, et al. Expert consensus guideline series: Treatment of behavioral emergencies. Postgrad Med 2001:1-88.
- Edward Feng, V.F. (2022) Managing agitation in the ED: Part 2 – restraints, medical approach, and Discharge, CanadiEM. Available at: https://canadiem.org/managing-agitation-part-2/ (Accessed: February 5, 2023).
- Moore G, Pfaff J. Assessment and emergency management of the acutely agitated or violent adult. UpToDate. Published 2020.https://www.uptodate.com/contents/assessment-and-emergency-management-of-the-acutely-a gitated-or-violent-adult
- Long, B. (2018) EMDOCS cases: Ed approach to agitation, net – Emergency Medicine Education. Available at: http://www.emdocs.net/emdocs-cases-ed-approach-agitation/ (Accessed: February 5, 2023).
- Kanich W, Brady W, Huff S, et al. Altered mental status: Evaluation and etiology in the ED. Am J Emerg Med. 2002 Nov;20(7):613-7.
- Nordstrom K, Zun LS, Wilson MP, et al. Medical Evaluation and Triage of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA Medical Evaluation Workgroup. West J Emerg Med. 2012;13(1):3-10
- Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAMICU). Crit Care Med. 2001;29(7):1370–9
- Inouye S, Rushing J, Foreman M, et al. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998; 13: 234-242.
- Pompei P, Foreman M, Rudberg M, et al. Delirium in hospitalized older persons: outcome and predictors. J Gen Intern Med. 1998 Apr;13(4):234-42.
- Muir-Cochrane E, Oster C, Gerace A, Dawson S, Damarell R, Grimmer K. The effectiveness of chemical restraint in managing acute agitation and aggression: A systematic review of randomized controlled trials. Int J Ment Health Nurs. 2020 Apr;29(2):110-126. doi: 10.1111/inm.12654. Epub 2019 Sep 9. PMID: 31498960.
- Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study. Am J Emerg Med. 1997; 15:335–40.
- Bieniek SA, Ownby RL, Penalver A, Dominguez RA. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. Pharmacotherapy. 1998; 18:57–62.
- Wilson MP, Pepper D, Currier GW, et al. The psychopharmacology of agitation: consensus statement of the American Association for Emergency Psychiatry Project Beta Psychopharmacology Workgroup. West J Emerg Med. 2012;13:26-34.
- Klein LR, Driver BE, Miner JR, Martel ML, Hessel M, Collins JD, Horton GB, Fagerstrom E, Satpathy R, Cole JB. Intramuscular Midazolam, Olanzapine, Ziprasidone, or Haloperidol for Treating Acute Agitation in the Emergency Department. Ann Emerg Med. 2018 Oct;72(4):374-385. doi: 10.1016/j.annemergmed.2018.04.027. Epub 2018 Jun 7. PMID: 29885904.
- Nobay F, Simon BC, Levitt MA, Dresden GM. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004 Jul;11(7):744-9. doi: 10.1197/j.aem.2003.06.015. PMID: 15231461.
- Searles Quick VB, Herbst ED, Kalapatapu RK. Which Emergent Medication Should I Give Next? Repeated Use of Emergent Medications to Treat Acute Agitation. Front Psychiatry. 2021 Dec 7;12:750686. doi: 10.3389/fpsyt.2021.750686. PMID: 34950067; PMCID: PMC8688542.
- Helman, A. (2022) Emergency management of the agitated patient: Em cases, Emergency Medicine Cases. Available at: https://emergencymedicinecases.com/emergency-management-agitated-patient/ (Accessed: February 5, 2023).
- Aftab A, Shah AA. Behavioral Emergencies: Special Considerations in the Pregnant Patient. Psychiatr Clin North Am. 2017 Sep;40(3):435-448.
- Fernández-Costa D, Gómez-Salgado J, Fagundo-Rivera J, Martín-Pereira J, Prieto-Callejero B, García-Iglesias JJ. Alternatives to the Use of Mechanical Restraints in the Management of Agitation or Aggressions of Psychiatric Patients: A Scoping Review. J Clin Med. 2020 Aug 29;9(9):2791. doi: 10.3390/jcm9092791. PMID: 32872463; PMCID: PMC7565407.
- Murphy BA. Delirium. Emerg Med Clin North Am 2000;18:243-252.
- Agitation: What every emergency physician should know: 2009-08-31: … (2009) Relias Media | Online Continuing Medical Education | Relias Media – Continuing Medical Education Publishing. Available at: https://www.reliasmedia.com/articles/115677-agitation-what-every-emergency-physician-should-know (Accessed: February 5, 2023).
- Restraint acute slides – alberta health services (no date). Available at: https://www.albertahealthservices.ca/assets/info/hp/hpsp/if-hp-hpsp-prov-restraint-acute-slides.pdf (Accessed: February 6, 2023).
- Lin J, Figuerado Y, Montgomery A, Lee J, Cannis M, Norton VC, Calvo R, Sikand H. Efficacy of ketamine for initial control of acute agitation in the emergency department: A randomized study. Am J Emerg Med. 2021 Jun;44:306-311. doi: 10.1016/j.ajem.2020.04.013. Epub 2020 Apr 11. PMID: 32340820.
- Cole JB, Moore JC, Nystrom PC, Orozco BS, Stellpflug SJ, Kornas RL, Fryza BJ, Steinberg LW, O’Brien-Lambert A, Bache-Wiig P, Engebretsen KM, Ho JD. A prospective study of ketamine versus haloperidol for severe prehospital agitation. Clin Toxicol (Phila). 2016 Aug;54(7):556-62. doi: 10.1080/15563650.2016.1177652. Epub 2016 Apr 22. PMID: 27102743.
- Aftab A, Shah AA. Behavioral Emergencies: Special Considerations in the Pregnant Patient. Psychiatr Clin North Am. 2017 Sep;40(3):435-448. doi: 10.1016/j.psc.2017.05.017. PMID: 28800800.
- Wilson MP, Nordstrom K, Shah AA, Vilke GM. Psychiatric emergencies in pregnant women. Emerg Med Clin North Am. 2015; 33(4):841–851. doi:10.1016/j.emc.2015.07.010
- Niforatos J, et al. How should I treat acute agitation in pregnancy? Cleveland Clinic Journal of Medicine. 2019; 86(4):243-247
- Ladavac AS, Dubin WR, Ning A, Stuckeman PA. 2007. Emergency management of agitation in pregnancy. Gen Hosp Psychiatr. 29:39–41.
- Shenvi C, Kennedy M, Austin CA, Wilson MP, Gerardi M, Schneider S. Managing Delirium and Agitation in the Older Emergency Department Patient: The ADEPT Tool. Ann Emerg Med. 2020 Feb;75(2):136-145. doi: 10.1016/j.annemergmed.2019.07.023. Epub 2019 Sep 26. PMID: 31563402; PMCID: PMC7945005.
- Erstad BL, Patanwala AE. Ketamine for analgosedation in critically ill patients. J Crit Care. 2016 Oct;35:145-9. doi: 10.1016/j.jcrc.2016.05.016. Epub 2016 May 25. PMID: 27481750.
- Carr FM. The role of sitters in delirium: an update. Can Geriatr J. 2013;16(1):22-36. doi: 10.5770/cgj.16.29. Epub 2013 Mar 4. PMID: 23440038; PMCID: PMC3578770.
- Tzeng HM, Yin CY, Grunawalt J. Effective assessment of use of sitters by nurses in inpatient care settings. J Adv Nurs. 2008 Oct;64(2):176-83. doi: 10.1111/j.1365-2648.2008.04779.x. PMID: 18990098.
- Battaglia J, Moss S, Rush J, Kang J, Mendoza R, Leedom L, Dubin W, McGlynn C, Goodman L. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study. Am J Emerg Med. 1997 Jul;15(4):335-40. doi: 10.1016/s0735-6757(97)90119-4. PMID: 9217519.
- Windover AK, Boissy A, Rice TW, et al. The REDE model of healthcare communication: optimizing relationship as a therapeutic agent. J Patient Exp. 2014;1(1):8-13.




this was a great presentation regarding dealing with behavioral situations