In Part 1 of this 2 part series, we focused on animal bite management. In Part 2, we will look at our approach to human bites and considerations around addressing Rabies related concerns.
Human Bites
- Human bites can present as:
- Occlusive bites: Bites from human teeth often occurring on the hands or arms.
- Fight bites/clenched fist injuries: Typically have traumatic lacerations over the MCPs
- Specifically with fight bites, these are considered high risk injuries because of the polymicrobial nature of the human mouth and higher risk for complications and infections
- These typically have a delayed presentation given the nature of the injury and present more frequently with infection on first presentation.
- Fight bites specifically have an infection rate of 10-50% with the risk of developing into severe hand infections, including septic arthritis and osteomyelitis
Microbiology
Similar to animal bites, antibiotic coverage should cover both the common skin flora and oral anaerobes, with eikenella being a common isolate. First line medications for treatment and prophylaxis would be the same as animal bites, with oral amox clav being first line.
But why are fight bites so high risk?
- The anatomy of the hand provides a complicated network of potential spaces and deeper structures that pose the risk of infection. The human bite has the potential of entering these spaces and inoculating structures with bacteria.
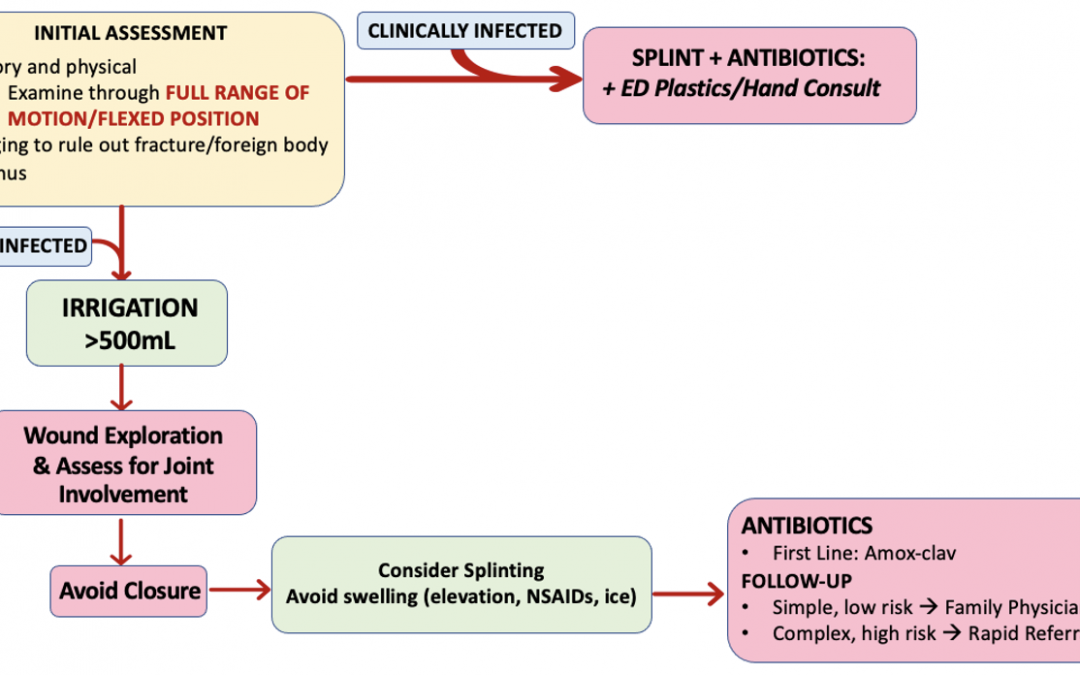
- For fight bites, it is prudent that we assess the hand for not only the extent of soft tissue damage, but we must assess for tendon laceration, joint involvement and ruling out fractures with a simple x-ray.
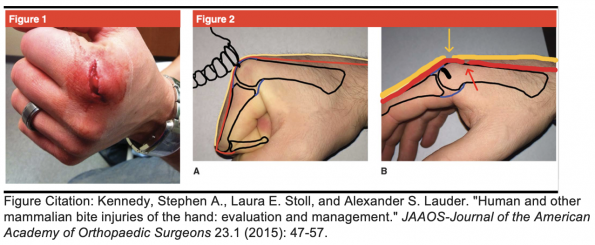
- This modified figure illustrates how fight bites can appear like a simple skin laceration, but are actually the hiding spot for deeper injuries affecting the skin (yellow), tendons (red) and joint (black).
- If you were to examine these wounds in an extended position you would miss the deeper injuries.
- It is imperative that we examine these injuries in the position that the injury occurred and through full range of motion.
Take Home Point #4: Respect the fight bite – these injuries are high risk of severe infection and morbidity. Make sure to examine the injury in a flexed position to ensure you don’t miss deeper injuries.
Lets talk to the Experts
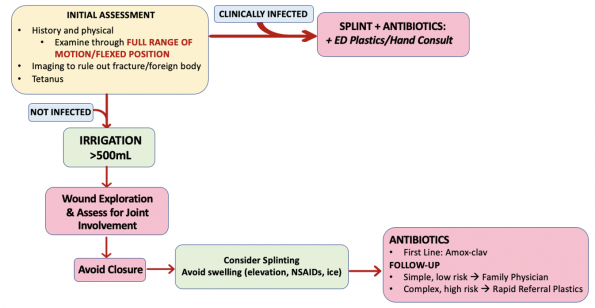
Dr. Brent Trull and Dr. Kevin Cheung provided me wither further insight into their management of human bite wounds, as summarized below.
- Keep a high suspicion for joint involvement!
- The most common error they see is when the fight bite is examined with fingers extended which pulls the extensors overtop of the joint, making it difficult to identify the intra-articular communication.
- After good local, examining the finger through full range and full finger flexion will often identify an injury through the extensor.
- The mainstay of treatment in the ED is thorough exploration and wound washout followed by antibiotic prophylaxis.
- Patients may not be forthcoming with how they got this type of injury, so keep a high suspicion when you see these classic presentations.
- Both Dr. Trull and Dr. Cheung recommended getting x-rays for these injuries to ensure there is no fracture or foreign body like a broken tooth.
- Follow up:
- Family physician: Uninfected fight bites, after irrigation and antibiotic prescription
- Hand surgeon/Plastic Surgery: If there is concern for tendon laceration or involvement of deeper structures
- ED Consult: If they present infected, they should be seen by the on-call team in the ED.
Rabies
Human rabies is very rare in Canada, with only 26 human rabies deaths recorded in Canada since reporting began in 1924. With the most recent death in 2019 in BC after an exposure to a bat and in 2012 in Ontario with an exposure outside of Canada. However, if we look at rabies prevalence worldwide, it remains a major public health problem.
Worldwide, the WHO reports 59,000 deaths per year from rabies. That’s 1 death every 9 minutes, with 40% of rabies deaths are in children under the age of 15. Rabies also disproportionately affects developing and more rural areas of the world with limited access to health care. Major effected areas include Africa and parts of Asia, with the major culprits in these regions being dogs, with 99% of human cases due to dog bites.
When looking at cases of rabies transmission, dogs remain the #1 cause of rabies transmission in humans. In Canada, bats are the most common reservoir for rabies, followed by skunks, raccoons and foxes.
Rabies Virus
- Type of virus: Bullet shaped lyssavirus from the rhabdoviridae family with single stranded RNA genome
- The rabies virus is neurotropic, meaning it has a predilection for neuro tissue.
- As a result, bites that occur in areas that have higher density of nerve endings are at increased risk of developing rabies and bites closer to the CNS have shorter incubation times.
- Rabies is known to have one of the highest case fatality rates of any human infectious diseases, with a near 100% fatality rate once the clinical phase has started.
Rabies Life Cycle
- Transmission:
- Most commonly occurs through direct contact with saliva (ex. bites) or from contact with nervous system tissue from an infected animal.
- Other routes of transmission are uncommon, but can occur from inhalation or organ transplants.
- Incubation Period
- Starts after the bite occurs.
- Infected individual will generally be ASYMPTOMATIC during this period.
- Duration: Most commonly 1-3 months
- Can vary in length depending on the location of the virus and how far it is from the brain as the virus travels upward.
- During this period, the virus first replicates in the peripheral tissue and then entered the local motor and sensory nerves. It then slowly migrates retrogradely along the peripheral nerves to the spinal cord and CNS. Once in the CNS, the virus will then move centrifugally along somatic and autonomic nerves resulting in widespread dissemination.
- Rapid viral replication and shedding occurs in highly innervated areas, such as the salivary gland, which is why bites are the most common method or transmission.
- Prodromal Period
- Period where the first symptoms will start to occur.
- Symptoms will be similar to the flu with complaints of generalized weakness, fever, headache.
- Some may complain of local discomfort or parasthesias at the site of the bites.
- Duration: Few days to a week
- Classic rabies symptoms
- Encephalitic Group (“Furious Rabies”) – 80% cases
- Symptoms will include “classic” rabies symptoms including hydrophobia, aerophobia and agitation.
- Paralytic Group – <20% cases
- Will develop a progressive flaccid paralysis.
- Once patients develop these clinical signs of rabies, the disease is almost fatal and treatment is generally supportive.
- Duration: Can vary in duration, but typically death will occur in 7-14 days.
Rabies Prevention
- Luckily with today’s advancements rabies is almost completely preventable with prompt post-exposure prophylaxis (PEP).
- There have been few cases of reported PEP failure worldwide, however almost always occurring after a deviation from the recommended PEP schedule. There have been no true PEP failures that have been reported in Canada or the US.
- Rabies prevention can be broken down into two major categories:
- Pre-exposure prophylaxis = 3 dose rabies vaccine series
- Given to high risk patients BEFORE an exposure occurs
- Examples of high risk patients:
- People who routinely work with high risk animals
- Lab workers who handle the virus
- Travelers going to endemic areas who may not have access to rabies treatment
- Post-exposure prophylaxis
- Passive Immunity = Rabies Immune Globulin
- Active Immunity = Rabies Vaccine
- Pre-exposure prophylaxis = 3 dose rabies vaccine series
Rabies Treatment: PEP
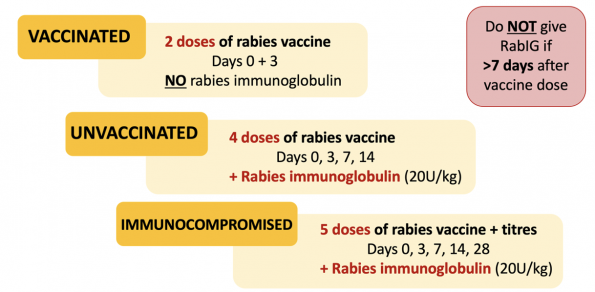
The recommended PEP regimens for rabies varies based on two factors:
- Is the patient previously immunized for rabies (i.e. received pre-exposure prophylaxis)?
- Is the patient immunocompromised?
See figure below for outlined post-exposure prophylaxis for these groups.
Reminder: The vaccine will start producing neutralizing antibodies in 7 days. So if a patient presented to the ED after getting a vaccine elsewhere, we would NOT give the rabies immunoglobulin after 7 days as there is no role for passive immunity at this time.
For the rabies immune globulin, the dose is 20U/kg and should be given at the site of the bite after thorough irrigation and wound care.
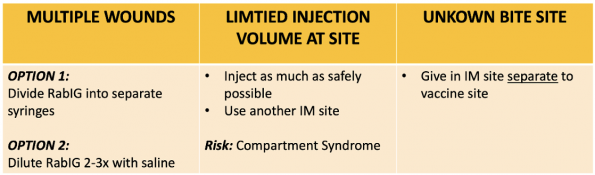
Below is a quick summary of an approach to different scenarios you may run into when trying to administer Rabies Immune Globulin.
Wound Care
Similar to the management of animal bites, wound care plays a key role in rabies prevention as well and should not be overlooked.
A few tips to remember when treating wounds that are high risk for rabies:
- Use copious irrigation and consider using a 1% diluted iodine solution as it is thought to be virucidal. Given that these bites are particularly high risk, avoid closure if possible.
- If you do need to close a wound that you are concerned for rabies exposure, after thorough wound irrigation, administer the rabies immunoglobulin BEFORE closure and even consider delaying wound closure for a few hours after the rabies immunoglobulin is instilled.
Who do we give Rabies PEP to?
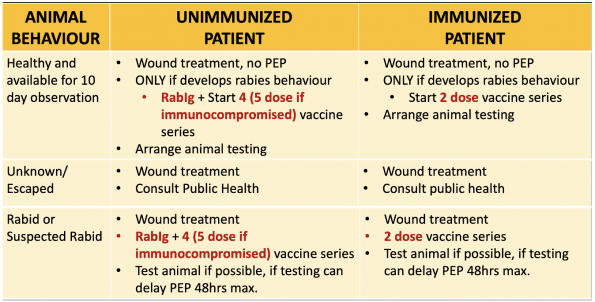
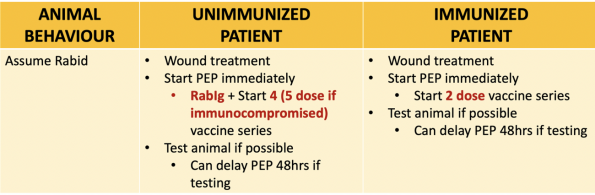
See below for summaries regarding the type of animal and considerations for PEP (adapted from Ontario Ministry of Health Management of Potential Rabies Exposure Guideline, 2020).
Domestic Animals (Dogs, Cats, Ferrets)
Wild Animals (Skunk, Bat, Fox, Racoon, Coyote)
- Of note, bites from squirrels, chipmunks, rats, mice and small rodents are generally fairly low risk for rabies and PEP is only given if the behaviour of the animal is highly unusual. However, in these situations, the recommendation is to consult public health for formal opinion.
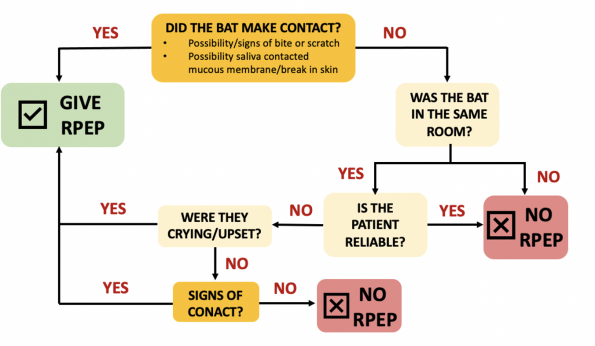
Bats
- Bats pose a unique clinical dilemma regarding rabies PEP given that the exposures may not be as obvious.
- When approaching a bat exposure, two key questions you should ask yourself are:
- Did skin or mucous membranes come into contact with the bat?
- Is the patient reliable and able to provide a clear history regarding the exposure?
- For example, is the patient a child or cognitively impaired and cannot provide a reliable history?
Key Change:
- As noted in the above diagram, public health no longer recommends giving PEP to patients who are found asleep in the same room as the bat with no evidence of direct exposure.
- This change was made in 2009 by the National Advisory Committee on Immunization based on evidence that the risk of rabies transmission in these cases is extremely low (De Serres et al.)
Reporting Requirements:
- Remember to report ALL animal bites to Public Health
- In Ottawa, Ottawa Public Health is available 24/7
- During regular business hours (Mon-Fri, 8:30-4:30), call 613-380-6744
- Select language, press 5 for Public Health Inspector (PHI) and 2 for animal bite
- After hours or on weekends/holidays: Call 311 and ask for the PHI
- During regular business hours (Mon-Fri, 8:30-4:30), call 613-380-6744
- In Ottawa, Ottawa Public Health is available 24/7
References
- Aziz, Hassan, et al. “The current concepts in management of animal (dog, cat, snake, scorpion) and human bite wounds.” Journal of Trauma and Acute Care Surgery 78.3 (2015): 641-648.
- Ball, Vincent, and Bradley N. Younggren. “Emergency management of difficult wounds: Part I.” Emergency medicine clinics of North America 25.1 (2007): 101-121.
- Banyard, A. C., and N. Tordo. “Rabies pathogenesis and immunology.” Revue Scientifique et Technique (International Office of Epizootics) 37.2 (2018): 323-330.
- Baxter, Megan, Kerina J. Denny, and Gerben Keijzers. “Antibiotic prescribing in patients who presented to the emergency department with dog bites: a descriptive review of current practice.” Emergency Medicine Australasia 32.4 (2020): 578-585.
- Bhaumik, Soumyadeep, Richard Kirubakaran, and Sirshendu Chaudhuri. “ Primary closure versus delayed or no closure for traumatic wounds due to mammalian bite.” Cochrane Database of Systematic Reviews 12 (2019).
- Chen, Esther, et al. “Primary closure of mammalian bites.” Academic Emergency Medicine 7.2 (2000): 157-161.
- Cheng, Hsu-Tang, Yung-Chang Hsu, and Chao-I. Wu. “Does primary closure for dog bite wounds increase the incidence of wound infection? A meta-analysis of randomized controlled trials.” Journal of Plastic, Reconstructive & Aesthetic Surgery 67.10 (2014): 1448-1450.
- Davis, Benjamin M., Glenn F. Rall, and Matthias J. Schnell. “Everything you always wanted to know about rabies virus (but were afraid to ask).” Annual review of virology 2 (2015): 451-471.
- Dean, D. J., G. M. Baer, and W. R. Thompson. “Studies on the local treatment of rabies-infected wounds.” Bulletin of the World Health Organization 28.4 (1963): 477.
- De Serres, Gaston, et al. “Bats in the bedroom, bats in the belfry: reanalysis of the rationale for rabies postexposure prophylaxis.” Clinical Infectious Diseases 48.11 (2009): 1493-1499.
- Dimcic, Tjasa, Minja Gregoric, and Vesna Breznik. “Rapidly Progressive Infection of Hand After a Cat Bite.” Cureus 12.7 (2020).
- Dire, Daniel J. “Cat bite wounds: risk factors for infection.” Annals of emergency medicine 20.9 (1991): 973-979.
- Elenbaas, Robert M., W. Kendall McNabney, and William A. Robinson. “Evaluation of prophylactic oxacillin in cat bite wounds.” Annals of emergency medicine 13.3 (1984): 155-157.
- Fernandez, Ritin, et al. “Water for wound cleansing.” Cochrane database of systematic reviews 9 (2002).
- Fooks, Anthony R., et al. “Rabies (Primer).” Nature Reviews: Disease Primers 3.1 (2017).
- Griego, Robert D., et al. “Dog, cat, and human bites: a review.” Journal of the American Academy of Dermatology 33.6 (1995): 1019-1029.
- Hampson, Katie, et al. “Estimating the global burden of endemic canine rabies.” PLoS neglected tropical diseases 9.4 (2015): e0003709.
- Henry, Francis P., Elizabeth M. Purcell, and Patricia A. Eadie. “The human bite injury: a clinical audit and discussion regarding the management of this alcohol fuelled phenomenon.” Emergency Medicine Journal 24.7 (2007): 455-458.
- Hemachudha, Thiravat, et al. “Human rabies: neuropathogenesis, diagnosis, and management.” The Lancet Neurology 12.5 (2013): 498-513.
- Henton, J., and A. Jain. “Cochrane corner: antibiotic prophylaxis for mammalian bites (intervention review).” Journal of Hand Surgery (European Volume) 37.8 (2012): 804-806.
- Iqbal, Tanzeem. “Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 1. Antibiotics in cat bites.” Emergency medicine journal: EMJ 25.10 (2008): 686-687.
- Jaindl, Manuela, et al. “The management of bite wounds in children—a retrospective analysis at a level I trauma centre.” Injury 43.12 (2012): 2117-2121.
- Kaplan, M. M., et al. “Studies on the local treatment of wounds for the prevention of rabies.” Bulletin of the World Health Organization 26.6 (1962): 765.
- Keates, Liisamaria. “Rabies vaccines: WHO position paper—recommendations.” Vaccine (2010).
- Kennedy, Stephen A., Laura E. Stoll, and Alexander S. Lauder. “Human and other mammalian bite injuries of the hand: evaluation and management.” JAAOS-Journal of the American Academy of Orthopaedic Surgeons 23.1 (2015): 47-57.
- Khan, Muhammad N., and Abul H. Naqvi. “Antiseptics, iodine, povidone iodine and traumatic wound cleansing.” Journal of tissue viability 16.4 (2006): 6-10.
- Maimaris, C., and D. N. Quinton. “Dog-bite lacerations: a controlled trial of primary wound closure.” Emergency Medicine Journal 5.3 (1988): 156-161.
- Medeiros, Iara Marques, and Humberto Saconato. “Antibiotic prophylaxis for mammalian bites.” Cochrane Database of Systematic Reviews 2 (2001).
- Mitnovetski, Sergei, and Frank Kimble. “Cat bites of the hand.” ANZ journal of surgery 74.10 (2004): 859-862.
- Morgan, Marina, and John Palmer. “Dog bites.” Bmj 334.7590 (2007): 413-417.
- National Advisory Committee on Immunization. “Recommendations regarding the management of bat exposures to prevent human rabies.” Canada Communicable Disease Report 35.ACS-7 (2009): 1-28.
- National Institute for Health and Care Excellence. “Human and animal bites: antimicrobial prescribing guideline evidence review.” NICE. (2020): 1-55.
- National Institute for Health and Care Excellence. “Human and animal bites: antimicrobial prescribing guideline.” NICE. (2020): 1-27.
- Ong, Yee Siang, and L. Scott Levin. “Hand infections.” Plastic and Reconstructive Surgery 124.4 (2009): 225e-233e.
- Oehler, Richard L., et al. “Bite-related and septic syndromes caused by cats and dogs.” The Lancet infectious diseases 9.7 (2009): 439-447.
- Ontario Agency for Health Protection and Promotion (Public Health Ontario). Management of patients with suspected rabies exposure: guidance for health care providers working with your local public health unit. Toronto, ON: Queen’s Printer for Ontario; 2017.
- Ontario Ministry of Health. Management of potential rabies exposures guideline, 2020.
- Paschos, Nikolaos K., et al. “Primary closure versus non-closure of dog bite wounds. A randomised controlled trial.” Injury 45.1 (2014): 237-240.
- Pearce, John MS. “Louis Pasteur and rabies: a brief note.” Journal of Neurology, Neurosurgery & Psychiatry 73.1 (2002): 82-82.
- Perron, Andrew D., Mark D. Miller, and William J. Brady. “Orthopedic pitfalls in the ED: fight bite.” The American journal of emergency medicine 20.2 (2002): 114-117.
- Pfortmueller, Carmen A., et al. “Dog bite injuries: primary and secondary emergency department presentations—a retrospective cohort study.” The Scientific World Journal 2013 (2013).
- Quinn, James V., et al. “Randomized controlled trial of prophylactic antibiotics for dog bites with refined cost model.” Western journal of emergency medicine 11.5 (2010): 435.
- Rothe, Karin, Michael Tsokos, and Werner Handrick. “Animal and human bite wounds.” Deutsches Ärzteblatt International 112.25 (2015): 433.
- Rui-feng, Chen, et al. “Emergency treatment on facial laceration of dog bite wounds with immediate primary closure: a prospective randomized trial study.” BMC emergency medicine. Vol. 13. BioMed Central, 2013.
- Rupprecht, Charles E., et al. “Evidence for a 4-dose vaccine schedule for human rabies post-exposure prophylaxis in previously non-vaccinated individuals.” Vaccine 27.51 (2009): 7141-7148.
- Sartelli, Massimo, et al. “2018 WSES/SIS-E consensus conference: recommendations for the management of skin and soft-tissue infections.” World Journal of Emergency Surgery 13.1 (2018): 1-24.
- Schär, Lukas, et al. “Bite injuries to the hand and forearm: analysis of hospital stay, treatment and costs.” Journal of hand surgery (European volume) 48.1 (2023): 41-45.
- Seegmueller, Jessica, et al. “Cat and dog bite injuries of the hand: early versus late treatment.” Archives of orthopaedic and trauma surgery 140 (2020): 981-985.
- Shewring, D. J., et al. “The management of clenched fist ‘fight bite’injuries of the hand.” Journal of hand surgery (European volume) 40.8 (2015): 819-824.
- Singer, Adam J., and Alexander B. Dagum. “Current management of acute cutaneous wounds.” New England Journal of Medicine 359.10 (2008): 1037-1046.
- Singer, Adam J., Judd E. Hollander, and James V. Quinn. “Evaluation and management of traumatic lacerations.” New England Journal of Medicine 337.16 (1997): 1142-1148.
- Smith, P. F., A. M. Meadowcroft, and D. B. May. “Treating mammalian bite wounds.” Journal of clinical pharmacy and therapeutics 25.2 (2000): 85-99.
- Stevens, Dennis L., et al. “Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America.” Clinical infectious diseases 59.2 (2014): e10-e52.
- Suwansrinon, Kanitta, et al. “Is injecting a finger with rabies immunoglobulin dangerous?.” The American journal of tropical medicine and hygiene 75.2 (2006): 363-364.
- Talan, David A., et al. “Bacteriologic analysis of infected dog and cat bites.” New England Journal of Medicine 340.2 (1999): 85-92.
- Tabaka, Meg E., et al. “Predictors of infection from dog bite wounds: which patients may benefit from prophylactic antibiotics?.” Emergency Medicine Journal 32.11 (2015): 860-863.
- Talan, David A., et al. “Clinical presentation and bacteriologic analysis of infected human bites in patients presenting to emergency departments.” Clinical infectious diseases 37.11 (2003): 1481-1489.
- Tarantola, Arnaud. “Four thousand years of concepts relating to rabies in animals and humans, its prevention and its cure.” Tropical medicine and infectious disease 2.2 (2017): 5.
- Vermeulen, H., S. J. Westerbos, and D. T. Ubbink. “Benefit and harm of iodine in wound care: a systematic review.” Journal of Hospital Infection 76.3 (2010): 191-199.
- Warshawsky, Bryna, and Shalini Desai. “Exposure to bats: updated recommendations.” CMAJ 182.1 (2010): 60-60.
- World Health Organization. “Rabies vaccines: WHO position paper, April 2018–Recommendations.” Vaccine 36.37 (2018): 5500-5503.
- World Health Organization. WHO expert consultation on rabies: third report. Vol. 1012. World Health Organization, 2018.
- World Health Organization. “Zero by 30: The global strategic plan to end human deaths from dog-mediated rabies by 2030.” (2018).


Trackbacks/Pingbacks