Case
You and your partner arrive at a scene where a 67-year-old male had a witnessed collapse 5 minutes ago and CPR is in progress; he is in cardiac arrest. The initial rhythm is ventricular fibrillation. You continue CPR with a King LT and provide 3 shocks, along with a dose of epinephrine remembering that early epinephrine can improve outcome, but he remains in VF. You start planning for transportation to the hospital, but you remember something in the ALS PCS about 20 minutes of on-scene resuscitation. You wonder what the best course of action is. Should you stay on scene or initiate transport? Is there anything else you can do for this patient to optimize their chance of survival?
Analyzing the Data
In 2020, paramedics of the RPPEO performed resuscitation on 1228 medical cardiac arrests. Approximately 55% of treated arrests were witnessed, and 48% received bystander CPR. In 22.5% of these arrests the initial rhythm was VF or VT, with the remainder being PE or asystole. Paramedics provided the first application of a defibrillator 78% of the time, with fire, police and bystanders providing the first defib application for the others. An ACP was on scene 72% of the time. About half of all cardiac arrest patients had resuscitation terminated in the field. In terms of outcomes, overall, 8.0% of patients survived to hospital discharge compared to 6.2% nationally. For patients with initial rhythm of VF/VT, the survival rate was 21.6%, compared to 20.9% nationally. The vast majority of survivors had ROSC obtained in the field. Survival for patients transported without ROSC was 0.9%.
How can this data help us make decisions about cardiac arrest management in the field?
First, patients who have initial shockable rhythms are much more likely to survive than those in PEA or asystole. This is because, unlike for the non-shockable rhythms, we have very effective treatment for VF/VT defibrillation.
“What to do when the VF/VT rhythm persists despite defibrillation?”
But, remember that nothing in medicine is black and white. Survival from VF/VT is more likely, yet this does NOT mean that patient in PEA or asystole can’t survive. You need to use your spidey sense and be a bit of a “detective” to try to determine the potential cause of the PEA/asystolic arrest, especially the narrow complex, “normal” looking PEA. Package and transport needs to be at the top of your treatment plan as there might be a beating heart under all those layers, especially if the monitored heart rate and EtCO2 are compatible with life.
The better survival odds for shockable rhythms is also because asystole is the final, degenerated state. We know response time/downtime is an important determinant of survival in cardiac arrest, and most patients with untreated VF/VT have the rhythm degenerate into asystole in a matter of minutes, especially without CPR being performed.
The very fact that the patient is still in VF/VT when the monitor arrives suggests the response interval to their arrest has been short enough, which improves their chance of survival.
Second, patients who are transported with CPR in progress are much less likely to survive than patients who achieve ROSC at the scene. This demonstrates the importance of a high quality resuscitation at the scene, and de-emphasizes the role of high speed transport to the ED for most patients for whom ROSC is not achieved in the field.
A Special Population
There is, however, a population of patients who do not achieve ROSC at the scene, but for whom the prognosis is much more favourable than others in this cohort: the patient in shock refractory VF/VT (defined as persistent VF or VT after 3 consecutive shocks). When the initial TOR criteria were being carefully studied for derivation and validation, the shock refractor VF/VT group of patients consistently produced survivors, even when ROSC was not established at the scene.
In a study carried out in Montreal and published in 2019, patients with up to 9 preshospital shocks had a survival rate of 8% (1). The survival rate was higher for those requiring fewer shocks.
Clearly this cohort of patients is different than your typical out-of-hospital cardiac arrest patient.
For these reasons, any cardiac arrest patient with an initial shockable rhythm or a shock-refractory rhythm has a much better prognosis, and resuscitation attempts should be aggressive and continued at length, with transportation to hospital strongly considered.
What Are Some Treatment Strategies for Shock Refractory Rhythms?
As paramedics, you know and teach that high quality CPR and early defibrillation have been shown time and again to improve survival in out-of-hospital cardiac arrest from shockable rhythms. But, what to do when the rhythm persists despite defibrillation? This question has been the focus of intense study of late, not the least of which because of the favourable prognosis for these patients. There is new evidence for treatment strategies that might be helpful. Some of these are within the scope of paramedic practice, and some can only be provided at the hospital.
Antiarrhythmics
A study comparing amiodarone vs lidocaine vs placebo for paramedic treatment of shock refractory VF/VT found no difference overall between the treatment and control groups with respect to survival. However, in the subgroup of patients who had witnessed arrests (bystander or paramedics), survival was greater in the treatment groups compared to placebo (2). In the cohort of patients with witnessed cardiac arrest, the medications were administered earlier in the arrest compared with the overall study. This suggests, like epinephrine, that early administration of antiarrhythmics may be important in effective termination of these arrhythmias with resulting ROSC and survival.
Vector Change (VC)
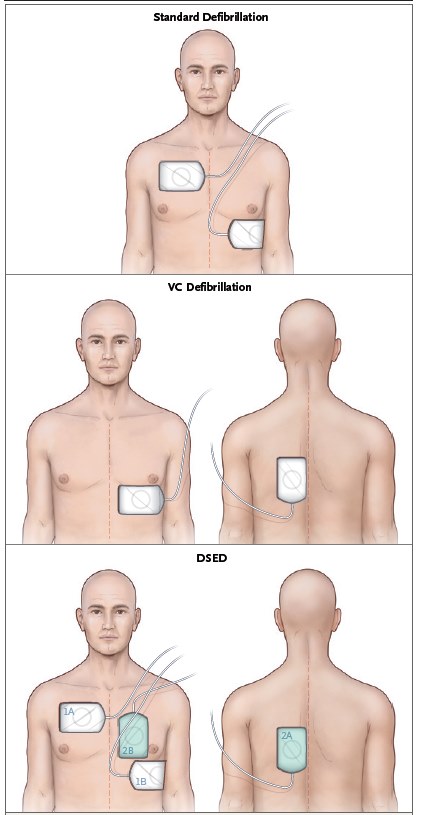
Changing pad positioning when shocks are not working is another option for treating shock refractory VF/VT. By switching pad positioning from the standard anterior-lateral position to anterior-posterior position (see pad placement image below), the voltage gradient across the left ventricle (a posterior structure composing the largest myocardial component of the heart) is greater.
A recent study conducted in Ontario, including patients treated by paramedics in Ottawa, demonstrated improved survival when changes in pad positioning were performed after VF/VT was determined to be refractory to the initial three shocks (21.7% vs 13.3%; 3). Paramedics can implement this change in their practice immediately when faced with a patient in refractory VF/VT.
Double Sequential External Defibrillation (DSED)
The same study that demonstrated survival benefit of VC defibrillation found even greater improvement in survival with DSED (30.4% vs 13.3%). For this technique, two defibrillators are used to deliver two near-simultaneous shocks with pads positioned in the standard anterior-lateral position and anterior-posterior positions (see pad placement image below). It is hypothesized that the added energy of the second shock combined with the change in wave pattern of fibrillation from the first shock make the heart more amenable to defibrillation. In the RPPEO, paramedics who were trained for the study may continue practicing DSED for shock refractory VF/VT, and for those who are not yet trained, expect to hear more about this as we implement the results of this practice-changing study.
Click HERE for full review of Advanced Cardiac Arrest Guidelines.
Beta Blockade
A recent systematic review and meta-analysis of observational studies found patients with shock refractory VF/VT treated with IV beta blockers like esmolol were more likely to survive than those treated with standard therapy alone (4). Standard resuscitation practice includes early epinephrine for cardiac arrest. Epinephrine is a powerful sympathomimetic that stimulates alpha- and beta-adrenergic receptors. The beneficial effects in cardiac arrest are seen with the alpha-adrenergic agonism, with peripheral vasoconstriction directing blood to the central circulation and improving coronary perfusion with CPR which improves rates of ROSC. Beta-adrenergic stimulation may be more problematic, increasing the sensitivity of myocardium to arrhythmias when it is already irritable from ischemia. Countering the pro-arrhythmic effect of epinephrine and any other factors predisposing the myocardium to irritability (like myocardial infarction that caused the initial arrest, for example) is the proposed mechanism by which beta blockers like esmolol can terminate shock refractory VF/VT in cardiac arrest. This is a promising therapy for this challenging condition, and one reason to consider transportation of these patients to the closest ED with CPR in progress.
In the same vein, the potentially deleterious effects of additive doses of epinephrine in these patients is also something to consider and is a question you can ask your BHP about if you elect to patch. Some BHPs will recommend limiting doses of epinephrine in refractory VF/VT for the reasons above. An additional concern is that higher doses of epinephrine appear to have a negative effect on outcome, possibly related to vasoconstriction of and reduced blood flow to the brain, although there is not currently enough evidence to make a firm recommendation for this one way or the other. This is a question an upcoming study with participants from the RPPEO region is hoping to answer.
Extracorporeal Membrane Oxygenation (ECMO) and PCI
One promising new therapy for shock refractory VF/VT that is still in experimental stages but that might be a future indication for rapid transportation to a tertiary care centre is ECMO followed by emergent PCI. By placing the patient on artificial life support with mechanical blood circulation, time is bought to reverse the cause of the arrhythmia – typically acute coronary artery occlusion – with PCI. Early studies are promising (5).
What Does This Mean For Timing of Transportation?
It should be clear from the information presented above that patients with cardiac arrest from VF/VT have a much more favourable prognosis. For this reason alone, aggressive and lengthy resuscitation is indicated and strong consideration should be given to transportation to hospital.
For the subgroup of patients who remain in VF or VT despite standard ACLS, you can attempt VC defibrillation, DSED for paramedics trained in this, and rapid transportation to the closest ED for consideration of beta blocker therapy.
For these reasons the ALS PCS 5.2 Medical Cardiac Arrest Directive states: For patients in refractory VF or pulseless VT, transport following 3 rounds of epinephrine (or after 3rd consecutive defibrillation if no IV/IO/CVAD/ETT access).
Importantly, there is no need to spend 20 minutes on scene resuscitating this patient population (more on this later). In fact, VF/VT patients are just one subgroup of patients for whom a favourable prognosis or treatments that can only be provided in the ED should lead to consideration of early transportation. Others in this category include patients in cardiac arrest who have a pregnancy greater than 20 weeks gestational age, patients for whom hypothermia might have caused the arrest, patients with an airway obstruction the paramedic cannot clear, and those with a drug overdose for which ED treatments could be beneficial (beta blockers, calcium channel blockers, digoxin, etc).
Think also about your patients who have an arrest witnessed by the paramedic, or those in fast “good looking” PEA with an ETCO2 compatible with life. Importantly, if the paramedic has decided that the patient has a potential for survival and will benefit from transportation, this can be initiated at the soonest opportunity, once treatments beneficial at the scene are exhausted. There is no requirement to resuscitate on scene for a specific period of time if your interventions are exhausted and you believe transport is indicated. To transport is in your toolbox of treatment options now that you have a better understanding of what the ED can do to assist your patient.
There is also no requirement for a patch in this circumstance. You are welcome to patch to a BHP if you have questions about treatment or the timing of transportation, but if you have no questions and have elected to transport to hospital, please do not spend time patching unless you feel it will benefit you or the patient.
So Where Did This 20 Minute On-Scene Resuscitation Come From?
Most patients who survive out-of-hospital cardiac arrest have ROSC at the scene, and very few patients transported with CPR in progress will survive. Unless there is a beneficial intervention that can be provided in the hospital that is not available to prehospital providers, or the patient has favourable prognostic factors like those mentioned above, we recommend aggressive on scene resuscitation without prioritizing transportation.
The question for these patients then becomes “How long should the resuscitation continue with no response before ongoing efforts are determined to be futile?”
Initial studies validating the TOR criteria were done in Ontario, and found that for patients with unwitnessed arrest, no shocks, and no ROSC at the 6 minute mark of the resuscitation, only 1/200 (0.5%) survive if the resuscitation continued (6).
When these criteria were studied in British Columbia, a province where on-scene resuscitations are routinely continued for longer, it was found that for patients meeting the TOR rule, 2% survived if the rule was applied at the 6 minute mark but resuscitation continued, compared with 1% at 20 minutes, and no survivors at 30 minutes (7).
This raised the concern that even for those patients for whom ongoing resuscitation seems futile, if resuscitation is terminated too early, we might be missing survivors (i.e., terminating resuscitation on a patient who would have survived had resuscitation continued). The longer the resuscitation continued with no shocks and no ROSC, the less likely the patient is to survive. Making decisions at the 6 minute mark seemed too soon. To be safe, we decided to recommend scene resuscitation for 20 minutes before considering patching for TOR in patients for whom the prognosis seems poor, to avoid terminating too early on potential survivors.
To be clear, the 20 minute condition for TOR applies to patients who do not have favourable prognostic factors and for whom on-scene termination is being considered. For patients who you are electing to transport, there is not amount of on-scene time required before moving, and there is no requirement for a patch.
In some cases, it might be reasonable to consider TOR prior to 20 minutes of resuscitation. Think of your elderly patient found down with an unwitnessed arrest and who remains in asystole despite your initial efforts. Loved ones may be openly contemplating if the patient would want chest compressions and rescucitative efforts. When the prognosis is extremely poor and it is not clear if ongoing resuscitation has any hope of meaningful benefit, and you are considering early termination feel free to patch to a BHP to discuss.
The ALS PCS directives are meant to provide guidance that is helpful for patients and paramedics, and if you believe a different approach is in the patient’s best interests, please feel free to discuss with a BHP at any time.
Case Resolution
Your patient remains in VF. You administer a dose of lidocaine as soon as possible after the second shock. The patient remains in VF and the third shock is ineffective. You continue CPR and make preparations for rapid transportation at the soonest opportunity. For the fourth shock you can change pad positioning from the anterior-lateral to anterior-posterior position. On your next analysis there is an organized rhythm on the monitor with a pulse. You continue with post-ROSC care and transport the patient to hospital.
References
- Alexis Cournoyer et al., 2019. The prognostic significance of repeated prehospital shocks for out-of-hospital cardiac arrest survival. Canadian Journal of Emergency Medicine, Volume 21, Issue 3, pp. 330 – 338 DOI: https:// doi.org/10.1017/cem.2018.437
- Peter Kudenchuk et al., 2016. Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. New England Journal of Medicine, Volume 374, pp. 1711-1722. DOI: 10.1056/NEJMoa1514204
- Sheldon Cheskes et al., 2022. Defibrillation Strategies for Refractory Ventricular Fibrillation. New England Journal of Medicine, Volume 387, pp. 1947-1956. DOI: 10.1056/ NEJMoa2207304
- Michael Gottlieb, Sean Dyer, and Gary D Peks, 2019. Beta- blockade for the treatment of cardiac arrest due to ventricular fibrillation or pulseless ventricular tachycardia: A systematic review and meta-analysis. Resuscitation. Volume 146, pp. 118-125. DOI: 10.1016/ j.resuscitation.2019.11.019.
- Demetris Yannoupolis et al., 2020. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. The Lancet, Volume 396 (10265), pp. 1807-1816. DOI: 10.1016/S0140-6736(20)32338-2.
- Laurie J. Morrison et al., 2009. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation, Volume 80 (3), pp. 324-8 DOI: 10.1016/ j.resuscitation.2008.11.014.
- Brian Grunau et al., 2017. External Validation of the Universal Termination of Resuscitation Rule for Out-of- Hospital Cardiac Arrest in British Columbia. Annals of Emergency Medicine, Volume 70 (3), pp. 374-381. DOI: 10.1016/j.annemergmed.2017.01.030.