We know that management of the patient in cardiac arrest can be difficult. As emergency providers, we often rely on an algorithmic approach because of limited information. Point of Care Ultrasound (POCUS) has offered an unprecedented ability to diagnose and monitor these patients in real time – but how can we practically use this information during a code? What does the evidence tell us about outcomes based on POCUS/Echo findings in cardiac arrest?
Transthoracic Echo in Cardiac Arrest
Pulmonary Embolism
- PE is the etiology of ~5% of cardiac arrests, and if detected early, the potential for ROSC is much higher when given thrombolytics (81 vs. 43%).1
- To date, the only study examining the diagnostic accuracy of POCUS for PE in ED patients demonstrated the following:2
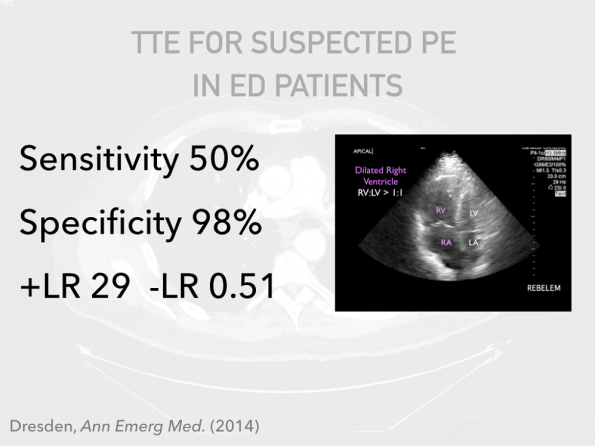
- Multiple guidelines state that in an arrest setting, absence of POCUS findings for RV strain preclude PE as a cause of arrest, and conversely, that the presence of these findings in a patient with suspected PE can justify use of thrombolytics.3, 4
- That said, there are many potential false positives for RV strain in our sick ED patients, including Right-sided MI, COPD, OSA, Pulmonary Hypertension, and left sided valve disease.
Bottom Line:
There is no evidence that we can reliably diagnose PE in cardiac arrest patient using TTE. But, if there are immediate signs of RV dilation/ dysfunction in a suspicious clinical context, you can consider using lytics–just remember to be wary of potential false positives.
Cardiac Activity aka “Pseudo PEA”
- Our accuracy at palpating for a pulse may be as low as 78% 5, and may take longer than 5 seconds even in healthy volunteers. 6
- Despite the absence of a pulse with a PEA rhythm, POCUS may demonstrate organized cardiac activity–this scenario is described as “Pseudo PEA”.
- A systematic review in 2012 found that the presence of cardiac activity had a rate of ROSC of 51.6% compared to patients with cardiac standstill (only 2.4%). 7
- More recently, a randomized control trial in 2016 found that the presence of cardiac activity during arrest confers a significantly higher rate of ROSC, survival to admission, and survival to discharge. 8
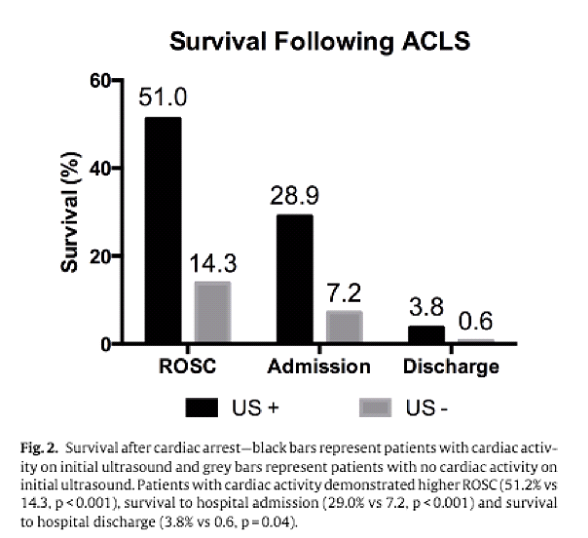
Bottom Line:
POCUS is a useful tool to adjust probability of ROSC in the context of other prognostic factors like witnessed arrest and bystander CPR. It has been repeatedly shown that absence of cardiac activity does not definitively predict futility of resuscitation.
ACLS+POCUS protocols
- Many algorithms have been proposed to incorporate POCUS into life-saving protocols9-12 but none have conclusively demonstrated an improvement in patient-centered outcomes such as neurologically intact survival.
- The updated 2015 AHA Guidelines for ACLS state that POCUS may be used to help identify reversible causes of arrest so long as it doesn’t otherwise interfere with high quality ACLS care, whether by prolonging pulse checks, or distracting from CRM principles. 13
Transesophageal Echo in Cardiac Arrest
Despite its promise, transthoracic echo views have several limitations–patient factors like obesity or subcutaneous air can prevent image generation. It also takes up space on the chest and can distract from proper CRM management, or worse, prolong hands-off time.
Emergency department transesophageal echocardiography (ED-TEE) may be the next step that gives us fast, reliable, clear images, unaffected by the aforementioned patient factors while simultaneously freeing up space during resuscitation. Because it is meant to be left in place during ACLS, it should lead to easier serial views and shorter pulse checks looking for cardiac activity. Novel uses include the ability to continuously monitor compressions, and looking for both depth and adequacy of LV compression. 14
Demystifying TEE
- Although TEE may seem complicated–conjuring up images of complicated cardiology echo reports–the truth is ED-TEE can be as simple as a 4-view protocol, with images that are analogous to the TTE views you already know and love.
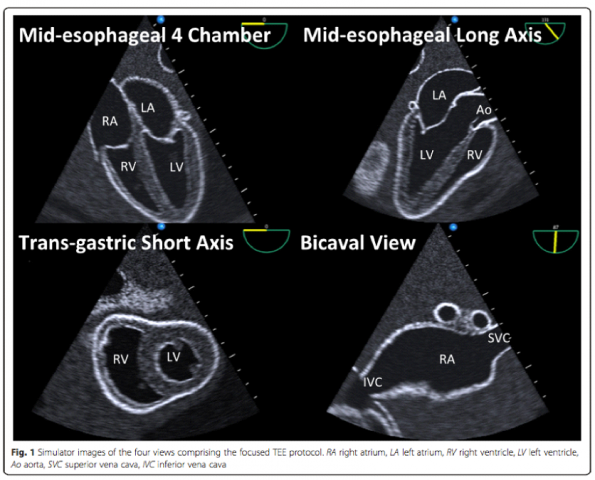
Image from Arntfield, Crit Ultrasound J (2015). 15
- Remember, this is not the same as a formal echo. Ideally you will have a focused protocol to quickly answer simple clinical questions–presence of effusion, global ventricular function, RV-dilation, volume assessment and procedural guidance.
- There is published data that emergency physicians who were TEE-naive can be trained in just 4 hours with good skill retention at six weeks. 15
TEE: Evidence in Cardiac Arrest
- This isn’t exactly a novel idea–in fact a small prospective observational study in 1997 of in-hospital cardiac arrests (including ED) found that TEE diagnosed pathology in 64% of cases, while changing care in 31%. 16
- Last year, Dr. Rob Arntfield published the largest series of emergency physician TEE examinations yet reported. 17 It is also the first known ED TEE program to be described, and the first description of an in vivo use of a four-view, focused TEE protocol. He found TEE led to a diagnostic influence in 78% of cases, and more importantly, a therapeutic impact was present in 67% of cases. Almost half the cases were intra-arrest, and a significant proportion of these exams led to direct improvement in quality of CPR; misplaced vector of force, identification of chest compressor fatigue, shortened pulse-check duration, and identification of ROSC during CPR were all described.
Bottom Line:
There is promising data that ED-TEE is diagnostically and therapeutically useful during cardiac arrest.
Safety of ED-TEE
- Generally speaking, complications are related to injuries to GI tract, bleeding, dysrhythmia, intubation related, oropharyngeal/laryngeal injury and even solid organ injury. 18
- A number of ICU studies have evaluated TEE to be very safe in the critically ill patient with close to zero mortality and <4% rate of complications. 19, 20, 21, 22, 23
- However, a 1999 study of ED patients undergoing TEE found the complication rate may be as high as 12.6%–mostly driven by respiratory complications, hypotension, and emesis. 24 That said, the more recent Arntfield paper found that there were no aerodigestive injuries. 15
Bottom Line:
ED-TEE is probably as safe as an NG tube,25 and likely more safe than a central line. 26
Summary
- TTE can be helpful in cardiac arrest, but evidence for routine use is lacking.
- TEE has several potential advantages to TTE, and evidence is promising for its use in cardiac arrest.
In my humble opinion – I submit to you that TEE is probably a better tool to use in cardiac arrest and is a realistic possibility in a well-functioning academic Emergency Department like ours. I recognize that the evidence is slim right now, and it may seem difficult to justify the resources of a TEE program, however I think it’s important that we consider- what do we want a 21st century resuscitation to look like?
References



Trackbacks/Pingbacks