This post is a continuation of a previous post about anorectal issues in the ED. Here, we will discuss anorectal abscess, surrounding complications, and necrotizing infections.
Anorectal Abscess
- Anorectal abscesses are thought to occur from the plugging of anal glands, resulting in infection and purulent collection that spreads along one of several potential spaces.1
- Abscesses are classically divided into four categories:
- Peri-anal: superficial, visible on external inspection, and do not extend into any deep rectal or pelvic space.
- Ischiorectal: transverse the external anal sphincter and extend into the ischiorectal space.
- Intersphincteric: contained between the internal and external anal sphincters (often not visible on inspection).
- Supralevator: proximal to the internal anal sphincter and are not visible on external inspection.2
- Anorectal abscesses can present anywhere from constant, dull, aching pain worsened by defecation, walking, and deep breathing, to anorectal sepsis.
- Management is always surgical, whether it be incision and drainage or otherwise.1
Of note, the formation and recurrence rate of anal fistula is quite high, with a 50% chance of one or the other happening within one year of initial abscess drainage.2 These odds do not seem to be operator- or specialty-dependent and do not seem to change if a fistula is identified and treated on the initial presentation or on followup.1

Perianal fistula. From Grucela A, Salinas H, Khaitov S, Steinhagen RM, Gorfine SR, Chessin DB. Prospective analysis of clinician accuracy in the diagnosis of benign anal pathology: comparison across specialties and years of experience. Diseases of the colon and rectum, 2010.
Perianal abscesses can and should be drained in the ED.3 Drainage is similar to uncomplicated abscesses on other sites: generous local anesthesia, incision, drainage, with the wound left open to heal by secondary intention. An elliptical incision or a cruciate incision with flap excision should be used, made as close as possible to the external sphincter. The patient should be advised that the abscess may continue to drain for 2-3 weeks.1

Perianal abscess. From Grucela A, Salinas H, Khaitov S, Steinhagen RM, Gorfine SR, Chessin DB. Prospective analysis of clinician accuracy in the diagnosis of benign anal pathology: comparison across specialties and years of experience. Diseases of the colon and rectum, 2010.
- Intersphincteric and supralevator abscesses are less common, comprising 21% and 7% of anorectal abscesses respectively.2 The ED diagnosis of these ‘occult’ abscesses remains challenging. As they are not visible on inspection, a DRE is recommended in instances where a deep space abscess is suspected.
- Pain on DRE or high clinical suspicion should trigger advanced imaging. Unfortunately, imaging test characteristics are not well delineated in the literature. The American Society of Colon and Rectal Surgery (ASCR) recommends CT with contrast, followed by MRI for a negative scan with high suspicion, but the evidence cited in guidelines is not ideal.4
- A single, retrospective, case series of 113 patients5 demonstrated a sensitivity of 77% for CT with contrast. Of note, this study included only patients already diagnosed with anorectal abscesses and did not describe the location of missed abscesses or patient demographics.
- Data on MRI test characteristics is similarly lacking: 2 papers are essentially small case series in patients with diagnosed abscess, with no patient demographics to guide clinical decision making.6,7
![]() Fournier’s Gangrene
Fournier’s Gangrene
- A necrotizing soft tissue infection of the perineal and urogenital region, first formally described by Fournier in 1883.8
- An initial insult and bacterial proliferation causes endarteritis obliterans, or thrombosis of the microcirculation. The resulting acidic environment encourages rapid bacterial spread through sterile spaces (classically fascial planes), fulminant necrosis, and overwhelming inflammatory response.
- The time from initial insult to fulminant necrosis can be anywhere from 2 to 7 days.9
- Depending on the degree of progression, patients may present with a range of symptoms; from erythema and crepitus to frank necrosis and anorectal sepsis.
- It is 10 times more common in males than females, but even so, a 2009 American population survey found an incidence of 1.6 per 100,000 males.
- Mortality, despite modern standard of care, remains between 20 and 30%.10
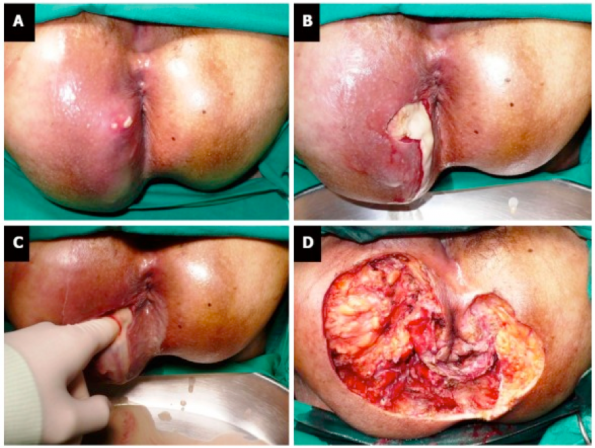
Progression of Fournier’s gangrene. From Lohsiriwat V. Anorectal emergencies. World journal of gastroenterology, 2016.
Although Fournier’s gangrene is associated with urogenital insults, multiple anorectal sources of infection exist: Shyam et al. describe some of the most common sources as hemorrhoidectomy, perianal abscess, and thrombosed hemorrhoid. 9
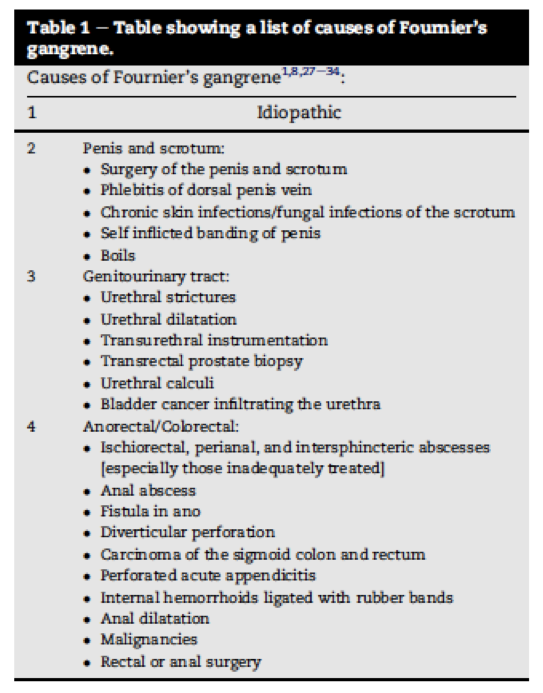
Causes of Fournier’s gangrene. From Shyam DC, Rapsang AG. Fournier’s gangrene. The Surgeon, journal of the royal colleges of surgeons of Edinburgh and Ireland, 2013.
- ED management of Fournier’s gangrene is straightforward: urgent surgical consultation and broad-spectrum antibiotics.
- Diagnosing this process can present a significant dilemma, given both its rarity and the spectrum on which patients may present.
- Case series describe classical clinical findings but evidence to guide advanced imaging and surgical consultation is lacking.9
More generally speaking, the best evidence describing clinical, biochemical, and imaging test characteristics is found in a recent publication by Fernando et al. regarding necrotizing soft tissue infections as a group.11 In a systematic review and meta-analysis, the authors underscore the dearth of high-grade evidence and the anecdotal nature of ‘classical’ findings. In the studies identified, only 3 clinical examination findings could be included in meta-analysis: fever, hemorrhagic bullae, and hypotension. Sensitivities were not ideal: 46% (fever), 25% (hemorrhagic bullae), 21% (hypotension). The sensitivity of the laboratory risk indicator for necrotizing fasciitis (LRINEC) score for biochemical markers (68% for a score of 6 or higher; 41% for 4 and under) and plain radiograph (49%) were similarly underwhelming. Contrast CT detecting fascial gas performed better, at 88.5% sensitivity; when the authors included contrast CT scans that identified gas or fascial edema or fascial enhancement, sensitivity rose to 94%.
Take Home Points
Anorectal abscesses:
- Consider drainage of simple perianal abscesses in ED
- No packing
- No antibiotics
- No imaging
- When ordering imaging, recall the moderate sensitivity of CT with contrast to avoid anchoring and premature closure biases
- Counsel patients about their risk of recurrence and fistulae
- Refer all abscesses drained in ED to outpatient General Surgery
Fournier’s gangrene
- Consider anorectal causes of infection
- Recall the lack of evidence guiding clinical exam and laboratory investigations to avoid missed diagnoses
- Speak to the interpreting radiologist about ‘pragmatic’ CT findings: fascial edema or enhancement
- Involve your surgical consultants early
References
- Pigot F. Treatment of anal fistula and abscess. Journal of visceral surgery, 2015
- Rizzo JA, Naig AL, Johnson EK. Anorectal abscess and fistula-in-ano: evidence-based management. Surgical clinics of North America, 2015
- Personal communication, Dr H Moloo
- Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL, Steele SR. The American society of colon and rectal surgeons clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Diseases of the colon and rectum, 2016
- Caliste X, Nazir S, Goode T, Street JH, Hockstein M, McArthur K, Trankiem CT, Sava JA. Sensitivity of computed tomography in detection of perirectal abscess. The American surgeon, 2011
- Maruyama R, Noguchi T, Takano M, Takagi K, Morita N, Kikuchi R, Uchida Y. Usefulness of magnetic resonance imaging for diagnosing deep anorectal abscesses. Diseases of the colon and rectum, 2000
- Garcia-Granero A, Granero-Castro P, Frasson M, Flor-Lorente B, Carreño O, Espí A Puchades I, Garcia-Granero E. Management of cryptoglandular supralevator abscesses in the magnetic resonance imaging era: a case series. International journal of colorectal disease, 2014
- Fournier JA. Gangrene foudroyante de la verge. Republished in Diseases of the colon and rectum, 1988
- Shyam DC, Rapsang AG. Fournier’s gangrene. The Surgeon, journal of the royal colleges of surgeons of Edinburgh and Ireland, 2013
- Sorenson MD, Krieger JN, Rivara FP, Broghammer JA, Klein MB, Mack C, Wessells H. Fournier’s gangrene: population based epidemiology and outcomes. Journal of urology, 2011
- Fernando SM, Tran A, Cheng W, Rochwerg B, Kyeremanteng K, Seely AJE, Inaba K, Perry JJ. Necrotizing soft tissue infection: diagnostic accuracy of physical examination, imaging, and LRINEC score: a systematic review and meta analysis. Annals of surgery, 2019