Tick. Tock. It’s time for a TXA update. This blog post aims to arm you with the most up-to-date knowledge for the use of tranexamic acid (TXA) in the ED. We will review TXA in the context of gastrointestinal bleeding, traumatic brain injuries, hemoptysis, intracranial hemorrhage, and trauma.
Please note, for evidence on the use of TXA in epistaxis, heavy menstrual bleeding, or for an in-depth review of the CRASH-2, MATTERs trials, and CRASH-3 please refer to the Grand Round summaries by Dr. J-C Ghazal (2015), Dr. Lauren Frutcher (2018) and Dr. Krishan Yadav (2019).
Part I: TXA Basics
Mechanism of Action
-
- The primary goal of TXA is to stop bleeding via inhibition of fibrinolysis;
- TXA is a synthetic lysine derivative – thus it binds to the lysine site on plasminogen. Therefore plasminogen’s interaction with fibrin is prevented, and the breakdown of fibrin clots inhibited – in other words – It stabilizes a clot that has already formed.
Pharmacy
-
- Available formulations: IV, PO, and nebulized;
- Half-life (IV): 2 hrs;
- Advantages: Readily available, inexpensive (approx. $6.00/1g);
Uses
-
- Approved Use: FDA approved for use in hemophilia and heavy menstrual bleeding;
- Off-label Use: Dentistry, orthopedic and cardiac surgery, epistaxis, hereditary angioedema, and many more!
Adverse Effects
-
- GI symptoms
- Headache
- Seizure
- Hypotension (especially with rapid IV injection)
- Thrombosis
Contraindications
-
- Known hypersensitivity
- Current or prior history of thrombosis
- Hypercoagulable states
- Subarachnoid hemorrhage (Note: this is controversial)
Part II: Indications for Use
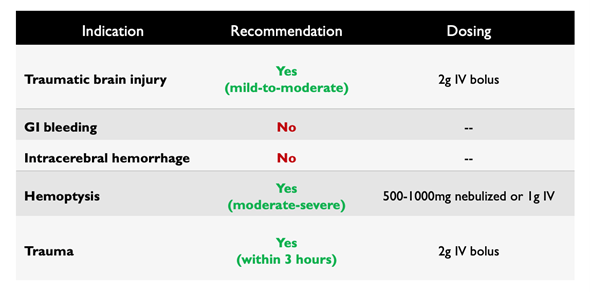
Based on the results of the CRASH-2 and MATTERs trials1,2, which showed that TXA reduces mortality in trauma patients, interest was sparked for the use of TXA for many other indications. These include but are not limited to traumatic brain injury (TBI), gastrointestinal (GI) bleeding, intracerebral hemorrhage (ICH), and hemoptysis.
Traumatic Brain Injury
Background
-
- TBI is a common and potentially devastating disease, affecting more than 452 people in Canada every day.
- Severity is categorized based on Glasgow Coma Scale (GCS):
- Mild = GCS 13-15
- Moderate = GCS 9-12
- Severe = GCS <9
- Increased fibrinolysis is part of the coagulopathy of TBI, with hemorrhage expansion occurring in the first few hours after injury, and larger hematomas being associated with increased mortality.
- TXA use in TBI is based on the theory that TXA might limit secondary brain injury via two pathways:
- It may limit fibrinolysis and therefore ICH progression
- It may inhibit the effect of tissue plasminogen activator (tPA), which is involved in peri-lesional edema
Evidence
-
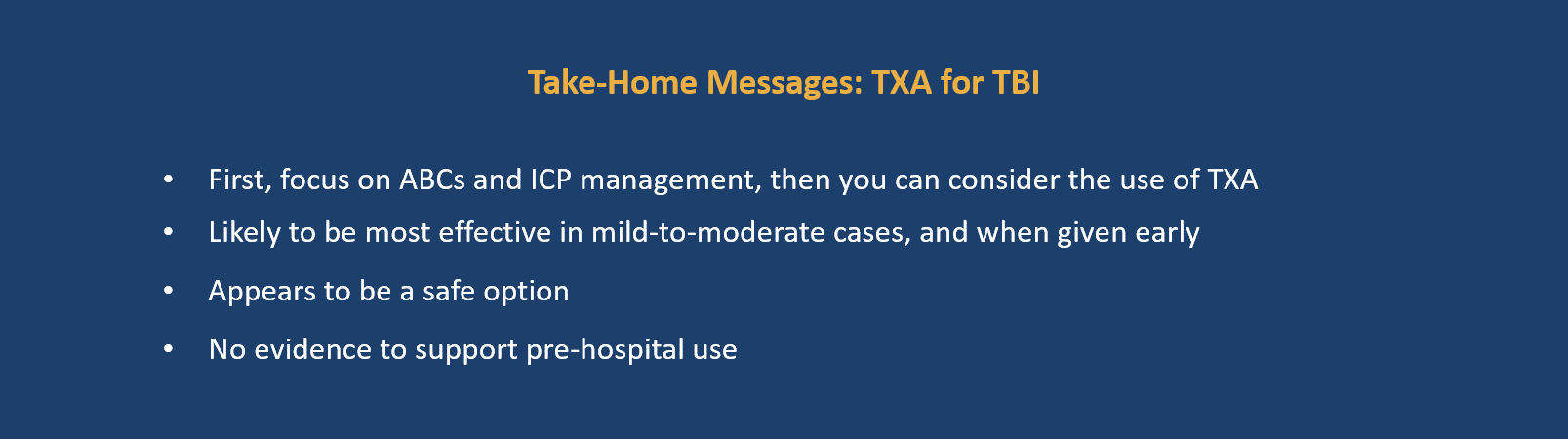
- A systematic review and meta-analysis by July et al3, evaluated 7 RCTs investigating the effect of TXA in TBI. They found an overall lower risk of death (RR 0.92, NNT of 71), and decreased rate of hemorrhage expansion (RR 0.79, NNT of 16), in the TXA groups. The CRASH-3 trial was included in this review.
- CRASH-3 Trial:
- Large RCT examining the effect of TXA in patients with TBI
- Study Design: Enrolled 12, 737 adult patients with TBI within 3 hours of injury
- Intervention arm: TXA 1g IV over 10 minutes, followed by 1g IV over 8 hours
- Control arm: Matched placebo (IV normal saline)
- Outcomes:
- Primary Outcome: Head-Injury related deaths in the hospital within 28 days
- Secondary Outcomes: Head-injury related deaths within 24hrs, all-cause mortality, vaso-occlusive events, and seizures, among others.
- Results:
- Head-injury related death at 28 days (Primary Outcome): NO SIGNIFICANT DIFFERENCE between groups (RR 0.94, 95% CI 0.86-1.02), even when excluding those with GCS 3 or bilateral fixed pupils (i.e. those who already had a poor prognosis and were unlikely to benefit from TXA) (*RR 0.89, 95% CI 0.80-1.00)
- Mild-moderate head injury: SIGNIFICANTLY DECREASED RATE OF HEAD INJURY RELATED DEATH AT 28 DAYS in TXA group (RR 0.78 CI 0.64-0.95). Earlier time to treatment was also found to be significantly more effective than later treatment in this subgroup (see Figure below). Time to treatment did not affect head-injury related deaths in those with severe TBI.
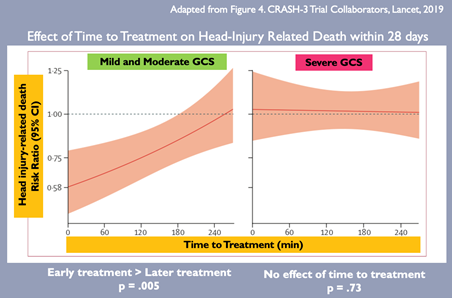
-
-
-
- Secondary Outcomes: there was a SIGNIFICANT DECREASE IN HEAD-INJURY RELATED DEATH AT 24 HOURS (RR -0.81, 95% CI 0.69-0.95). However, there were no significant changes in all-cause mortality, or in the risk of vaso-occlusive events or seizure.
- Conclusions:
- The authors concluded that TXA is safe to be used in patients with TBI and that treatment within 3 hours of injury reduces head-injury related death…but this is somewhat misleading…the reduction in head-injury related deaths was limited to a specific subgroup of patients with a mild-to-moderate head injury, and those at 24hours. The conclusions drawn from this trial should reflect this.
- Limitations:
- Change in primary outcome during the study from head injury-related death for patients treated within 8 hours to those treated within 3 hours of injury
- Failure to meet their updated targeted sample size to account for the change in the primary outcome
-
- Mahmood et al. (2020)5
- Separate sub-study on the CRASH-3 patients
- Evaluated the rates of hemorrhage expansion and new hemorrhage formation for patients in each group
- TXA significantly reduced new hemorrhage formation (p=0.03) in patients with bilateral reactive pupils but did not significantly affect the hemorrhage expansion or progression (p=0.62), again demonstrating that patients with less severe TBI appear to be the most likely to benefit from TXA. This is likely because patients with severe TBI already have large volumes of intracranial bleeding and significant coagulopathy, at which point TXA likely has little room to work.
-
Pre-Hospital TXA in TBI
Two recent trials were published on the role of pre-hospital TXA in TBI
-
- Rowell et al. (2020)6
- RCT (N=1280), TXA versus placebo
- Failed to find any significant difference in favorable neurological outcome at 6 months in patients with moderate-to-sever TBI who received TXA within 2 hours of injury (difference 3.5%, p=0.16)
- Bossers et al. (2020)7
- Observational trial (N=1827)
- Found TXA to be associated with increased 30-day mortality in patients with severe isolated TBI (OR 4.49%, 95% CI 1.57-12.87,p=0.005) (not, causality cannot be inferred based on the observational nature of the trial)
- Rowell et al. (2020)6
Conclusion:
Currently there is no clear benefit to the use of pre-hospital TXA in TBI
Expert Opinion
-
- Dr. Luis Da Luz (MD, MSc, FRCSC, General Surgeon, Trauma Team Leader, Sunnybrook Health Sciences Center) recommends:
- Regular use of TXA for patients with isolated TBI if:
- GCS <14, or
- If there is a high index of suspicion for bleed
- If in doubt as to the cause of the decreased GCS:
- Wait for imaging (CT head), and administer TXA if there is a bleed present on the imaging
- Do not regularly use of TXA if:
- Very small traumatic SAH in a patient who is neurologically intact, as the risk of hemorrhage expansion on subsequent CT is very small in these cases.
- Regular use of TXA for patients with isolated TBI if:
- Dr. Luis Da Luz (MD, MSc, FRCSC, General Surgeon, Trauma Team Leader, Sunnybrook Health Sciences Center) recommends:
Gastrointestinal Bleeding
Background
-
- GI bleeds are a common presentation to the ED, with case fatality rates as high as 14% even with our current treatments
Evidence
-
- Cochrane Review (2014)8
- Included 8 RCTs investigating TXA in upper GI bleeds (UGIB), N=1701
- Found TXA to be associated with a mortality benefit (NNT of 29), and a reduction in rates of rebleeding
- Overall quality of evidence = moderate-to-low, significant bias in the studies included
- Concluded that more evidence was needed before using TXA for UGIB
- HALT-IT (2019)9
- International RCT (N=12,009) on adults with significant upper or lower GI bleeding
- Intervention arm: TXA 1g IV over 10 minutes, followed by 3g IV over 24 hours
- Control arm: Matched placebo (IV Normal Saline)
- Outcomes:
- Primary: Death due to bleeding within 5 days
- Secondary: Death due to bleeding within 24 hours and 28 days, rates of rebleeding up to 28 days, the need for endoscopy, surgical intervention, or blood product transfusion, and various complications, among others.
- Results:
- Death due to bleeding at 5 days (primary outcome): no significant difference between groups (RR 0.99, 95% CI 0.82-1.18)
- All-cause mortality: no significant difference between groups (RR 1.03, 95% CI 0.92-1.16)
- Secondary outcomes:
- No significant differences between groups with respect to rates of rebleeding, total amount of blood products transfused, the need for surgery, endoscopy, or transfusion, or rates of arterial thromboembolism
- Doubling of the risk of VTE (including DVT and PE) in the TXA group (0.8% versus 0.4%, NNH = 250)
- Slightly increased risk of seizures (0.6% versus 0.4%, NNH of 500)
- Conclusions:
- TXA does not reduce death due to GI bleeding and may increase the risk of VTE and seizures
- TXA is currently not recommended for patients with GI bleeds
- Limitations:
- Change in primary outcome from all-cause mortality at 28 days to death due to bleeding within 5 days, however, this likely did not affect results
- International RCT (N=12,009) on adults with significant upper or lower GI bleeding
- Cochrane Review (2014)8
Expert Opinion
-
- Dr. Jeff McCurdy (MD, PhD, FRCPC, Gastroenterology, The Ottawa Hospital)
- “I recommend AGAINST its use for the vast majority of cases…The current weight of evidence suggests more harm than good.”
- Dr. Jeff McCurdy (MD, PhD, FRCPC, Gastroenterology, The Ottawa Hospital)

Spontaneous Intracerebral Hemorrhage
Background
-
- Spontaneous (non-traumatic) ICH is bleeding into the parenchyma of the brain itself resulting from a diseased blood vessel (excludes epidural, subdural, or subarachnoid hemorrhages)
- Hematoma expansion is seen in 25% of cases and has been independently associated with death and poor outcomes, accounting for half of the deaths related to stroke.
Evidence
-
- TICH02 (2018)10
- RCT (N=2,325) on adults with spontaneous ICH, presenting within 8 hours of symptom onset
- Study Design:
- Intervention Arm: TXA 1g I, followed by 1g IV over 8 hours
- Control Arm: Matched placebo (IV Normal Saline)
- Outcomes:
- Primary outcome: Functional status at 90 days (on modified Rankin Scale)
- Secondary outcomes: Hematoma expansion at 48 hours, change in hematoma volume at 24 hours, mortality at 7 and 90 days, safety outcomes up to 90 days, among others
- Results:
- Functional status at 90 days (primary outcome): NO SIGNIFICANT DIFFERENCE between groups (aOR 0.88, 96% CI 0.76-1.03, p=0.11)
- Secondary outcomes:
- Mortality at 7 days: significantly reduced (9% vs 11%, p=0.04, NNT = 54)
- Mortality at 90 days: no significant difference (22% vs 21%, p =0.37)
- Rate of hematoma expansion at 48 hours: significantly reduced (25% vs 29%, p=0.03, NNT 31)
- Volume of hematoma expansion at 24 hours: significantly reduced (delta 1.2mL, p=0.04), but this is unlikely to be clinically significant.
- Serious adverse events: no significant differences in any serious adverse events (including venous and arterial occlusive events, or seizure)
- When considered overall: significantly fewer serious adverese events at 90 days in the TXA group (44.9% vs 47.8%, p=0.039)
- Conclusions:
- TXA DOES NOT significantly improve functional status at 90 days in patients with ICH, despite a reduction in early deaths and serious adverse events
- Limitations:
- Choice of inclusion time of up to 8 hours after symptom onset
- The median time to randomization was approximately 4 hours, at which point only a small percentage of patients would have still been bleeding
- Choice of inclusion time of up to 8 hours after symptom onset
- TICH02 (2018)10
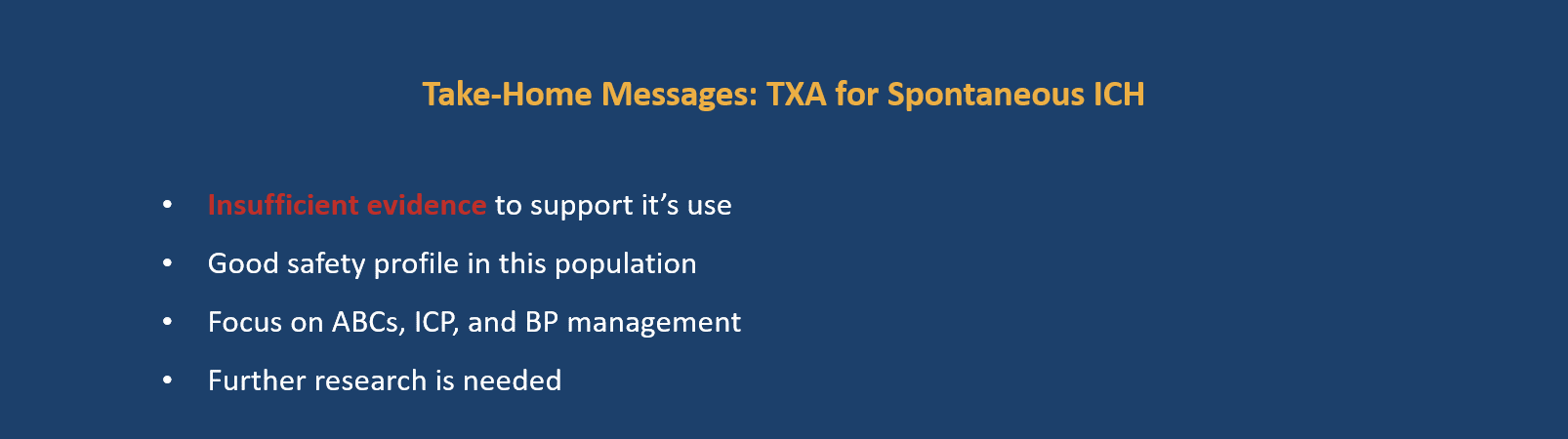
Expert Opinion
-
- Dr. Dar Dowlatshahi (MD, PhD, FRCPC, Stroke Neurologist, The Ottawa Hospital)
- Suspects TICH-2 was an overall negative trial because they studied the wrong time window
- The rule of thumb is that hemorrhage expansion will occur within the first 6 hours of insult, with only about 10% still expanding at that point…the sweet spot is really within the first 2 hours
- Insider scoop on 2022 AHA Guidelines
- There is insufficient evidence to recommend the use of TXA in emergency settings for spontaneous ICH, but could be considered in exceptional circumstances, given its good safety data
- Dr. Dar Dowlatshahi (MD, PhD, FRCPC, Stroke Neurologist, The Ottawa Hospital)
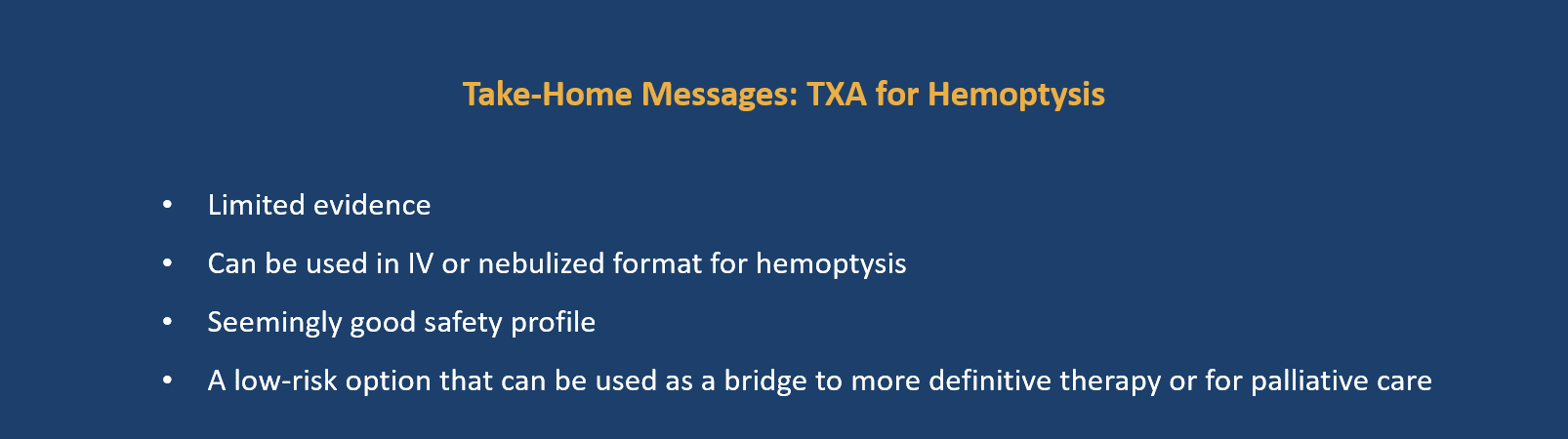
Hemoptysis/Pulmonary Hemorrhage
Background
-
- Hemoptysis refers to bleeding from the major airways, or from the lung parenchyma itself
- Most common causes: lung cancer, bronchiectasis, pulmonary infection
- Categorized based on the volume of bleeding
- Non-massive = <200mL in 24 hours
- Massive = >200mL in 24 hours
- Current definitive therapies include:
- Bronchoscopy with iced saline or epinephrine
- Balloon tamponade
- Electrocautery
- Arterial embolization
- Surgical intervention
- Current therapies are most useful when the bleeding source can be identified, but when the source is unknown, therapies are essentially limited to airway management and correcting coagulopathy
Evidence
-
- Cochrane Review (2016)11
- Only 2 RCTs found that looked at the use of TXA in hemoptysis
- Ruiz (1994)12 (N = 24) – IV TXA x 3 days in hemoptysis due to TB
- Tscheikuna et al. (2002)13 (N = 46) – Oral TXA x 7 days for various etiologies
- Neither study found TXA to lead to remission of bleeding by 7 days
- When pooled together, there was a significant difference in the duration of bleeding, with no adverse events reported
- Only 2 RCTs found that looked at the use of TXA in hemoptysis
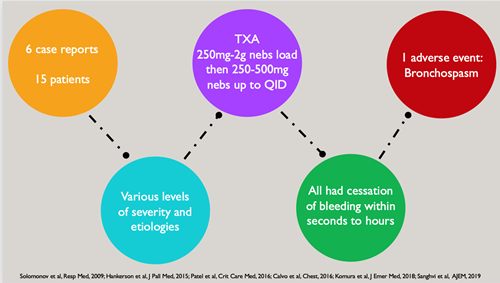
- Case Reports
- Most of the evidence to date on inhaled TXA for hemoptysis is based on case reports
- Since 2009, there have been 6 published case reports on 15 adult patients14-19
- Causes of hemoptysis varied but most often included cancer, bronchiectasis, or alveolar hemorrhage
- Doses ranged from an initial dose of 250-2000mg, potentially followed by repeat doses of 250-500mg every 6-8 hours
- Bleeding almost always stopped within minutes of administration
- Nebulized TXA was well tolerated, with only 1 adverse event reported (bronchospasm that resolved with bronchodilators)
- Cochrane Review (2016)11
-
- O’Neill et al (2020)20
- An observational trial in pediatric patients (N = 19, aged 5 months to 19 years)
- Dose: TXA 250-500mg nebulized q6-12h
- Cessation of bleeding in 95% cases, with a median time to cessation being 1 day
- Effective in all cases except one: a child who was anticoagulated with heparin and was on ECMO
- No adverse events
- Wand et al (2018)21
- RCT (N = 47) on adult patients with non-massive hemoptysis, comparing nebulized TXA to placebo
- Study Design:
- Intervention Arm: TXA 500mg nebs TID up to 5 days
- Control Arm: Matched placebo (Normal saline nebs)
- Outcomes:
- Primary outcome: Rate of completed resolution of hemoptysis within 5 days
- Secondary outcomes: Need for intervention (bronchoscopy, embolization, or surgical intervention), and adverse events, among others
- Results:
- Complete resolution of hemoptysis within 5 days (primary outcome): SIGNIFICANTLY INCREASED in TXA group (96% vs 50%, p < 0.0005, NNT =2)
- Need for procedural intervention: significantly decreased (0% vs 18.2%, p = 0.041, NNT = 5)
- No adverse events in either group
- Conclusion:
- Inhaled TXA can be safely and effectively used to control bleeding in patients with non-massive hemoptysis
- Limitations:
- Small sample size
- A treatment course of 5 days makes it less relevant to ED practice
- Excluded patients with hemodynamic compromise or massive hemoptysis
- O’Neill et al (2020)20
Expert Opinion
-
- Dr. Michael Hickey (MD, FRCPC, Emergency Physician & Intensivist, St. Joseph’s Health Centre, Toronto)
- There is very little downside, as long as it doesn’t delay resuscitation or other more important interventions
- Priorities remain lung isolation and definitive therapy
- TXA’s effectiveness will likely depend on the source of bleeding
- Dr. Madelein Warwick (MD, FRCPC, Respirology Fellow, Queen’s University, Kingston)
- “We use TXA regularly for hemoptysis while we’re figuring out further management”
- If moderate-to-massive hemoptysis –> TXA 1g IV
- If increased risk of thromboembolism –> TXA 500mg nebs
- Dr. Michael Hickey (MD, FRCPC, Emergency Physician & Intensivist, St. Joseph’s Health Centre, Toronto)
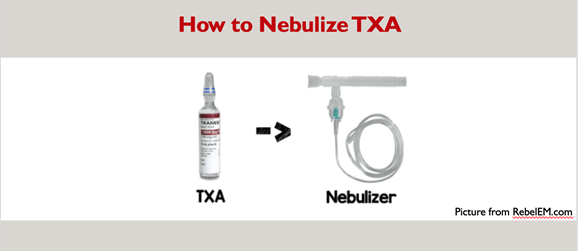
How To Nebulize TXA
-
- Ask for a 1g vial of TXA, pour half into the nebulizer and that’s it – easy peasy!
- You can consider adding 5-10cc of normal saline as well, but this is not necessary and may induce bronchospasm (I would advise against this)
Part III: TXA FAQ’s
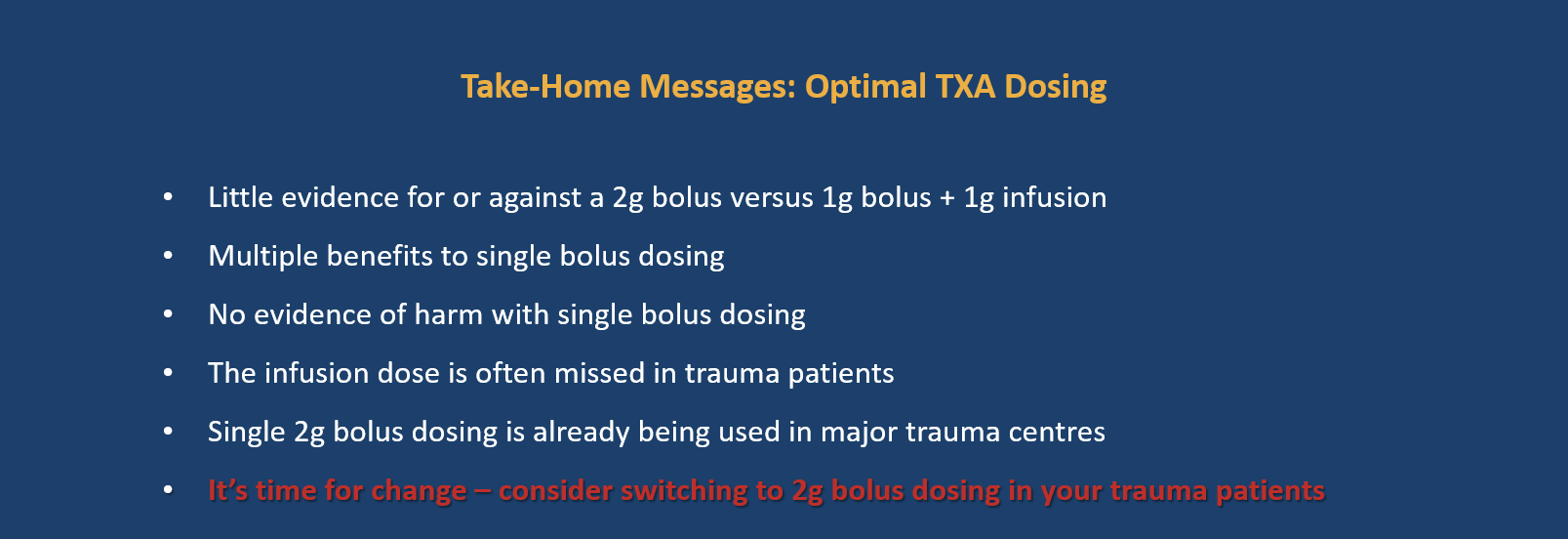
Optimal TXA Dosing: 2g Bolus upfront versus 1g Bolus + 1g Infusion
Emergency Situations
The optimal dosing for TXA use in emergency situations remains unclear.
-
- The CRASH-2 dosing1 (1g IV over 10 minutes, followed by 1g IV over 8 hours) appears to be the leading guide
- This dosing regimen was chosen as it has previously been shown to be effective at reducing fibrinolysis in cardiac surgery patients, and early administration was favored given that most trauma deaths due to bleeding occur on the day of the injury
- However, there is considerable practice variation in dosing regimens used, with some centers using a 2 g bolus up front instead of the 1g + 1g infusion… but is one way better than the other? Unfortunately, research is limited.
- The CRASH-2 dosing1 (1g IV over 10 minutes, followed by 1g IV over 8 hours) appears to be the leading guide
Pre-Hospital Evidence
-
- A study by Rowell et al (2020)6 as well as the STAAMP trial (Guyette et al, 202022), looked at the effect of a 2g bolus (with or without subsequent infusion) compared to the CRASH-2 dosing of 1g IV + 1g infusion
- Neither trial found a significant difference in functional outcomes or mortality in trauma patients between dosing regimens but also did not find any significant differences in adverse events.
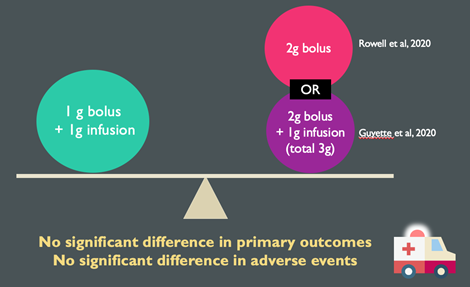
-
- As such, there is insufficient evidence to suggest that one dosing regimen is better than the other, however administering TXA as a single bolus does offer additional benefits:
- Frees up an IV line by removing the need to run an infusion for 8 hours
- Allows for mental offloading of the need for an infusion
- As such, there is insufficient evidence to suggest that one dosing regimen is better than the other, however administering TXA as a single bolus does offer additional benefits:
Support for 2g IV Bolus versus Bolus + Infusion Regimen
-
- 2020 TCCC Guideline Updates23
- Shifted to a 2g IV bolus instead of a 1 g bolus in military settings, in addition to including TBI as an indication for TXA use
- Practice at other major trauma sites
- Both St. Michael’s Hospital and Sunnybrook Health Sciences Centre have shifted to giving 2 grams upfront after realizing that the infusion dose was often being missed in their trauma patients
- Local data from The Ottawa Hospital (2014)24 also shows that the infusion dose is often missed in our trauma patients (only given within 3 hours in 18% of patients), and the most common deviation from the CRASH-2 protocol was found to be a failure of the administration of the second dose of TXA
- 2020 TCCC Guideline Updates23
Routes of Administration
-
- TXA has many routes of administration including intravenous, oral, topical, and nebulized
- But what about Intramuscular (IM) Use?
- Grassin-Delyle et al. (2020)25
- A prospective study (N = 30) looking a the pharmacokinetics of IM TXA in trauma patients
- Intervention: TXA 1g IM given 2 hours after an initial IV bolus
- Results:
- Therapeutic concentrations were achieved in as little as 15 minutes following IM administration of TXA
- No reported serious adverse events
- Conclusion:
- IM TXA is well tolerated and rapidly absorbed, reaching therapeutic concentrations within 15 mins
- But this is not enough evidence to support practice change (yet!)
- Grassin-Delyle et al. (2020)25
Clinical Considerations: Why is there so much variability in major TXA trial outcomes?
-
- Simple answer: Not all bleeding is the same!
- Dr. Kerstin de Wit (MD, MSc, FRCPC, Thrombosis & Emergency Medicine, McMaster University) provided insights into why she suspects we are seeing mixed results on the effectiveness of TXA in trauma and other forms of bleeding
- Many different factors affect bleeding itself, as well as the effect bleeding has on the patient
- eg. A small bleed into the spinal canal can have devastating consequences for patients, whereas a similar volume elsewhere may be of little consequence to the patient
- The dynamics of different types of bleeding have likely affected the results seen in different trials
- Traumatic bleeding is often fast onset and associated with very early healing
- Mucosal bleeding (seen in gastritis or epistaxis) is typically slower and more gradual
- The side effects of TXA and the effect of these on the patient may also play a role in the outcomes seen
- eg. The effect of hypotension is likely to be much more devastating in patients with a traumatic brain injury than it is in other conditions
- Many different factors affect bleeding itself, as well as the effect bleeding has on the patient
- Taken together, these factors help us understand the differences seen in the major TXA trials so far, and provide an outlet for further research.
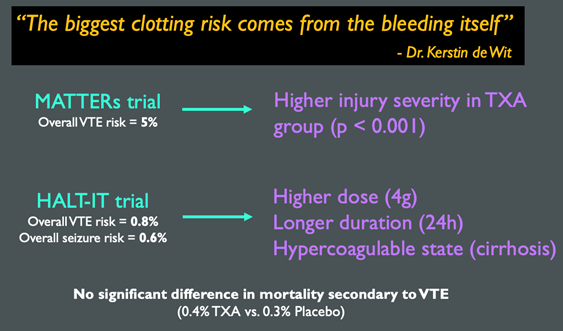
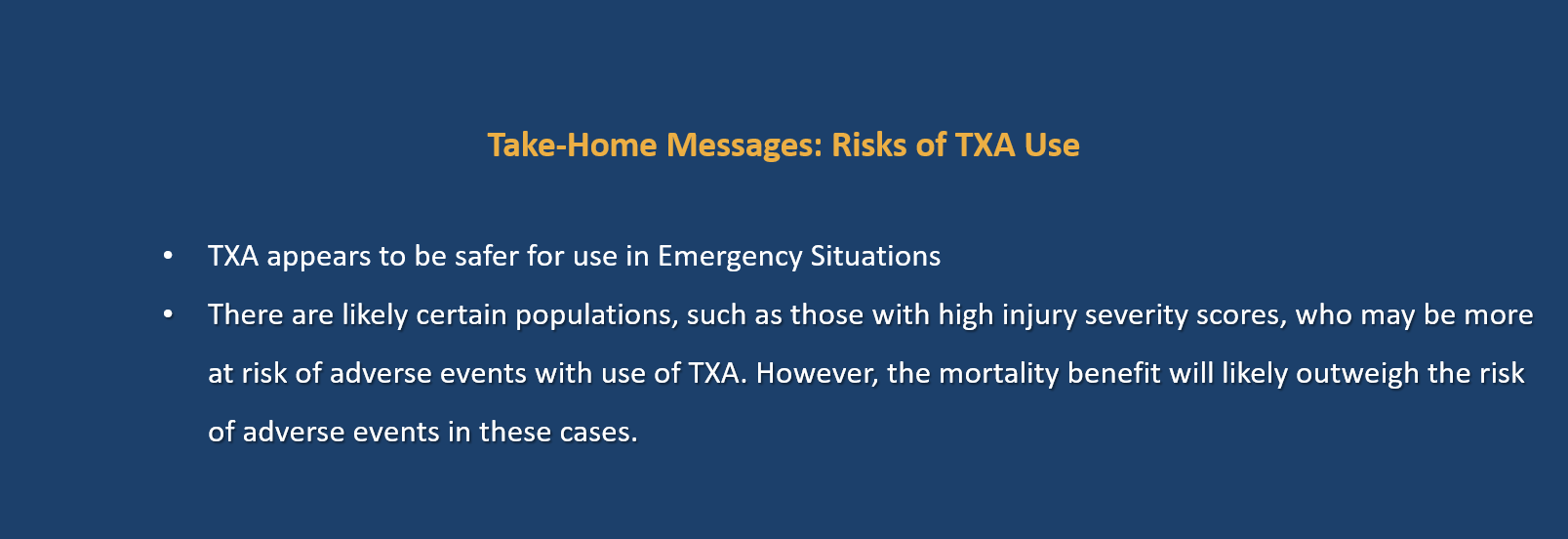
Risks of TXA Administration
-
- The most commonly studied adverse events are venous and arterial thromboembolism and seizures
- The literature on overall rates of adverse events is quite mixed, however, when considering data specific to its use in emergency situations, most trials have not shown significant differences in rates of VTE, arterial thromboembolism, or in seizures, with the exception of two studies, the MATTERs, and the HALT-IT trials, as shown here in this table:
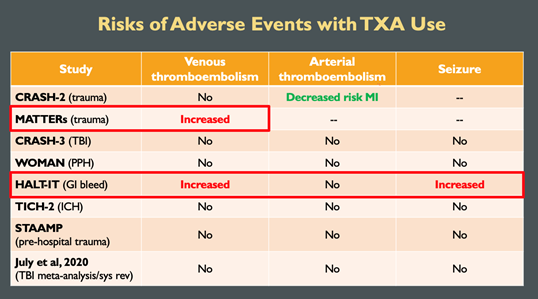
-
- Looking at these trials individually, we can speculate as to why there may have been increased rates of adverse events in these studies
- The MATTERs trial2 on trauma patients in military settings showed a significantly increased risk of VTE
- There was a higher degree of injury severity in the TXA group compared to the placebo group
- Higher injury severity is an independent risk factor for thrombosis
- As such, it’s not surprising that a higher rate of VTE was seen in this group of more severely injured patients
- The HALT-IT trial9 on GI bleeding showed an increased risk of VTE and seizures
- Their use of a higher dose of TXA for a longer period of time (4g IV over 24 hours) than has been used in other trials may have increased the risk of seizure and VTE, respectively
- Nearly half the participants had cirrhosis, increasing the likelihood that they were hypercoagulable at baseline which may have increased the rate of VTE in this study.
- The MATTERs trial2 on trauma patients in military settings showed a significantly increased risk of VTE
- Looking at these trials individually, we can speculate as to why there may have been increased rates of adverse events in these studies
Part IV: Take Home Messages
Dosing
-
- 2g IV bolus appears equally effective & safe
- May offer additional benefits
Routes of Administration
-
- IM TXA reaches therapeutic levels quickly
- Potential future modality – not yet ready for clinical use
Clinical Considerations
-
- Not all bleeding is the same
- The effectiveness of TXA will depend on multiple factors including the timing of administration, the type, size, and location of the bleed
Adverse Events
-
- Very good safety profile
- Increased risk VTE with high injury severity and GI bleeds
Overall Summary of Recommendations
References
- CRASH-2 Trial Collaborators. (2010). Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. The Lancet, 376(9734), 23–32. https://doi.org/10.1016/s0140-6736(10)60835-5
- Morrison, J. J., Dubose, J. J., Rasmussen, T. E., & Midwinter, M. J. (2012). Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) Study. Archives of Surgery, 147(2), 113. https://doi.org/10.1001/archsurg.2011.287
- July, J., & Pranata, R. (2020). Tranexamic acid is associated with reduced mortality, hemorrhagic expansion, and vascular occlusive events in traumatic brain injury – meta-analysis of randomized controlled trials. BMC Neurology, 20(1), 1–11. https://doi.org/10.1186/s12883-020-01694-4
- CRASH-3 Trial Collaborators. (2019). Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomised, placebo-controlled trial. The Lancet, 394(10210), 1713–1723. https://doi.org/10.1016/s0140-6736(19)32233-0
- Mahmood, A., Needham, K., Shakur-Still, H., Harris, T., Jamaluddin, S. F., Davies, D., Belli, A., Mohamed, F. L., Leech, C., Lotfi, H. M., Moss, P., Lecky, F., Hopkins, P., Wong, D., Boyle, A., Wilson, M., Darwent, M., & Roberts, I. (2020). Effect of tranexamic acid on intracranial haemorrhage and infarction in patients with traumatic brain injury: a pre-planned substudy in a sample of CRASH-3 trial patients. Emergency Medicine Journal, 0, 1–9. https://doi.org/10.1136/emermed-2020-210424
- Rowell, S. E., Meier, E. N., McKnight, B., Kannas, D., May, S., Sheehan, K., Bulger, E. M., Idris, A. H., Christenson, J., Morrison, L. J., Frascone, R. J., Bosarge, P. L., Colella, M. R., Johannigman, J., Cotton, B. A., Callum, J., McMullan, J., Dries, D. J., Tibbs, B., … Schreiber, M. A. (2020). Effect of Out-of-Hospital Tranexamic Acid vs Placebo on 6-Month Functional Neurologic Outcomes in Patients With Moderate or Severe Traumatic Brain Injury. JAMA, 324(10), 961–974. https://doi.org/10.1001/jama.2020.8958
- Bossers, S. M., Loer, S. A., Bloemers, F. W., Hartog, D. D., Van Lieshout, E. M. M., Hoogerwerf, N., van der Naalt, J., Absalom, A. R., Peerdeman, S. M., Schwarte, L. A., Boer, C., & Schober, P. (2020). Association Between Prehospital Tranexamic Acid Administration and Outcomes of Severe Traumatic Brain Injury. JAMA Neurology, E1–E8. https://doi.org/10.1001/jamaneurol.2020.4596
- Bennett, C., Klingenberg, S. L., Langholz, E., & Gluud, L. L. (2014). Tranexamic acid for upper gastrointestinal bleeding. Cochrane Database of Systematic Reviews, 1–33. https://doi.org/10.1002/14651858.cd006640.pub3
- HALT-IT Trial Collaborators. (2020). Effects of a high-dose 24-h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding (HALT-IT): an international randomized, double-blind, placebo-controlled trial. The Lancet, 395, 1927–1936. https://doi.org/10.1016/S0140-6736(20)30848-5
- Sprigg, N., Flaherty, K., Appleton, J. P., Salman, R. A.-S., Bereczki, D., Beridze, M., Christensen, H., Ciccone, A., Collins, R., Czlonkowska, A., Dineen, R. A., Duley, L., Egea-Guerrero, J. J., England, T. J., Krishnan, K., Laska, A. C., Law, Z. K., Ozturk, S., Pocock, S. J., … Bath, P. M. (2018). Tranexamic acid for hyperacute primary IntraCerebral Haemorrhage (TICH-2): an international randomised, placebo-controlled, phase 3 superiority trial. The Lancet, 391(10135), 2107–2115. https://doi.org/10.1016/s0140-6736(18)31033-x
- Prutsky, G., Domecq, J. P., Salazar, C. A., & Accinelli, R. (2016). Antifibrinolytic therapy to reduce haemoptysis from any cause. Cochrane Database of Systematic Reviews, 1–12. https://doi.org/10.1002/14651858.cd008711.pub3.
- Ruiz W. 1994. Acido tranexamico vs placebo en hemoptisis por TBC pulmonar: estudio pilato doble ciego. Thesis.
- Tscheikuna, J., Chvaychoo, B., Naruman, C., & Maranetra, N. (2002). Tranexamic acid in patients with hemoptysis. J Med Assoc, 85(4):399-404.
- Solomonov, A., Fruchter, O., Zuckerman, T., Brenner, B., & Yigla, M. (2009). Pulmonary hemorrhage: A novel mode of therapy. Respiratory Medicine, 103(8), 1196–1200. https://doi.org/10.1016/j.rmed.2009.02.004
- Hankerson, M. J., Raffetto, B., Mallon, W. K., & Shoenberger, J. M. (2015). Nebulized Tranexamic Acid as a Noninvasive Therapy for Cancer-Related Hemoptysis. Journal of Palliative Medicine, 18(12), 1060–1062. https://doi.org/10.1089/jpm.2015.0167
- Patel, M., Abbas, F., & Sheppard, T. (2016). 1887: HEMOPTYSIS CONTROLLED WITH THE USE OF INHALED TRANEXAMIC ACID: A CASE SERIES. Critical Care Medicine, 44(12), 547. https://doi.org/10.1097/01.ccm.0000510560.32498.25
- Segrelles Calvo, G., De Granda-Orive, I., & López Padilla, D. (2016). Inhaled Tranexamic Acid as an Alternative for Hemoptysis Treatment. Chest, 149(2), 604. https://doi.org/10.1016/j.chest.2015.10.016
- Komura, S., Rodriguez, R. M., & Peabody, C. R. (2018). Hemoptysis? Try Inhaled Tranexamic Acid. The Journal of Emergency Medicine, 54(5), e97–e99. https://doi.org/10.1016/j.jemermed.2018.01.029
- Sanghvi, S., Van Tuyl, A., Greenstein, J., & Hahn, B. (2019). Tranexamic acid for treatment of pulmonary hemorrhage after tissue plasminogen activator administration for intubated patient. The American Journal of Emergency Medicine, 37(8), 1602.e5-1602.e6. https://doi.org/10.1016/j.ajem.2019.05.024
- O’Neil, E. R., Schmees, L. R., Resendiz, K., Justino, H., & Anders, M. M. (2020). Inhaled Tranexamic Acid As a Novel Treatment for Pulmonary Hemorrhage in Critically Ill Pediatric Patients. Critical Care Explorations, 2(1), e0075. https://doi.org/10.1097/cce.0000000000000075
- Wand, O., Guber, E., Guber, A., Epstein Shochet, G., Israeli-Shani, L., & Shitrit, D. (2018). Inhaled Tranexamic Acid for Hemoptysis Treatment. Chest, 154(6), 1379–1384. https://doi.org/10.1016/j.chest.2018.09.026
- Guyette, F. X., Brown, J. B., Zenati, M. S., Early-Young, B. J., Adams, P. W., Eastridge, B. J., Nirula, R., Vercruysse, G. A., O’Keeffe, T., Joseph, B., Alarcon, L. H., Callaway, C. W., Zuckerbraun, B. S., Neal, M. D., Forsythe, R. M., Rosengart, M. R., Billiar, T. R., Yealy, D. M., Peitzman, A. B., & Sperry, J. L. (2020). Tranexamic Acid During Prehospital Transport in Patients at Risk for Hemorrhage After Injury. JAMA Surgery, E1–E10. https://doi.org/10.1001/jamasurg.2020.4350
- Drew, B., Auten, J., Cap, A., Deaton, T., Donham, B., Dorlac, W., DuBose, J., Fisher, A. D., Ginn, A. J., Hancock, J., Holcomb, J. B., Knight, J., Knight, R., Koerner, A., Littlejohn, L., Martin, M. J., Morey, J., Morrison, J., Schreiber, M., … Butler, F. (2020). The Use of Tranexamic Acid in tactical combat casualty care. Journal of Special Operations Medicine, 20(3), 36–43. https://doi.org/10.0000/0000
- Yelle, K., Woo, M.Y., Saidenberg, E., Lampron, J. (2020). The Use of Tranexamic Acid in Trauma Patients- a Retrospective Review, unpublished manuscript, The University of Ottawa.
- Grassin-Delyle, S., Shakur-Still, H., Picetti, R., Frimley, L., Jarman, H., Davenport, R., McGuinness, W., Moss, P., Pott, J., Tai, N., Lamy, E., Urien, S., Prowse, D., Thayne, A., Gilliam, C., Pynn, H., & Roberts, I. (2021). Pharmacokinetics of intramuscular tranexamic acid in bleeding trauma patients: a clinical trial. British Journal of Anaesthesia, 126(1), 201–209. https://doi.org/10.1016/j.bja.2020.07.058





great job. Thank you so much
Very well done article. Congrats!
Excellent review! Much Appreciated – keep up the great work!