Shoulder dislocations are the most common large joint dislocation encountered by emergency physicians. Given their incidence in the emergency department, managing shoulder dislocations efficiently is key to departmental flow.`
Recently, Dowson et al.1 utilized a specific shoulder reduction bench as a means to improve flow and reduce the need for procedural sedation. The results of this work were quite striking; this simple protocol reduced the average length of stay by 52 minutes, and the need for procedural sedation decreased from 57% to 18%.
Even without specialized gear, there are ways to improve efficiency when it comes to shoulder dislocations. This post aims to tackle the following common questions to improve departmental flow while ensuring quality and safe patient care:
Do I need pre-reduction imaging?
Is POCUS helpful in diagnosing shoulder dislocations?
What are the alternatives to procedural sedation?
What method is best at reducing shoulder dislocations?
This post will touch on these three questions as well as contraindications, post-reduction follow up care and and the dreaded posterior dislocations.
Do I need pre-reduction imaging?
What are the downsides to pre-reduction imaging?
- Associated with a 30 minute increase in ED department length of stay2
- Delays in reduction can lead to increased risk of reduction failure3
The concern about forgoing pre-reduction imaging is that the clinician might miss a fracture. However,:
- Orloski et al4 demonstrated that fractures are uncommon in patients under the age of 30
- Hendey5 demonstrated that fractures are rare in non-traumatic mechanisms.
These criteria can be combined in the Frenso-Quebec rule6 (not yet been prospectively validated, but was recently retrospectively validated7):
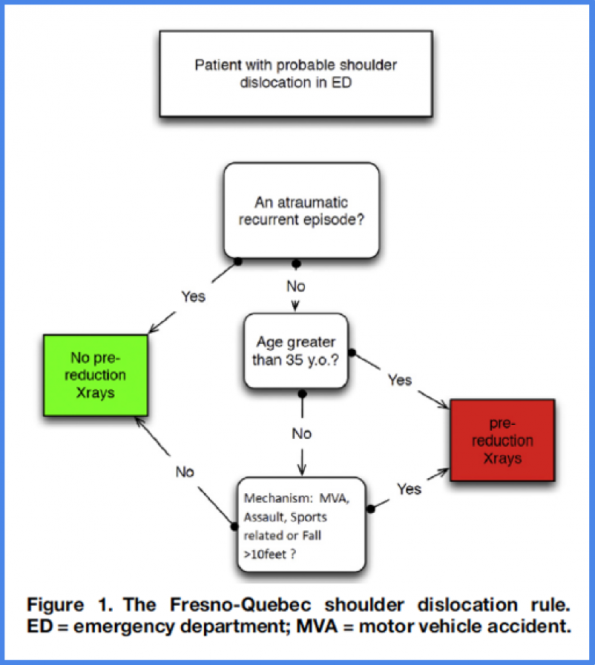
Figure from: Emond et al, 2018
Take home point #1: Pre-reduction films are not required in all cases. In particular for recurrent presentations, and young patients with atraumatic mechanisms. Consider utilization of the Fresno-Quebec rule to help guide decision making.
Is PoCUS useful in diagnosing shoulder dislocations?
The most common approach to ultrasound the glenohumeral joint is to use the curvilinear probe placed in the posterior aspect of the shoulder in the transverse orientation.
In a non-displaced shoulder, the humeral head can readily be seen articulating with the glenoid, the scapula medially, and infraspinatus above as the patient internally and externally rotates their arm. In the setting of a shoulder dislocation, this clear articulation would be lost.

Gottlieb et al.8 published a systematic review comparing the diagnostic accuracy of ultrasound with plain radiography in the assessment of shoulder dislocations. They found that ultrasound was 99.1% sensitive, and 99.9% specific for the diagnosis of shoulder dislocation
However, Secko et al.9 also examined the utility of ultrasound for dislocation diagnosis. Amongst their cohort of 65 patients, there were 25 total fractures, and 48% were not identified by ultrasound. Additionally, one of the misses was a surgical neck fracture, which is one of the major contraindications to attempted shoulder reduction in the emergency department.
Take home point #2: Ultrasound is likely not required in most cases. It can, however, assist in the confirmation of reduction in difficult cases when you’re not sure if your reduction was successful. The downside to ultrasound is that it may miss fractures, and therefore likely does not replace the need for pre-reduction imaging when indicated, or standard post-reduction imaging.
What are the alternatives to procedural sedation?
Within the literature there are three forms of regional anesthesia cited as alternatives to traditional procedural anesthesia for shoulder dislocations:
- Intra-articular lidocaine,
- Suprascapular nerve block
- Interscalene block.
We will focus our attention to intra-articular lidocaine and the suprascapular nerve block, and defer discussion of the interscalene block. In discussion with local expertise, the interscalene block was felt to be an unnecessarily complicated and higher risk block, and no more effective than the alternatives available.
Intra-articular lidocaine (IAL)
Method:
- A sterile technique is utilized and performed under ultrasound guidance, with a spinal needle aimed toward the joint space. Approximately 15-20 cc of 1% lidocaine is typically injected.
Evidence:
- In 2014, the journal of clinical anesthesia Jiang and colleagues published a systematic review comparing intravenous analgesia and sedation to intra-articular lidocaine.10 They were able to include 438 patients from 9 studies with varied methods of sedation, and reduction technique.
- No significant difference in joint reduction success was found.
- Additionally, sedation was associated with more adverse outcomes such as respiratory depression, vomiting, and thrombophlebitis.
- A previous Cochrane review from 2011, also found similar results.11
- These research findings suggest that IAL is an effective form of regional anesthesia.
Suprascapular nerve block (SNB):
The target of a SNB is the suprascapular nerve, which is a mixed (sensory and motor) nerve originating from the superior trunk of the brachial plexus (C5 and C6 nerve roots). It passes through the suprascapular notch, where it can be visualized with ultrasound.
Method:
- Using ultrasound, the suprascapular notch (primary target), is located, as well as the overlying transverse scapular ligament (TSL), which is hyperechoic
- The suprascapular nerve is located just beneath the TSL
- A spinal needle is introduced and dipped just below the transverse scapular ligament to bathe the nerve with approximately 5cc of 1% lidocaine

Landmarking
Visualization of the suprascapular notch with overlying suprascapular ligament
Evidence:
- The literature surrounding this technique is far sparser than that of IAL, primarily consisting of case reports.
- In 2014 Tezel et al. published a paper in the American Journal of Emergency Medicine comparing the suprascapular nerve block to procedural sedation.12
- This prospective trial randomized 41 patients to receive either IV Ketamine or a suprascapular nerve block to facilitate their shoulder reduction using the modified Kocher technique.
- No significant difference was noted in the groups in terms of reduction success.
- All patients were successfully reduced.
- ED length of stay was longer in the sedation group.
- These findings suggest that the SNB is an effective form of regional anesthesia.
Take home point #3: IAL and the SNB are both effective forms of regional anesthesia and can be considered as an alternative to procedural sedation for shoulder reductions.
Closed reduction
Contraindications:
Before proceeding with any procedure, it’s important to consider contraindications to reduction.
The first absolute contraindication:
- Delayed presentation in the elderly, ie. Any dislocation that has been present for a week or longer.
- These patients have much higher incidence of vascular injury and fracture associated with reduction attempt
- These patients warrant an orthopaedics consultation in the emergency department.
The second absolute contraindication:
- Fracture of the humeral neck.
- The photo below highlights why this is a contraindication.
- In this case following attempted reduction, the patient will essentially have a 100% chance of developing avascular necrosis of the humeral head

The top represents a subtle humeral neck fracture, with the bottom photo being post-reduction. Note the complete separation of the proximal portion of the humeral head from the distal segment.

What method is best at reducing shoulder dislocations?
There are dozens of maneuvers, and frankly it can be a bit overwhelming. We’ll start by eliminating two maneuvers from our arsenal as they have been associated with increased harm.
The first is the Hippocratic method:
- A foot is placed in the axilla,
- traction placed on the abducted arm.
- This has been linked to cases of brachial plexus and axillary vessel injury, and such is best avoided.13
The Second is the popular Kocher method:
- Vertical traction and external rotation of the arm
- This method has been present and in use since 1870.
- There have been case reports of humeral shaft fractures, axillary vein rupture, rotator cuff, and pectoralis muscle rupture.13
- Given this rare potential for harm, defer this technique given the multitude of other techniques available.
So, which maneuver is best?
- In 2021, Dong et al. published a systematic review attempting to answer the question of which method of reduction technique was the best.14
- They elected to group the various techniques into categories of traction based techniques, leverage based techniques, and scapular manipulation.
- They included 12 RCTs with over 1000 patients.
- Unfortunately, they did not find any significant difference in success of reduction, and their results were limited by a small number of low quality trials.
- Traction techniques were however noted to be associated with less pain, which makes sense intuitively as the application of force may relieve pressure on an impacted humeral head.
Knowing that there is no optimal method of reduction, there is merit recommend starting with one of the maneuvers that has been associated with decreased need for procedural sedation such as:
- Davos or Boss-Holzach-Matter Method15
- FARES method16
- scapular manipulation17
For the difficult reduction requiring sedation, consider starting with a series of leverage based techniques:
- External rotation, into a Milch maneuver, with subsequent addition of an anterior directed force on the humeral head (attempting to lift it around the glenoid into the joint space).
- If still unsuccessful, make sure that your patient’s sedation and analgesia are optimized. Then, consider switching from these leverage based techniques to a traction based method such as traction-counter-traction.
If no success at this point, (which should be exceedingly rare), it would be time to call orthopaedics for consultation, and consideration for OR reduction.
Take home point #4: The optimal method of reduction is unknown. Remember contraindications, and arm yourself with a toolbox of maneuvers that can be applied at the bedside without procedural sedation. And then have a sequential and step wise approach for the patient that does require sedation.
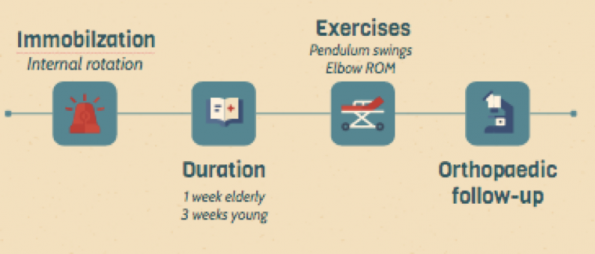
Post-reduction follow-up care
The following post-reduction care is required after successful reduction of an anterior dislocation:
- Immobilize in internal rotation
- 3 weeks in younger patients
- 1 week in the elderly. Longer durations of immobilization in older patients are associated with increased risk of adhesive capsulitis.
- Patients should be advised to avoid any overhead lifting.
- They should be advised to perform gentle shoulder pendulum exercises each day, as well as elbow ROM exercises to prevent concomitant elbow stiffness.
- Orthopaedics follow-up recommended.
Posterior shoulder dislocations
For the last portion of this post, we will briefly discuss posterior dislocations. Epidemiological data published in 2013 looking at over 20000 shoulder dislocations presentations in Ontario, demonstrated that posterior dislocations represent approximately 2% of all dislocations.18 Classically they are found to be associated with the 3 E’s:
- Epilepsy
- Electricity
- Ethanol
Posterior dislocations are commonly missed, with wide varying ranges quoted in the literature with some quoting the miss rate to be as high as 80% on initial presentation.
Additionally, the commonly taught radiographic findings are difficult to interpret, and are often missed. These include:
- The lightbulb sign,
- Widening of the glenohumeral joint,
- Trough line sign.
They were once quoted as a diagnostic trap by orthopaedic surgeon Harrison McLaughlin in 1954,19 and this remains so today.
In an attempt to provide better insight into the neglected posterior dislocation. Xu et al. published a systematic review of the literature surrounding the diagnosis of posterior dislocations.20
- They identified 53 articles consisting mainly of case reports and case series, that included 242 shoulder dislocations amongst 205 patients.
- They found that only 11.4% of cases had a correct diagnosis on initial assessment
- However, in 36 cases where an AP view was combined with an axillary or Y-view or CT, diagnosis was made correct and timely in 100% of cases.
- In going through these individual cases, it was truly the addition of the axillary view that corresponded to the bulk of this result.
- The utility of the axillary view is highlighted below:



Posteriorly dislocated shoulder. Note how the axillary view on the top provides the greatest diagnostic utility.
Take home point #5: Posterior shoulder dislocations are commonly missed. Common x-ray findings are insensitive for the diagnosis, and will lead to continued routine misses if relied upon.The axillary view is your best defence against missing this uncommon diagnosis.
References
- Dowson P. (2019). Shoulder Reduction Bench Project: improving care for patients with shoulder dislocations BMJ Open Quality; 8:e000366. doi: 10.1136/bmjoq-2018-000366
- Shuster M, Abu-Laban R, Boyd J, Gauthier C, Shepherd L, Turner C. (2002). Prospective evaluation of a guideline for the selective elimination of pre-reduction radiographs in clinically obvious anterior shoulder dislocation. Canadian Journal of Emergency Medicine, 4(4), 257-262. doi:10.1017/S148180350000748X
- Kanji A, Atkinson PR, Fraser J, Lewis DA, Benjamin S. (2015). Delays to initial reduction attempt are associated with higher failure rates in anterior shoulder dislocation: a retrospective analysis of factors affecting reduction failure. Emergency Medicine Journal, 33, 130 – 133.
- Orloski J, Eskin B, Allegra PC. (2011). Do all patients with shoulder dislocations need prereduction x-rays? Am J Emerg Med; 29:609–612. doi: 10.1016/j.ajem.2010.01.005.
- Hendey GW. (2000). Necessity of Radiographs in the emergency department management of shoulder dislocation. Annals of Emergency Medicine, 36;2:108-113.
- Emond M, Gariepy C, Boucher V, Hendey GW. (2018). Selective Prereduction Radiography in Anterior Shoulder Dislocation: The Fresno-Quebec Rule. J Emerg Med, 55:218−25.
- Durak VA, Atıcı T. (2021). Diagnostic accuracy of Fresno-Quebec Rules and risk factors for an associated fracture in patients presenting to the emergency department with anterior shoulder dislocation: A retrospective study. Ulus Travma Acil Cerrahi Derg, Jan;27(1):115-121. English. doi: 10.14744/tjtes.2020.29402. PMID: 33394468.
- Gottlieb M, Holladay D, Peksa GD. (2019). Point‐of‐care ultrasound for the diagnosis of shoulder dislocation: A systematic review and meta‐analysis. American Journal of Emergency Medicine, 37, 757–761.
- Secko MA, Reardon L, Gottlieb M, et al. (2020). Musculoskeletal ultrasonography to diagnose dislocated shoulders: a prospective cohort. Ann Emerg Med, S0196-0644(20)30008-1.
- Jiang N, Hu YJ, Zhang KR, Zhang S, Bin Y. (2014). Intra-articular lidocaine versus intravenous analgesia and sedation for manual closed reduction of acute anterior shoulder dislocation: an updated meta-analysis. J Clin Anesth. 26(5): 350-9.
- Wakai A, O’Sullivan R, McCabe A. (2011). Intra‐articular lignocaine versus intravenous analgesia with or without sedation for manual reduction of acute anterior shoulder dislocation in adults. Cochrane Database of Systematic Reviews. Issue 4. Art. No.: CD004919. DOI: 10.1002/14651858.CD004919.pub2.
- Tezel O, Kaldirim U, Bilgic S, Deniz S, Eyi YE, Ozyurek S, Durusu M, Tezel N. (2014). A comparison of suprascapular nerve block and procedural sedation analgesia in shoulder dislocation reduction. Am J Emerg Med. 32(6):549- 52.
- Dala-Ali B, Penna M, McConnell J, Vanhegan I, Cobiella C, (2014). Management of Acute Anterior Shoulder Dislocation. British Journal of Sports Medicine, vol. 48, no. 16, pp. 1209–15. PubMed, doi:10.1136/bjsports-2012-091300.
- Dong H, Jenner EA, Theivendran K. (2021) Closed reduction techniques for acute anterior shoulder dislocation: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 47:407.
- Stafylakis D, Abrassart S, Hoffmeyer P. (2016) Reducing a Shoulder Dislocation Without Sweating. The Davos Technique and its Results. Evaluation of a Nontraumatic, Safe, and Simple Technique for Reducing Anterior Shoulder Dislocations. J Emerg Med. 50:656.
- Sayegh FE, Kenanidis EI, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kapetanos GA. (2009) Reduction of acute anterior dislocations: a prospective randomized study comparing a new technique with the Hippocratic and Kocher methods. J Bone Joint Surg Am. 91(12):2775-82.
- Pishbin E, Bolvardi E, Ahmadi K. (2011). Scapular manipulation for reduction of anterior shoulder dislocation without analgesia: results of a prospective study. Emerg Med Australas. 23: 54-58.
- Leroux T, Wasserstein D, Veillette C, et al. (2014). Epidemiology of Primary Anterior Shoulder Dislocation Requiring Closed Reduction in Ontario, Canada. The American Journal of Sports Medicine. 42(2):442-450.
- McLaughlin HL. (1952). Posterior dislocation of the shoulder. J Bone Jt Surg Am. 24:584e90.
- Xu W, Huang L-X, Guo JJ, et al. (2015). Neglected posterior dislocation of the shoulder: A systematic literature review. J Orthop Translat. 3(2):89–94.



“Such a great blog! Thank you for this information, I appreciate your effort, please keep us update.
I am looking for these kinds of blogs for last many days. Thanks for sharing it with us”
Excellent Article, Excellent Blog , Excellent Site ✅✅✅