We know that Physician burnout rates through the pandemic are escalating from already alarming numbers, prompting increased focus on personal wellness. But, at the same time its hard to feel the strain of the healthcare system.
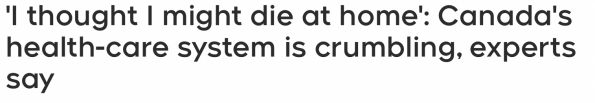
Headlines like this make the notion of wellness quite challenging, and amplifying this are concerns amongst healthcare providers, media and patients that the healthcare system is struggling to meet the needs of our patients.
When healthcare administration talks about addressing burnout, we know that wellness concepts are going to talk about resiliency. The problem is, this that this comes across disingenuously – when there are valid concerns that the healthcare system is far less resilient than the providers holding it up.
But I don’t think that is the appropriate lens to view our ‘resiliency’ through, because the reality is, the system doesn’t care if you are burnt out.
Its not that the people in the system don’t care about your wellness (that may not be entirely true) but its that the vehicle that is the healthcare system doesn’t care about it. We are all but single cogs in this giant machine that is struggling. Sure, outside of your work you can sit on committees, working groups, and have academic roles to improve the system. But when you’re at work all you can control is a very limited set of variables.
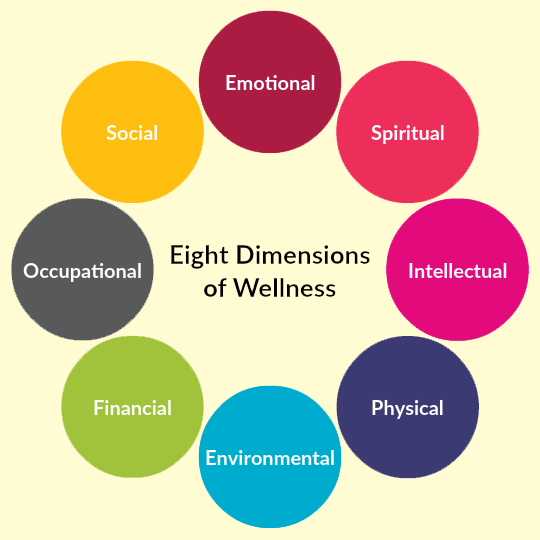
Within the wellness domains, most people are probably pretty good at maintaining a healthy balance through most of these.
The biggest problem is occupational wellness, and it’s because we lack control within that domain. When I show up to work and there are 50 people in the waiting room with 8-hour wait times, I can’t control the circumstances that lead to be working in that environment. While I can chose to be upset about it, or angry at the system, I can’t change it. That’s really challenging. But, I never want a job to make me feel miserable, so how I think about my job centres around the variables that I can control.
And for me, that became resiliency.
It took me a while to gain this perspective, but when I did I decided that I would explore more wellness concepts to integrate into my work and life to see if I could improve my occupational wellness. I’ll confess, I was quite skeptical going in, because I had come from the mindset that doctors are resilient, resiliency means just continuing to jump through hoops that you’re supposed to, and wellness concepts were fluffy.
I was wrong.
This series of posts looks to address the morale distress, injury and burnout we incur as a result of our occupation, and how we can use personal agency to minimize the effect and internalization that has upon us, to improve our occupational wellness at home and work.
Disclaimer
These series requires three very important disclaimers:
- This is my take (with some guest input), from skeptic to believer. Not everything in the posts will resonate with you, everyone has to find the tools that work best for them.
- There is a proportion of healthcare providers (roughly 15%) for whom wellness content will not be especially useful. This is because the morale distress that we often feel, compounded overtime can result in significant morale injury – and subsequently PTSD around ones work. We know that negative physiologic responses to our work are rooted in having some PTSD; and a mandatory wellness module, pizza party of meditation session isn’t going to help that. For some people – wellness is no longer in their hands, and their burnout is something that only true therapy (and likely trauma counselling) can help address. (For more on PTSD in healthcare, check out this great post).
- The second disclaimer is that wellness isn’t all sunshine and rainbows. Wellness is not about every day being great; it is about being yourself. It is having the ability to show up with enough gas in your tank to do the things you need to do. A great secondary outcome of focusing on wellness is loving your job, but the primary outcome is to develop an approach to at least not have negative physiologic feelings toward your work.
We’re not Alone
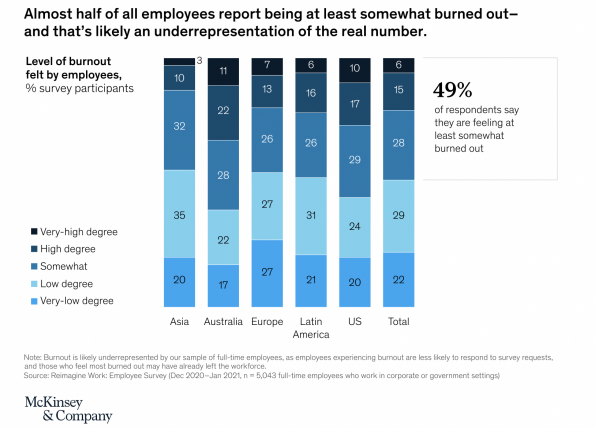
Escalating burnout rates are not isolated to medicine, and the pandemic is really highlighted this across a lot of different industries.
This idea that we are not alone is important, because people who feel that they are unique in their experiences suffer from morale injury to a greater extent. There is an idea of ‘living for the weekend’ exists for many people; that occupational wellness is challenging, and a want to refill our ‘cups’ away from work.
The problem with this is, that we spend so much time at work, and when your occupational wellness is so challenging, it can take away too much of our energy.
It doesn’t matter if you’re resilient
There is a perception that physicians are resilient. That just because we went through years of school and training that we have the ability to do hard things. But the mere ability to do hard things by no means makes us resilient. There is often this navy seal mentality in medicine, that one should just keep doing hard things and get up when you get knocked down. It took a lot of insight and recognition to realize that I was naive in thinking that was all there was to resiliency.
The Wellness Battery
Too often, we go on vacation, fully charge our batteries, and feel great coming back home – and then we work 2-3 shifts, and our battery is completely drained again. Which begs the question, how can we maintain a semblance of charge when our occupational wellness is so draining?
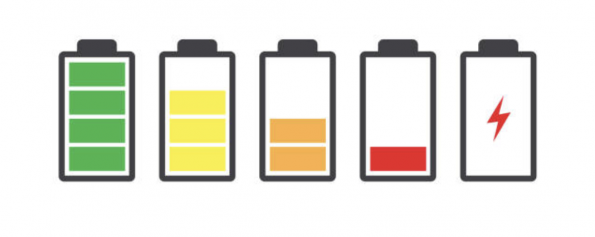
I’m not sure I have any more significant emotional complexity than my iPhone; and I have to be cognizant to charge it once or twice a day to make it though the end of the day without a dead battery. I’ve come to recognize that I am no different – while one can charge their batteries through various wellness domains, this is pointless of our occupational wellness is too critically draining. So it requires a renewed focus and emphasis on finding ways to optimize one’s own occupational wellness. You can call the drained battery whatever you want; burnout, energy levels, empathy fatigue, but personal wellness needs to centre around not completely draining your battery.
The Physiologic Argument for Wellness
Admittedly, starting my wellness journey, I was quite skeptical. But it was ultimately the physiologic argument for wellness that caught my attention.
Our days are constantly full of macro and micro-stressors. Consider the loss of a loved one as a macro-stressor, while many of our daily interactions cause micro-stressors. We are constantly inundated with micro-stressors in our day-to-day lives, from the moment we get out of bed and look at our phones, or the news – to our interpersonal interactions throughout the day.
The problem is that our natural evolutionary response to stress is the activation of our fight or flight response. This response was paramount for our species to ensure survival – from 5000 years ago when we had to run away from bears and lions, to even 100 years ago during world war one and the great depression. Nowadays, for most people, we are able to achieve the basic needs of survival, and yet our fight or flight response still exists in its purest form, and as a result we are often mounting a significant adrenal response to routine daily stressors.
Imagine a challenging day:
- Rushed morning
- Can’t find parking at the hospital
- Working with multiple junior learners
- Receive many handovers
- Day full of complex patients
- There are no beds to see patients in
- Dont get a chance to eat lunch
- Get yelled at by patients
- Receive patient complaint
- Leave your shift two hours late
It is hard for us to feel physiologically well if every shift we feel like we’re fighting a bear. If you allow yourself to feel this physiologic stress each day, of course occupational wellness is going to become a significant challenge, and chronically this will lead to some element of burnout.
Morale Distress
Morale distress is finely intertwined within healthcare; ethical questions, distressing medical cases, an acknowledgement of the struggles of the system and the (in)ability to provide care. Every day we will do something challenging or difficult; it may not be every case, but every day will have some challenges in it. This is inevitable – but you get to decide how that impacts you. There is an idea that you should enjoy 100% of your job, but that’s not realistic; sometimes your day sucks. People may often feel like if their day at work wasn’t perfect, that it was bad, and that is a dangerous dichotomy to reflect in such a binary way.
Because morale distress is an inevitable component of medicine, it is important to recognize that without appropriate repair, recovery and reflection that morale distress leads to morale injury, that cannot be fixed without professional help. This is because one begins to internalize that morale distress into a reflection of their morale fibre. Wellness ideas aren’t necessarily super positive of fluffy, but an acknowledgement of how one gets back to a healthy baseline.
Burnout
By now you have some sense of what burnout means to you, or you may have read conventional definitions as medicine begins to highlight this more frequently. Ultimately, burnout is an umbrella term for a spectrum of feelings that popped have – and those feelings can lead to a sense of resentment towards one’s job.
The basic framework for this is that medicine causes distress, and this can lead to a pathological internalization of oneself; “why do I even bother”, “why do I even do this?”. This causes an erosion of one’s sense of self because of an inability to frame things in a healthy way, and if this happens too much and you can’t replenish your feelings with other wellness domains, you’re going to struggle. The idea of ‘living for the weekend’ is ubiquitous across all professions and industry, and so it is not surprising that the pandemic has highlighted that across most professions, rates of burnout are going up.
The Problem with Personal Resiliency
Well-meaning wellness teachings or agendas will often expunge the importance of personal resiliency. For many in healthcare, this feels like a slap in the face. That we’re supposed to be resilient in the face of a crumbling system, leading some to suggest the system is not as resilient as its doctors, and telling us to be more resilient isn’t helpful. Now, while it may be hard to focus on personal resiliency in a system that is crumbling, we need to once again remember that the system doesn’t care if you are burnt out. The system doesn’t care about your wellness, only you do.
On airplanes; we are told to fix our own oxygen mask before helping others, when it comes to wellness and personal resiliency, the same holds true – because if we are unwell, how can we help others.
Being resilient is not about adopting a navy seal mindset and just being tough – it is about understanding what is within your control, and that is your reaction to situational stressors.
Personal Agency
Personal agency is the idea that “I am the one who is causing or generating an action, and that I am going to determine how things beyond my control affect me”.
When I walk into that department, and there are 50 patients waiting to be seen, with 8 hour wait times – I cannot change my circumstances. That department is what it is, but I get to decide how that environment is going to affect me.
Recently, we started to see more pediatric cases at work because of how busy pediatric hospitals have become during this flu season. One could bemoan the fact that we’re now seeing a new population; but instead of revealing in the negative, I used this as an opportunity to brush up on some pediatric CME, and embrace a skill that I often enjoy (seeing kids) and a novel challenge. So when kids starting showing up in the ED – I was happy to be able to provide care, rather than focusing on the negative, all because of perception around a variable that I had no control over anyways.
Every day can become a problem if you let it
This idea of personal agency becomes so important because otherwise every day can become a big problem. I know many colleagues who pathologize their shifts (and some of that may be PTSD); “what a crazy shift, woe is me”. Personally, I don’t think that is particularly healthy because I like to engage with the notion that I am unwilling to let a job make me feel miserable.
While morbid, I often give residents the example that if I were hit by a bus today (while that would be sad) – my shifts would be covered instantly by the group. Individually, we are all that replaceable, but, I am not that replaceable at home to my family. So, I refuse to let what is ultimately just a job distract from my wellness or make me feel miserable.
Because it IS just a job, medicine is what I do, it is not who I am
When medicine is closely linked to your identity it can start to erode you and your sense of self. We often think of morale distress occurring in the context of our patient experiences, but more often than not it has more to do with our interpersonal relationships and interactions within the healthcare system. In the past month, have you heard any of these?
Can you hold them overnight and see if they can walk in the morning?
What is your clinical question?
We wouldn’t admit this patient, try another service
Oh, they’re not direct to service, Emerg should see them first
In your attempts to advocate for a patient you encounter a seemingly endless barrage of pushback. You think that something needs to happen for a patient, and a consultant disagrees – then you have distress around the idea that maybe you’re wrong.
Maybe this elderly patient from home, who can’t ambulate, has no food in his fridge, rats in his apartment, and was covered in feces on arrival can go home after a physiotherapy consultation in the ED, just because their medical workup is normal.
Then you go home, and you feel like your job is awful, and you accomplished nothing to help this person. If this happens enough without appropriate reflection, recovery or renewal of your sense of self, then the next time it happens you’ll think “why does it matter” or “why should I care”, and that is a slippery slope. This is when you start to question your internal sense of self, and you feel rudderless – so there needs to be some internal recognition of what is a system issue, and what you can control.
Don’t stress about things you can’t control
Easy to say, but hard to do. But this is one of the most important concepts we need to cement into our minds as it pertains to our occupational stressors. Sure, you can sit on committees and working groups to advocate for change to the better within our system, but any given shift or day at work you have no control over any of that. On any given day we are all but single cogs in this medical machine, and only have control over a limited set of variables.
When we come back to this challenging day, we need to re-frame this in a way that highlights what we have control over:
- Rushed morning
Can’t find parking at the hospital(ok, ok, I know some people bike to work and this isn’t a problem for them)Working with multiple junior learnersReceive many handoversDay full of complex patientsThere are no beds to see patients in- Dont get a chance to eat lunch (doctors that don’t eat make more mistakes, you can build this in)
Get yelled at by patientsReceive patient complaint- Leave your shift two hours late (leaving on time is important for my wellness, and for the most part, I can control this variable with how I approach my shifts).
There are a few variables there that I ultimately have control over; my morning routine (maybe leave the house earlier so you can establish your own tone for arriving to work), the ability to eat lunch and the ability to leave on time (sometimes these are beyond your control, but for the most part we can control these variables). Otherwise, the remainder of the ‘physiologic stress’ incurred on that day are due to things that we have no control over, so physiologically stressing over them provides no benefit.It isn’t to say that our occupational wellness isn’t draining – because it is, which is why we need to counter it.
I used to have some road rage (drivers in Ontario – I’m looking at you), but I eventually recognized that getting angry at other cars on the road only made me physiologically unwell, and accomplished nothing; so why do that to myself? I started to view my occupational physiologic stressors in the same light.
Find moments on a shift that ground you
There are good things in medicine, and it is important to allow ourselves the opportunity to seek out and bask in these moments. For some, this is a laceration repair or abscess drainage, maybe managing a sick trauma patient, teaching residents or having good rapport with a family. This is individual and personal, but we must seek out these moments, and afford ourselves the opportunity to enjoy these moments (and sometimes that means signposting it for ourselves, or reflecting on it after our shift).
Perspective is also a valuable tool. I may be having a bad day, or having some personal challenges, but when I see three patients under the age of 40 with cancer, my perspective on my own circumstances changes drastically. For me, that perspective is both humbling and valuable.
Every shift is going to have positive and negative moments – instead of framing a shift as “that was a crazy shift” (in a negative way), we can instead view it as a life trajectory we changed, strong team dynamics or good medicine. We love to tell stories in medicine, but the dichotomy of how we experience things has a huge influence on how we experience our occupational wellness. But, you have to have some insight into how you internalize these cases and experiences.
The transition
Through this post, we’ve identified that within a struggling healthcare system, it may feel disingenuous to suggest healthcare providers need more personal resiliency and agency, but the reality remains that the system does not care about your burnout. So in order to minimize the amount of energy taken from you due to your (lack of) occupational wellness, one needs to ‘take things into their own hands’. The notion of personal agency is immensely powerful, as it can help us recognize domains of our occupational wellness that ARE within our control, and acknowledging that we cannot stress about things beyond our control, for these physiologic stressors are bad for us.
In our next post, we’re going to dive into how we can integrate some of these principles more seamlessly into our work and lives.
Medicine is a community, so we’d love to hear your insights and on how you optimize your own occupational wellness!