Lacerations are a common presenting complaint to emergency department. In 2013, in the United States there were 7 million visits to the emergency department (ED) for lacerations making up a total of 5.2% of ED visits(1). Let’s review some of the evidence (or lack thereof) surrounding laceration repair so that we can be better at managing this common presentation.
Types of wound closure
Primary closure: bringing the edges of the wound together with stitches, adhesive tape, staples or glue.
Secondary closure: the wound is left open and allowed to close spontaneously.
Delayed/Tertiary closure: wound is cleaned, left for 2-3 days, checked to see if it is still clean, and then close. This is thought to decrease the chances of infection. (2)
Question 1: When can I use Primary Closure?
- In the literature, a “golden period” of 6 hours for wound closure has been frequently cited (3–5).
- This concept dates back to 1898 when Paul Leopold Friedrich inoculated lacerated guinea pigs’ skin with bacteria and then excised the wound before and after 6 hours. He concluded that if the wound was excised in more than 6 hours, the guinea pig would die (4).
With regards to timeframes for laceration repair, there is limited robust, high-quality evidence on this topic. Recently, there have been multiple publications that have challenged this notion citing limited evidence, please find relevant studies below.
- The impact of wound age on the infection rate of simple lacerations repaired in the emergency department (Zehtabchi et al. 2012) (3)
- Study type: systematic review
- Included: ED patients with lacerations repaired by primary closure
- Excluded: patients who presented with delayed primary repair or secondary closure, wounds requiring intra-op repair, skin graft, drains or extensive debridement, and grossly contaminated or infected wounds at presentation.
- Comparison of wound infection between early and delayed wound closure.
- 4 trials enrolling 3724 patients in aggregate met inclusion/exclusion criteria were identified.
- All were prospective studies with low quality of evidence.
- One study with a small sample size that enrolled lacerations to the hand and forearm showed a higher rate of infection in patients with delayed wound closure over 12 hours (RR 4.8, 95% CI 1.9-12.0).
- Bottom Line: Evidence does not support the golden period nor supports the role of wound age in infection rate in simple lacerations, however, there was significant heterogeneity among trials.
- Primary closure versus delayed closure for nonbite traumatic wounds within 24 hours post-injury. (Eliya-Masamba, Banda 2013) (2)
- Study type: systematic review
- No systematic evidence was found – as no studies met inclusion criteria.
- Bottom Line: insufficient evidence to recommend delayed vs primary closure.
- Traumatic Lacerations: What are the risks for infection and has the “golden period” of laceration care disappeared? (Quinn et al. 2014) (4)
- Study type: Multicenter, prospective cohort study.
- Included: Consecutive patients with traumatic lacerations at three diverse emergency departments.
- Patients were followed for 30 days to determine the development of wound infection
- 2663 patients completed follow-up, 69 developed an infection (2.9%).
- No difference in infection rates for lacerations closed before or after 12 hours (3% vs 1.2%).
- Bottom Line: Type II diabetes, wound contamination, length >5cm, and location on the lower extremity were important risk factors for the development of wound infections. Time from injury to wound closure was not as important as previously thought.
- Is the use of a specific time cut-off or “golden period” for the primary closure of acute traumatic wounds evidence-based? A systematic review. (Jaman et al. 2021)(5)
- Study type: systematic review
- Included: prospective observational, retrospective, and randomized control studies on patients of any age requiring acute surgical wound care who presented to EDs or other healthcare facility.
- Excluded: studies in which wound management was deliberately postponed were, studies involving only bite wounds.
- Nine studies met the inclusion criteria.
- Bottom Line: Unable to determine a specific time frame in which wounds can be primarily closed.
As you can see, there is no robust, high-quality evidence. Given this, there is certainly a high degree of practice variation. Practically speaking, I reached out to two plastic surgery colleagues:
- Katie Hicks (PGY5 University of Toronto Plastic and Reconstructive Surgery)
- Primary closure is appropriate up to 24-48h after the injury. This can be case-dependent, if there is a significant wound to a cosmetically sensitive area (e.g. face), there can be a role for debridement and primary closure by plastic surgery.
- Alison Baergen (PGY4 University of Ottawa Plastic and Reconstructive Surgery)
- Primary closure is appropriate for up to 24 hours on the face/scalp with good irrigation. For limbs can be up to 12 hours but will be case-dependent. Dr. Baergen also recommends consideration of an x-ray to rule out foreign bodies, fractures or dislocation as these can be commonly missed if a cut is thought to look superficial.
Answer #1:
- Low-quality research evidence without true consensus.
- Discuss risks and benefits with your patient and consider cosmesis.
- Per discussion with our plastic surgery colleagues:
- Face: up to 24-48 hours
- Limbs: between 12-24 hours (variable)
- Animal and human bites on the face should be closed primarily with appropriate antibiotic prophylaxis.
- Per discussion with our plastic surgery colleagues:
Question #2: How Should I Repair the Laceration?
- There are various methods in which lacerations can be repaired primarily in the ED.
- We should consider both patient and wound factors when taking this into consideration
- Patient
- Patient cooperation
- Comorbidities
- Wound
- Location
- Length
- Depth
- Similar to the timing of laceration repair there are few robust studies investigating the differences between laceration repair techniques. Please see some of the relevant studies below.
- A randomized control trial comparing the hair apposition technique with tissue glue to standard suturing in scalp lacerations (Hock et al.) 2002 (6)
- Study type: Randomized control trial
- Inclusion criteria: linear lacerations to the scalp less than 10cm long
- Exclusion criteria: severely contaminated wounds, actively bleeding wounds, patients with hair strands less than 3cm, and hemodynamically unstable patients were excluded
- Randomized to hair apposition technique (HAT) vs standard suturing
- Wounds were then evaluated 7 days later, non-blinded for wound healing, scarring, and complications
- 96 and 93 patients in the study and control groups
- Wound healing trended toward being judged more satisfactory in the HAT group than standard suturing (100% versus 95.7%; P=.057; effect size 4.3%; 95% confidence interval 0.1% to 8.5%)
- Patients who underwent HAT had less scarring (6.3% versus 20.4%; P=.005), fewer overall complications (7.3% versus 21.5%; P=.005), significantly lower pain scores (median 2 versus 4; P<.001), and shorter procedure times (median 5 versus 15 minutes; P<.001)
- There was a trend toward less wound breakdown in the HAT group (0% versus 4.3%; P=.057). When patients were asked whether they were willing to have HAT performed in the future, 84% responded yes, 1% responded no, and 15% were unsure.
- Limitations: Nonblinded, small study.
- Bottom Line: HAT is equally acceptable and perhaps superior to standard suturing.
- A randomized control trial comparing the hair apposition technique with tissue glue to standard suturing in scalp lacerations (Hock et al.) 2002 (6)
- Patient
-
-
- Comparison of Hair Knotting with Primary Suture and Stapler Techniques in Scalp Lacerations: A prospective observational study (Gur et ) 2023 (7)
- Study type: single-center, prospective observational study
- Inclusion criteria: patients with hair length greater than 3cm and linear laceration less than 10cm.
- Exclusion criteria: active bleeding wounds, severely contaminated wounds, unconscious patients, unstable patients, and pregnant women.
- Patients were divided into 3 groups (40 patients per group) according to treatment technique – hair knotting, stapler, and primary closure with sutures.
- Shorter LOS in the ED (23 minutes) in the hair knot group vs 35.5 minutes in the stapler group and 42 minutes in the primary suture group, which was statistically significant (p= 0.003 and p=0.001)
- Lower complications in the hair knot group as well as lower rate of cosmetic problems.
- Limitations: observational and small study.
- Bottom Line: HAT can be used as an alternative to suturing and staples for hair lacerations in the ED.
- Tissue Adhesives for Traumatic Lacerations in Children and Adults (Farion et al.) 2002 (8)
- Study type: systematic review
- Population: children and adults
- 13 studies included
- 11 studies compared a tissue adhesive with standard wound closure – no significant difference was found for cosmesis
- Pain scores and procedure times favored tissue adhesives.
- Bottom Line: tissue adhesives are acceptable alternative when compared to standard wound closure.
- Benefits: decreased procedure time and pain
- Risks: small but statistically significant increased rate for wound dehiscence (favouring standard wound care NNH 40; 95% CI 20 to 1168) and erythema (favouring tissue adhesive NNH 10; 95% CI 5 to 239).
- Now let’s have a look at the differences between absorbable and non-absorbable sutures. Putting in absorbable sutures can be helpful for patients so that they do not have to come back for a second visit for suture removal.
- A Randomized Control Trial Comparing long-term cosmetic outcomes or traumatic pediatric lacerations repairs with absorbable plain gut vs nonabsorbable nylon (Karounis et al.) 2004 (9)
- Study Type: Randomized control trial
- Inclusion criteria: patients between 1-18yo presenting to a pediatric emergency department with lacerations <12 hours old
- Exclusion criteria: if can be approximated by tissue adhesives, animal/human bites, gross contamination, puncture or crush wounds, wounds crossing joints, tendon/nerve damage
- Patients were divided into two groups: absorbable plain gut vs nonabsorbable
- Evaluated at 10 days by a research nurse, also assessed by a blinded plastic surgeon at 4-5 months
- Study population: 147 patients, 95 enrolled, rest declined
- No difference at short-term follow-up for rates of infection or dehiscence
- 65/95 patients presented for long-term follow-up, no difference was found in the wound evaluation score or visual analog scale of cosmesis
- Bottom Line: No difference found between plain gut and nonabsorbable nylon for repair of traumatic lacerations in pediatric lacerations.
- Absorbable versus Nonabsorbable sutures in the management of traumatic lacerations and surgical wounds (Al-Abdullah et ) 2007 (10)
- Study type: Meta-analysis
- 7 randomized control trials that met inclusion criteria, 3 that analyzed traumatic wounds, 4 analyzing surgical wounds
- Results:
- Infection: no difference, reported only by 6/7 studies
- Cosmesis:
- Only reported by 2/7 studies
- Long-term cosmesis had no difference in the two studies
- Short and long-term cosmesis examined in one study, point estimates favoured nonabsorbable sutures, but no significant difference
- Wound dehiscence: reported only by one study, no statistically significant difference
- Bottom Line: Lack of large, well-conducted RCTs to address this topic. From limited evidence – no difference between absorbable and nonabsorbable sutures.
- A Randomized Control Trial Comparing long-term cosmetic outcomes or traumatic pediatric lacerations repairs with absorbable plain gut vs nonabsorbable nylon (Karounis et al.) 2004 (9)
- Comparison of Hair Knotting with Primary Suture and Stapler Techniques in Scalp Lacerations: A prospective observational study (Gur et ) 2023 (7)
-
-
-
-
-
- Cosmetic outcomes of absorbable versus nonabsorbable sutures in pediatric lacerations (Luck et ) 2008 (11)
- Study type: Randomized clinical trial
- Inclusion criteria: healthy patients 1-18yo presenting to pediatric ED with facial lacerations
- Exclusion criteria: <1cm, >5cm, irregular borders, result of mammalian bite, contaminated, > 8hours old, could be repaired with topical adhesive
- Randomized to repair with fast-absorbing cat gut or nylon
- Followed up at 5-7 days where sutures were removed, then again at 3 months
- 3 observers who were blinded used visual analog scale (VAS) rated photographs of the wounds at 3 months
- Parents also rated the wound
- 88 patients enrolled, 47 completed the study
- Observers mean VAS score did not have any significant difference
- Parents also did not have a difference in the VAS score and no differences in the rates of infection, wound dehiscence, keloid formation, and parental satisfaction were seen
- Bottom Line: No significant differences between absorbable and non-absorbable sutures. Both types of sutures were removed 5-7 days after insertion.
- Cosmetic outcomes of absorbable versus nonabsorbable sutures in pediatric lacerations (Luck et ) 2008 (11)
-
-
-
-
-
-
-
- Comparison of cosmetic outcomes of absorbable versus nonabsorbable sutures in pediatric facial lacerations (Luck et ) 2013 (12)
- Study type: randomized clinical trial
- Inclusion criteria: healthy patients, 1-18yo presenting to the ED with noncontaminated, linear facial lacerations 1-5cm in length
- Exclusion criteria: <1cm, >5cm, irregular borders, result of mammalian bite, contaminated, >8 hours old, could be repaired with topical adhesive
- Randomized to repair with fast-absorbing cat gut or nylon
- Returned at 4-7 days for follow-up and suture removal in nonabsorbable group, and then in 3-4 months photographs taken and surveys of caregivers performed
- 98 patients enrolled, 76 caregiver surveys completed, 61 photographs scored by physicians
- Higher VAS scores given by physicians to the nylon group – noninferiority was not able to be established with regards to the VAS
- Caregiver VAS scores were similar, found to be non-inferior
- In terms of convenience, caregivers preferred absorbable 36/36 vs 21/36, and regarding suture material for future repairs, they preferred absorbable 36/36 vs 26/36
- Limitations: high attrition rate, unclear if discharge instructions were followed in all patients, small sample size
- Bottom Line: Caregiver assessment of wounds showed noninferiority between absorbable and nonabsorbable sutures and absorbable sutures were preferred by caregivers. Noninferiority with respect to cosmetic outcomes not established for physician assessment.
- A comparison of cosmetic outcomes of the laceration on the extremities and trunk using absorbable versus nonabsorbable sutures (Tejani et ) 2014 (13)
- Study type: randomized control trial
- Inclusion criteria: pediatric or adult patients with linear, small (<8cm) lacerations, minimally contaminated on the trunk or extremities
- Exclusion criteria: facial lacerations, visible dirt in the wound, >12h, nonlinear shape, bites, significant past medical history, daily steroid use, wound over an area of tension, previous reaction to topical anesthetic
- Randomized to vicryl rapide or prolene sutures
- Follow up at 10 days to assess for wound infection and dehiscence
- At 3 months wounds were photographed, and evaluated by blinded plastic surgeons for cosmetic outcome
- Noninferiority of the VAS assessment
- No statistical differences in the rate of complications but trend towards more infections in the absorbable group (4 infections with absorbable 11% vs 1 with prolene 3%)
- Limitations: low reliability, complications documented by phone by patients
- Bottom Line: Given the limitations of this study, ED physicians should consider vicryl rapide for laceration repair on the trunk and extremities as it provides a similar cosmetic outcome.
- Comparison of cosmetic outcomes of absorbable versus nonabsorbable sutures in pediatric facial lacerations (Luck et ) 2013 (12)
-
-
-
-
-
-
-
- Using Absorbable Sutures for Traumatic Wound Closure to Avoid Additional Hospital Visits for Suture Removal During the COVID-19 Pandemic: A Randomized Controlled Trial (Alkandari et ) 2022 (14)
- Study Type: Randomized Control Trial
- Inclusion criteria: healthy, 1-60yo, not on antibiotics or anti-inflammatories, open traumatic wound >2cm within 24hours, in a low tension area away from joints/bony prominences
- 471 patients randomized to treatment with non-absorbable sutures (control group) or rapid-onset absorbable sutures (treatment group)
- Phone/video call follow-up was performed after 21 days and parameters were compared between groups
- No difference in wound infection was observed between the two groups
- Using absorbable sutures resulted in significantly fewer (p<0.001) post-op hospital visits compared to using non-absorbable sutures (1 vs 3 visits)
- Two patients in the non-absorbable group had suture remnants under the skin due to inadequate self-removal
- Limitations: single center, wound infection was subjective – reported by patients over the phone
- Bottom Line: Laceration repair with absorbable sutures for traumatic lacerations is safe with regard to wound healing and infection rates. It also decreases post-operative hospital visits.
- Using Absorbable Sutures for Traumatic Wound Closure to Avoid Additional Hospital Visits for Suture Removal During the COVID-19 Pandemic: A Randomized Controlled Trial (Alkandari et ) 2022 (14)
-
-
-
-
-
-
-
- There are multiple small studies with a low level of evidence as you can see above showing that absorbable sutures have similar outcomes to nonabsorbable with the potential for improved patient convenience as they do not need to return to have sutures removed.
- Now let’s have a brief look at staples with regards to laceration repair. There was very little literature in this specific area and there were no studies that I was able to find with regards to sutures strictly in the emergency department setting. Let’s have a look at one study that attempted to look into this question, albeit in a different setting.
- Surgical wound closure by staples or sutures? Systematic review. (Cochetti et ) 2020 (15)
- Study Type: Systematic review and meta-analysis
- Included RCTs and cluster-randomized trials comparing staples with sutures for adults who had undergone any type of surgery
- 42 very low-quality RCTs with a total of 11067 patients were included
- Sutures result in slightly fewer overall wound infections compared to staples (4.9% vs 6.75%)
- Bottom Line: low quality of evidence, conclude that sutures reduce postop pain and improve the grade of satisfaction with the cosmetic outcome.
- Again, I reached out to two of my plastic surgery colleagues for this question. Please find their practice patterns below.
- Katie Hicks (PGY5 University of Toronto Plastic and Reconstructive Surgery)
- Pediatric – absorbable.
- Adult
- Face – non-absorbable as this causes less of an inflammatory reaction and better scar.
- Rest of body – either is appropriate.
- If unreliable patient, consider absorbable regardless of location.
- Alison Baergen (PGY4 University of Ottawa Plastic and Reconstructive Surgery)
- Pediatric – absorbable.
- Adult
- Face – non-absorbable.
- Rest of body – either is appropriate. Recommendation for plain gut sutures for laceration repair if picking an absorbable suture. These can cause more inflammation/scarring from her experience and so if the patient is reliable and can follow up, consider using non-absorbable.
- Katie Hicks (PGY5 University of Toronto Plastic and Reconstructive Surgery)
- Surgical wound closure by staples or sutures? Systematic review. (Cochetti et ) 2020 (15)
-
-
-
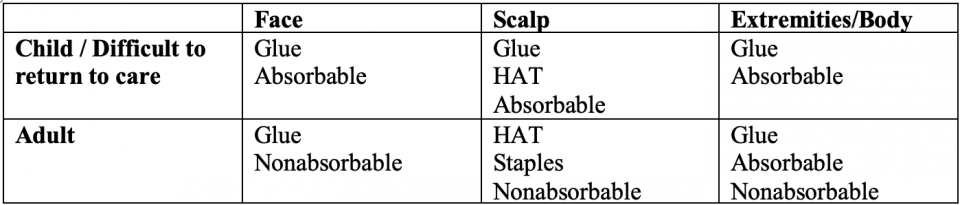
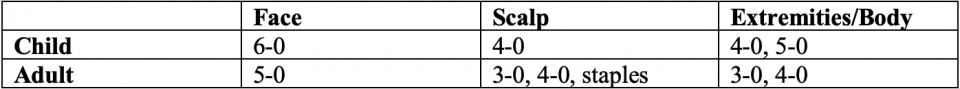
Answer #2:
- Consider glue and hair apposition technique when possible in areas of low tension
- Consider absorbable sutures in specific populations where return to care may be difficult
- Please see below for a suggested outline in the choice of laceration repair. Disclaimer: This is NOT evidence-based but a summary from a review of literature and expert opinion.
PART 2: Local Anesthetic Systemic Toxicity (LAST)
Question #3: What is local anesthetic systemic toxicity and how do I treat it?
- Severe complication of local anesthetic use, primarily affecting the cardiovascular and nervous systems
- Incidence: rare complication – 2 to 2.8 per 10,000 peripheral nerve blocks(17)
- Local anesthetic mechanism of action (17)
- Block cell membrane-based voltage-gated sodium channels, preventing sodium influx, subsequent depolarization, and generation of action potentials, primarily in the cardiac and central nervous systems
- Can also block calcium and potassium channels
- As plasma levels of the local anesthetic increase, CNS depression can occur, resulting in altered mental status, coma, and respiratory arrest
- Within the cardiovascular system, local anesthetics can produce myocardial dysfunction, disturbances in conduction, and vascular tone lability
- Bupivacaine and ropivacaine are more likely to cause cardiac dysrhythmias, whereas lidocaine and mepivacaine are more likely to decrease contractility, manifesting as systemic hypotension
- Toxic doses for common local anesthetics (17) :
- Bupivacaine
- 2 mg/kg without epinephrine
- 3 mg/kg with epinephrine
- Lidocaine
- 5mg/kg without epinephrine
- 7 mg/kg with epinephrine
- Gitman and colleagues published a review in 2018 that looked at 47 cases of LAST found in 35 peer-reviewed articles (18)
- They found that bupivacaine was involved in 36% of LAST cases followed by lidocaine was the culprit in 26% of cases
- LAST was most common in penile blocks (23%) followed by local infiltration (17%)
- Bupivacaine
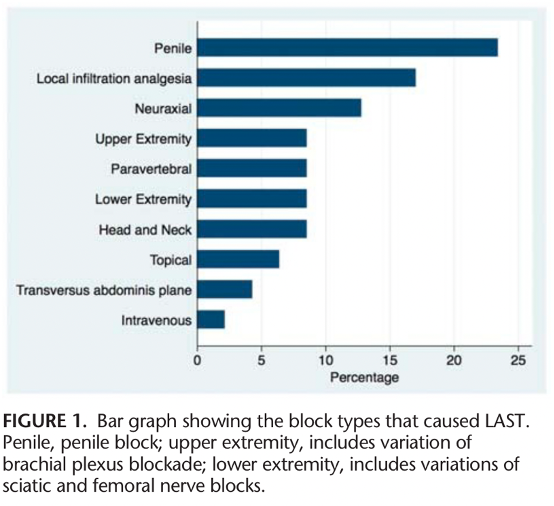
Above graph from study by Gitman et al. (18)
Risk Factors
- Medication Factors:
- Type of local anesthetic agent
- Total dose administered
- Patient Factors: infants, elderly, and patients with mitochondrial dysfunction (17)
- Infants are at higher risk due to immature hepatic enzymes that may increase the free fraction of the local anesthetic in the plasma(19)
- The elderly have a reduced local anesthetic clearance due to reduced organ perfusion and pharmacodynamic function, thereby increasing the potential of drug accumulation with repeated boluses of local anesthetic or continuous infusion
- Medication administration factors
- Highly vascular tissues
- Local anesthetic without epinephrine
- Direct injection into the vasculature
- Can happen with topical administration (oral viscous lidocaine) or EMLA patches
Presentation
- Timing of onset
- There is variability in time of onset of symptoms from the time of local anesthetic administration
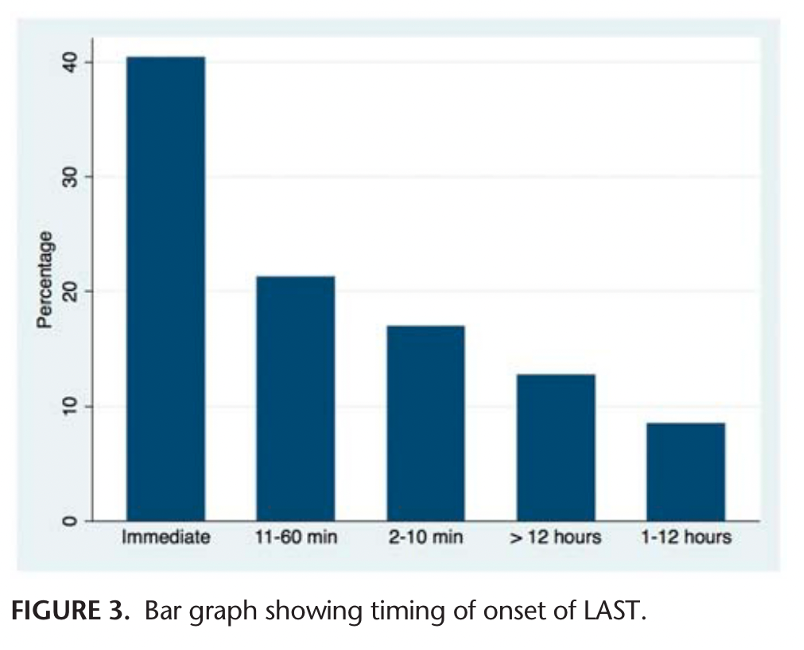
Timing of LAST onset from study by Gitman et al.
- 25% experience symptoms within 1 min of injection, 22% experience symptoms within 1-5 min, 10% within 6-10 min and 20% within 11-30 min(17)
- CNS is the most common feature of LAST (68-77%) (17)
- Primarily in the form of seizures
- Early manifestations
- Peri-oral paresthesia
- Confusion
- Audio-visual disturbances
- Dysgeusia
- Restlessness
- Tremors
- Later manifestations
- agitation
- Seizures
- ALOC
- CVS
- Up to 1/3 of cases will progress to significant cardiovascular manifestations with dysrhythmias and/or hypotension, while 10% of LAST patients will have isolated and less severe CVS signs (17)
- Early: hypertension and tachycardia
- Late
- Vasodilation and hypotension
- Sinus bradycardia, AV block
- Ventricular dysrhythmias
- Cardiac arrest
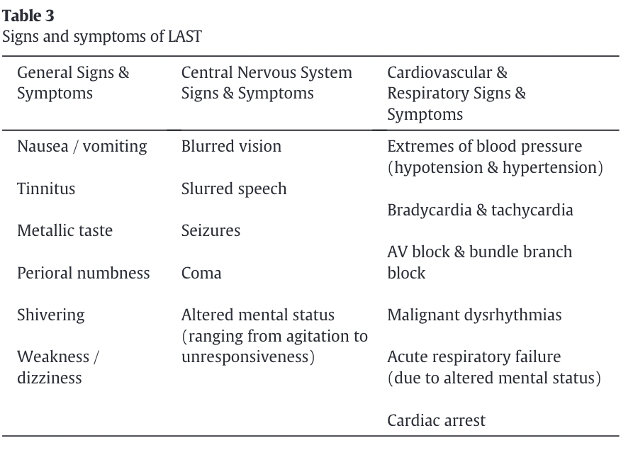
Table of signs and symptoms of LAST from review by Long et al
Management
- Early recognition is important
- Discontinue injection of local anesthetic if ongoing
- Application of supplemental oxygen as needed
- Consideration of intubation if the airway is compromised, oxygenation is impaired or ventilation is in inadequate (17)
- Benzodiazepines can be administered for seizures at usual dosing
- If seizures do not resolve with the administration of benzodiazepines, small doses of propofol can be used (19)
- The following ACLS modifications should be made if there is a cardiac arrest (17,19):
- Epinephrine reduced to 1 ug/kg as standard dosing can worsen arrhythmia
- Avoid vasopressin, calcium channel blockers, beta-blockers as they can worsen hypotension
- Local anesthetics such as lidocaine should be avoided for ventricular dysrhythmias
- Amiodarone can be used if there is a ventricular dysrhythmia
- For patients with refractory cardiac arrest, extracorporeal membrane oxygenation (ECMO) may be required (17)
- Intravenous lipid emulsion therapy (20%) should be immediately administered for patients with seizures or severe cardiotoxicity (hemodynamically compromising dysrhythmias, hypotension, cardiac arrest)
- The dose is dependent on the weight of the patient (19)
- Body weight > 70kg
- Bolus 100 mL over 2-3 mins
- Followed by 20% lipid emulsion infusion of 200-250 mL over 15-20mins
- Body weight < 70kg
- Bolus 1.5mL/kg over 2-3 mins
- Followed by 20% lipid emulsion infusion of 0.25mL/kg-min
- If patient continues to be unstable, can repeat bolus up to two times and increase the infusion to 0.5mL/kg-min
- The maximum recommended dose of 10% lipid emulsion is 12 mL/kg
- Patient disposition will depend on the severity of LAST
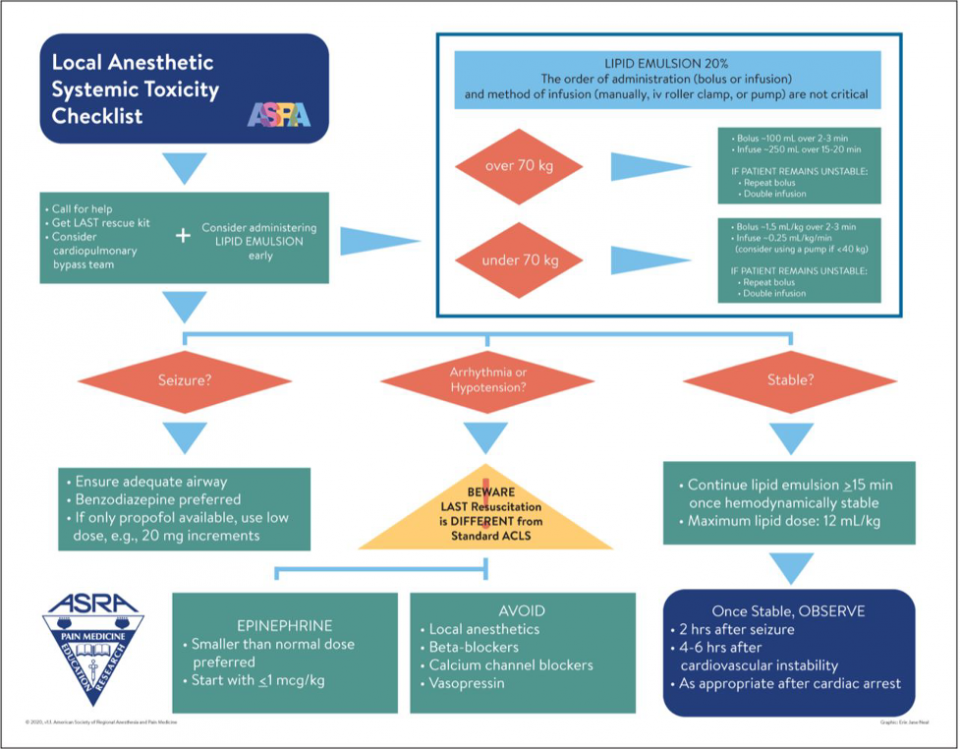
Neal et al Publication or reproduction of the checklist for commercial use requires written permission from ASRA. Graphic: Erin J. Neal.(20)
References
- Mankowitz SL. Laceration Management. The Journal of Emergency Medicine. 2017 Sep;53(3):369–82.
- Eliya-Masamba MC, Banda GW. Primary closure versus delayed closure for non bite traumatic wounds within 24 hours post injury. Cochrane Wounds Group, editor. Cochrane Database of Systematic Reviews [Internet]. 2013 Oct 22 [cited 2023 Nov 4]; Available from: https://doi.wiley.com/10.1002/14651858.CD008574.pub3
- Zehtabchi S, Tan A, Yadav K, Badawy A, Lucchesi M. The impact of wound age on the infection rate of simple lacerations repaired in the emergency department. Injury. 2012 Nov;43(11):1793–8.
- Quinn JV, Polevoi SK, Kohn MA. Traumatic lacerations: what are the risks for infection and has the ‘golden period’ of laceration care disappeared? Emerg Med J. 2014 Feb;31(2):96–100.
- Jaman J, Martić K, Rasic N, Markulin H, Haberle S. Is the use of specific time cut-off or “golden period” for primary closure of acute traumatic wounds evidence based? A systematic review. Croat Med J. 2021 Dec;62(6):614–22.
- Hock MOE, Ooi SBS, Saw SM, Lim SH. A randomized controlled trial comparing the hair apposition technique with tissue glue to standard suturing in scalp lacerations (HAT study). Annals of Emergency Medicine. 2002 Jul;40(1):19–26.
- Gür A, Tekin E, Özlü İ, Tortum F, Çimen EY. Comparison of Hair Knotting with Primary Suture and Stapler Techniques in Scalp Lacerations: A Prospective, Observational Study. Eurasian J Emerg Med. 2023 Jun 1;22(2):107–13.
- Farion KJ, Russell KF, Osmond MH, Hartling L, Klassen TP, Durec T, et al. Tissue adhesives for traumatic lacerations in children and adults. Cochrane Wounds Group, editor. Cochrane Database of Systematic Reviews [Internet]. 2002 Jul 22 [cited 2023 Nov 4];2010(1). Available from: http://doi.wiley.com/10.1002/14651858.CD003326
- Karounis H, Gouin S, Eisman H, Chalut D, Pelletier H, Williams B. A Randomized, Controlled Trial Comparing Long-term Cosmetic Outcomes of Traumatic Pediatric Lacerations Repaired with Absorbable Plain Gut versus Nonabsorbable Nylon Sutures. Academic Emergency Medicine. 2004 Jul;11(7):730–5.
- Al-Abdullah T, Plint AC, Fergusson D. Absorbable Versus Nonabsorbable Sutures in the Management of Traumatic Lacerations and Surgical Wounds: A Meta-Analysis. Pediatric Emergency Care. 2007 May;23(5):339–44.
- Luck RP, Flood R, Eyal D, Saludades J, Hayes C, Gaughan J. Cosmetic Outcomes of Absorbable Versus Nonabsorbable Sutures in Pediatric Facial Lacerations. Pediatric Emergency Care. 2008;24(3).
- Luck R, Tredway T, Gerard J, Eyal D, Krug L, Flood R. Comparison of Cosmetic Outcomes of Absorbable Versus Nonabsorbable Sutures in Pediatric Facial Lacerations: Pediatric Emergency Care. 2013 Jun;29(6):691–5.
- Tejani C, Sivitz AB, Rosen MD, Nakanishi AK, Flood RG, Clott MA, et al. A Comparison of Cosmetic Outcomes of Lacerations on the Extremities and Trunk Using Absorbable Versus Nonabsorbable Sutures. Zehtabchi S, editor. Academic Emergency Medicine. 2014 Jun;21(6):637–43.
- Alkandari AF, Soliman DM, Madhyastha S, Alawadhi AA, Alawadhi FA, Almotairi NM, et al. Using Absorbable Sutures for Traumatic Wound Closure to Avoid Additional Hospital Visits for Suture Removal During the COVID-19 Pandemic: A Randomized Controlled Trial. Cureus [Internet]. 2022 Oct 6 [cited 2023 Nov 6]; Available from: https://www.cureus.com/articles/104880-using-absorbable-sutures-for-traumatic-wound-closure-to-avoid-additional-hospital-visits-for-suture-removal-during-the-covid-19-pandemic-a-randomized-controlled-trial
- Cochetti G, Abraha I, Randolph J, Montedori A, Boni A, Arezzo A, et al. Surgical wound closure by staples or sutures?: Systematic review. Medicine. 2020 Jun 19;99(25):e20573.
- Forsch RT. Essentials of skin laceration repair. Am Fam Physician. 2008 Oct 15;78(8):945-51. PMID: 18953970.
- Long B, Chavez S, Gottlieb M, Montrief T, Brady WJ. Local anesthetic systemic toxicity: A narrative review for emergency clinicians. The American Journal of Emergency Medicine. 2022 Sep;59:42–8.
- Gitman M, Barrington MJ. Local Anesthetic Systemic Toxicity: A Review of Recent Case Reports and Registries. Regional Anesthesia and Pain Medicine. 2018 Jan;1.
- El-Boghdadly K, Pawa A, Chin KJ. Local anesthetic systemic toxicity: current perspectives. LRA. 2018 Aug;Volume 11:35–44.
- Neal et al. Publication or reproduction of the checklist for commercial use requires written permission from ASRA Pain Medicine. Graphic: Erin J. Neal. ACLS, Advanced Cardiac Life Support; LAST, Local Anesthetic Systemic Toxicity.