In this post, we will discuss the use of neuromuscular blocking agents (NMBAs) for intubation in the Emergency Department; we will focus on considerations in predicted difficult airways (RSI vs. awake intubation), Rocuronium vs. Succinylcholine, and the indications for Sugammadex.
This post will not cover laryngoscopy; although this was previously well covered by Dr. Peter Reardon’s previous Grand Rounds Summary post
When should a paralytic be used for intubation in the Emergency Department?
Rapid sequence intubation (RSI), with induction and paralysis, should be the first line intubation strategy in the Emergency Department unless the airway is predicted to be difficult.
When compared to induction agents alone, intubation with induction and paralytic agents result in better intubating conditions, higher first pass success, and fewer complications.1–4 In a 2017 Cochrane review comparing intubating conditions with and without NMBAs, not using a NMBA was associated with a significantly increased risk of difficult intubation (RR 13, NNH 1.9).5
When an airway is predicted to be difficult, that is, when intubation and/or ventilation is predicted to be difficult, a NMBA that takes away a patient’s spontaneous respirations is not recommended, as this may increase your risk of a “can’t intubate, can’t ventilate” scenario, necessitating a surgical airway.
What is a difficult airway?
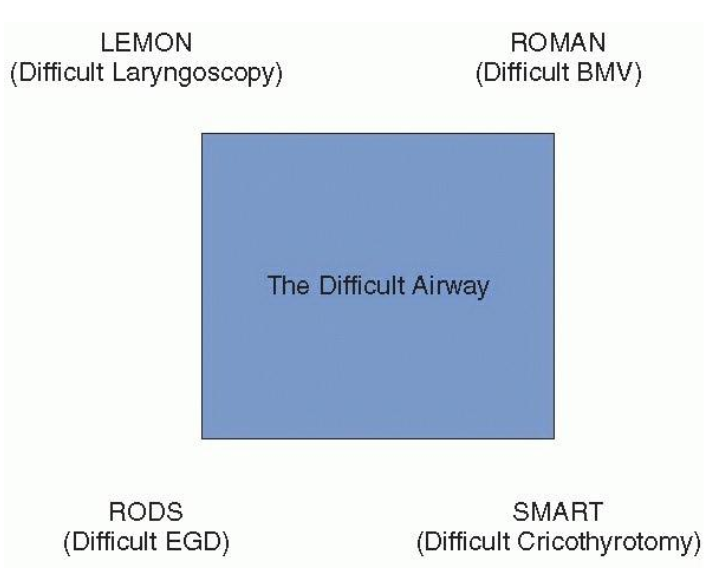
There are cases where the predicted difficulty of the airway is obvious (e.g., facial trauma, massive angioedema, or advanced Ludwig’s angina). But in many other cases, the difficulty of the airway is more subtle. We have many mnemonics to help us remember what to look for on our airway assessment, but how good are we at predicting difficult airways?
In a Danish cohort study of >180,000 intubations, just over 3,000 intubations were recorded to be difficult, of which, 93% were unanticipated. When an intubation was predicted to be difficult, only 25% of these were actually difficult. Difficult bag mask ventilation was unanticipated in 94% of cases, and only 22% of predicted difficult mask ventilations were actually difficult.6
In a recent study by John Sakles from the University of Arizona examining 500 ED intubations, 11% of intubations were predicted to be difficult, yet 80% of these difficult intubations received a neuromuscular blocking agent anyway, and their first pass success was 82%, with 100% overall success and no failed airways or surgical airways.7
And what about physiologically difficult airways? Intuitively we are often taught to use an awake approach for patients with deranged physiology such as refractory hypoxemia and severe metabolic acidosis, yet this management is not actually guided by robust evidence.8
For further information on the physiologically difficult airway, see Dr. Lauren Lacroix’s previous Grand Rounds Summary post
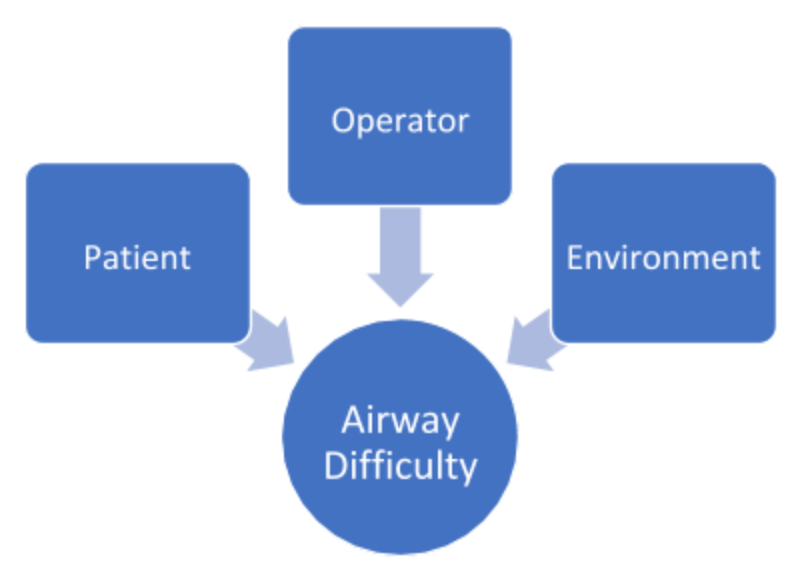
Some would argue that the concept of a difficult airway is a combination of the patient, the clinician, and the environment.9 For example, an experienced anesthesiologist in the OR with a fiberoptic scope might not find an obese Mallampati 4 patient difficult, while a PGY-2 on ICU call overnight may have difficulty with a Mallampati 1 patient.
There simply is no good way to define or predict a difficult airway. In the end, a difficult airway is an airway that is difficult for you.
For an approach to the Pediatric Airway, see Dr. Rebecca Brown’s previous Grand Rounds Summary post
Conceptual framework for RSI vs “awake” intubation

What are the contraindications to succinylcholine?
Absolute contraindications
- Personal or family history of malignant hyperthermia
- Myopathies
- Inherited
- Muscular dystrophies
- Myotonia
- Acquired
- Dermatomyositis
- Polymyositis
- Rhabdomyolysis
- Inherited
- Acetylcholine receptor upregulationa
- Burns
- Crush injury
- Severe infection
- Massive muscle atrophy
- Denervation
- Spinal cord injury
- Stroke
- Guillain-Barre
- Botulism
- Multiple sclerosis
- Amyotrophic lateral sclerosis
- Known allergy
Relative contraindications
- Pre-existing hyperkalemiab
- Predisposition to hyperkalemiab
- Metabolic acidosis
- Chronic kidney disease
- Increased intracranial pressurec
- Myasthenia gravisd
- Cocaine toxicityd
- Plasma pseudocholinesterase deficiencyd
- Increased intraocular pressured
a 3 days to 6 months post event, always safe in first 24 hours
b The Walls Airway Manual suggests that it is “reasonable to use succinylcholine in patients with preexisting hyperkalemia or renal failure unless the ECG shows evidence of myocardial instability from hyperkalemia”
c Subgroup analysis of a retrospective study demonstrated increased mortality in patients with severe traumatic brain injury intubated with succinylcholine.10
d Clinical consequences trivial
Rocuronium vs Succinylcholine
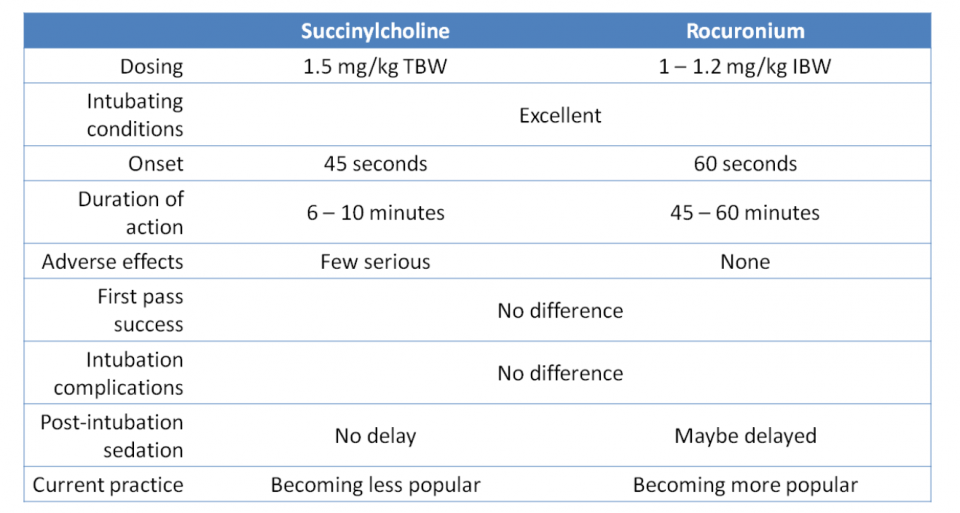
Succinylcholine; the only depolarizing NMBA we use, was introduced in 1951 and has been used since the advent of RSI. Due to its contraindications and side effects, alternative non-depolarizing NMBAs such as vecuronium and rocuronium were introduced. Vecuronium has largely fallen out of favour for RSI due to its slow onset.
There has been an abundance of literature comparing succinylcholine vs. rocuronium and an endless debate about which should be the first line agent for RSI. At the end of the day, it probably does not matter which one you use. There has been no evidence to show one is superior to the other in terms of any meaningful clinical outcomes.1,11 As a clinician, it would be prudent to be familiar with both and know the situations where one would be better than the other.
What is sugammadex?
Sugammadex is a modified cyclodextrin that can inactivate rocuronium or vecuronium and reverse neuromuscular blockade by reducing the amount of free NMBA available to bind to acetylcholine receptors at the neuromuscular junction.12 A dose of 2-4mg/kg is used for routine reversal of deep to moderate neuromuscular blockade. A dose of 16mg/kg is used for immediate reversal of deep neuromuscular blockade within 2 minutes. At The Ottawa Hospital, a 200mg vial costs about $100 and a 500mg vial costs about $200. It is currently used in the operating room by anesthesiologists when reversal with neostigmine is contraindicated or inadequate.
Studies have shown that rocuronium followed by sugammadex at 16mg/kg has faster offset of neuromuscular blockade than succinylcholine.13
Is there a role for sugammadex in unanticipated difficult airway scenarios in the Emergency Department?
No.
Sugammadex is not recommended as “rescue reversal” in a difficult airway scenario for three reasons:14–17
- Critically ill patients who require intubation in the first place will not return to a state of normal respiration as they always have a downward trajectory.
- All airway interventions (BVM, supraglottic airway, surgical airway, etc.) are easier in the paralyzed patient.
- Management of a “can’t intubate, can’t ventilate” scenario is a surgical airway, not reversal of paralysis.
In the ED, sugammadex may eventually have a potential role in reversing paralysis of neurologic patients (eg. traumatic brain injury, status epilepticus, etc.) who are intubated with rocuronium.
Summary
- RSI should be the first line intubation strategy in the ED unless the airway is predicted to be difficult
- We are generally poor at predicting the difficulty of an airway. There is no good way to reliable predict airway difficulty; it is a combination of patient, clinician, and environmental factors
- To conceptualize “awake” intubation vs. RSI:
- The more difficult an airway is predicted to be, the more we tend towards “awake” intubation
- The more urgent the intubation is, the more we tend towards RSI
- There has been no evidence to demonstrate the superiority of either Rocuronium or Succinylcholine in terms of meaningful clinical outcomes
- There is no current role for Sugammadex for rescue reversal in the ED
References
- Brown, C. A., Sakles, J. C. & Mick, N. W. The Walls Manual of Emergency Airway Management 5th Edition. (Wolters Kluwer, 2018).
- Brown, C. A., Bair, A. E., Pallin, D. J. & Walls, R. M. Techniques, success, and adverse events of emergency department adult intubations. Ann. Emerg. Med. 65, 363–370.e1 (2015).
- Pallin, D. J., Dwyer, R. C., Walls, R. M. & Brown, C. A. Techniques and Trends, Success Rates, and Adverse Events in Emergency Department Pediatric Intubations: A Report from the National Emergency Airway Registry. Ann. Emerg. Med. 67, 610–615e1 (2016).
- Wilcox, S. R. et al. Neuromuscular blocking agent administration for emergent tracheal intubation is associated with decreased prevalence of procedure-related complications. Crit. Care Med. 40, 1808–1813 (2012).
- Lundstrom Lars, H., Strande, S., Moller Ann, M. & Wetterslev, J. Use versus avoidance of neuromuscular blocking agent for improving conditions during tracheal intubation or direct laryngoscopy in adults and adolescents. Cochrane Database Syst. Rev. Volume|, (2011).
- Nørskov, A. K. et al. Diagnostic accuracy of anaesthesiologists’ prediction of difficult airway management in daily clinical practice: A cohort study of 188 064 patients registered in the Danish Anaesthesia Database. Anaesthesia 70, 272–281 (2015).
- Sakles, J. C., Douglas, M. J. K., Hypes, C. D., Patanwala, A. E. & Mosier, J. M. Management of Patients with Predicted Difficult Airways in an Academic Emergency Department. J. Emerg. Med. 53, 163–171 (2017).
- Mosier, J. et al. The Physiologically Difficult Airway. West. J. Emerg. Med. 16, 1109–1117 (2015).
- Jaber, S., Jung, B. & Chanques, G. Endotracheal intubation in the ICU. Yearb. Intensive Care Emerg. Med. 2009 313–321 (2007). doi:10.1007/978-0-387-92278-2_30
- Patanwala, A. E., Erstad, B. L., Roe, D. J. & Sakles, J. C. Succinylcholine Is Associated with Increased Mortality When Used for Rapid Sequence Intubation of Severely Brain Injured Patients in the Emergency Department. Pharmacotherapy 36, 57–63 (2016).
- Tran, D. T. T. et al. Rocuronium vs. succinylcholine for rapid sequence intubation: a Cochrane systematic review. Anaesthesia 72, 765–777 (2017).
- Keating, G. M. Sugammadex: A Review of Neuromuscular Blockade Reversal. Drugs 76, 1041–1052 (2016).
- Sørensen, M. K., Bretlau, C., Gätke, M. R., Sørensen, A. M. & Rasmussen, L. S. Rapid sequence induction and intubation with rocuronium-sugammadex compared with succinylcholine: A randomized trial. Br. J. Anaesth. 108, 682–689 (2012).
- Kovacs, G. Sugammadex in the critically ill: Keep ’em sleepin. YouTube (2016). Available at: https://www.youtube.com/watch?v=w-CqtKoZMhI. (Accessed: 30th January 2018)
- Curtis, R., Lomax, S. & Patel, B. Use of sugammadex in a ‘can’t intubate, can’t ventilate’ situation. Br. J. Anaesth. 108, 612–614 (2012).
- Kyle, B. C., Gaylardt, D. & Riley, R. H. A persistant ‘can’t intubate, can’t oxygenate’ crisis despite rocuronium reversal with sugammadex. Anaesth Intensive Care 40, 344–346 (2012).
- Naguib, M., Brewer, L., Lapierre, C., Kopman, A. F. & Johnson, K. B. The Myth of Rescue Reversal in ‘can’t Intubate, Can’t Ventilate’ Scenarios. Anesth. Analg. 123, 82–92 (2016).



