Here we seek to provide a guide on when to consider awake intubation in the Emergency Department (ED), with an approach to the procedure!
The Difficult Airway
When assessing patients who may require any form of airway intervention, we should be assessing for two main entities:
- Difficult anatomy. Ask yourself:
- Do I feel like intubation will be difficult?
- If intubation is challenging, will I still be able to ventilate this patient (eg., BVM, SGA, etc.)?
- Difficult physiology. Identify and address:
- Hypotension and elevated Shock Index
- RV failure
- Apnea Intolerance:
- Hypoxia
- Acidosis
- Hypoventilation (eg., obesity, neuromuscular weakness, etc.)
Burning Your Bridges
Why are the concepts of the anatomically and physiologically difficult airway important? As we’ve reviewed in prior grand rounds (by Drs. Parks and Lacroix), they should change your approach to avoid “burning your bridges.” In patients with predictors of an anatomically difficult airway, we may call for help or reach for airway adjuncts. We tailor our approach to sedation and paralysis to avoid loss of the patient’s airway and a possible “can’t intubate, can’t ventilate/oxygenate” scenario. In patients with challenging physiology, we should focus on optimizing our approach by addressing hypoxia, compromised hemodynamics, and severe acidosis before, during, and after intubation.

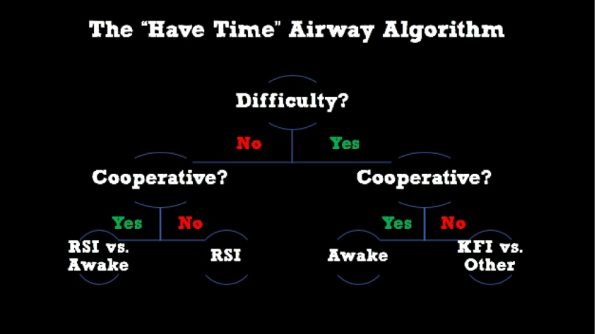
What options do we have when it comes to sedation and analgesia for intubation when difficulty is predicted? In ‘crash airways’ the patient requires intubation in seconds to minutes. Typically our approach to a crash airway is a rapid sequence intubation (RSI) with a double set-up. This is when the patient is rapidly sedated and paralyzed to give the best first attempt using laryngoscopy +/- SGA, ideally with another practitioner in the room capable of performing an emergency cricothyroidotomy. However, more often there is enough time to consider the following options:
- Ketamine-Facilitated Intubation (KFI): The patient is given a dissociative dose (1-2mg/kg) of ketamine with avoidance of paralytics. Topicalization of the airway can be performed as required.
- Awake Intubation: This approach relies primarily or solely on topicalization of the patient’s airway with general avoidance of sedation and paralytics. May provide small amounts of anxiolytics/analgesics as required.
- Sedation-only intubation: Small aliquots of sedative agents (eg. propofol, benzodiazepines) given with avoidance of paralytics.
- Unfortunately, research and expert opinion are demonstrating that sedation-only techniques can include the complications of RSI (hypotension, hypopnea/apnea, baseline aspiration risk, increased incidence of difficult laryngoscopy) without the benefits.
- This is due to the fact that the sedative medications are frequently the culprit of hypotension and negative inotropy. 1
In summary, we should employ “breathing intubation” techniques in patients who require non-emergent intubation with predictors of difficulty- ie. awake vs. KFI.
Theory and Evidence: Awake Intubations
According to multiple high-level, ED-focused sources, we should strongly consider an awake approach to intubation in cooperative patients with predicted difficulty, when the situation permits. .2–4 The theory behind awake intubation is relatively straightforward: with proper topicalization, the patient maintains airway tone and ventilatory drive while the practitioner secures the endotracheal tube.
A recent anesthesia-based prospective observational cohort study shows us that even in a primarily trainee-based setting, awake intubations can be performed with great results:5 This study included 600 awake intubations performed in the OR over a period of three years at a large tertiary care centre in the UK. It demonstrated:
- 99% overall success rate
- 11% complication rate (majority being minor complications such as multiple attempts, oversedation, or mild transient desaturation)
Awake techniques have traditionally been quite cumbersome, challenging, and performed almost exclusively by experienced anesthetists. Fortunately, over the past 10-20 years, the approach to airway topicalization and awake intubation has become much more accessible. It is straightforward and has been employed with success by ED practitioners.6 In addition, for ED providers who are unfamiliar with fiberoptic intubating scopes, recent anesthesia-based literature has shown similar success rates and quicker intubation times for video laryngoscopes compared to fiberoptic intubating scopes.7
The Approach: Awake Intubation
Airway topicalization has multiple straightforward approaches. Click here for a demonstration that requires minimal equipment. It includes:
- Tongue depressor with 5% lidocaine ointment (thumbnail sized, 1-3 applications)
- Atomizer with 5-10mLs of 4% aqueous lidocaine
Clinical pearls for topicalization and awake intubation:
- Approach the intubation as you would any other. An awake technique is simply your “Plan A.” This means you should still have all your airway adjuncts available, sedative/dissociative agents, paralytics, exit strategy, etc. just in case.
- Preoxygenate as you usually would. You can easily work around BiPAP and HFNC masks if needed.
- If the patient’s condition allows, a seated/semi-recumbent position is generally preferred for patient comfort.
- Medications:
- Glycopyrrolate 0.4mg IM 20-30 minutes prior to intubation can help dry up small amounts of airway secretions which may make visualization easier. However, this is not a necessary step.
- Anxiolysis if patient is experiencing significant anxiety or distress:
- Midazolam 0.25-1mg IV
- Avoid oversedation – take the “low and slow” approach
- Analgesia PRN if patient is experiencing discomfort:
-
- Fentanyl 25-50mcg IV
- Ketamine 0.3mg/kg IV over 10 minutes
-
- Coach your patient! This is a procedure that requires patient buy-in. Calmly and reassuringly talk the patient through all the steps and possible discomfort they may experience: transient gagging/cough and “laryngeal dyspnea” (ie. the subjective sensation of mild dyspnea when the glottis is topicalized).
- Perform precision laryngoscopy. Minimize the amount of unnecessary pressure on soft tissues and airway structures during laryngoscopy and intubation.
The Approach: Ketamine-Facilitated Intubation
As indicated by a recently published review article,8 there is no high-quality evidence to guide us on the indications or efficacy of KFI, which means we must fall back on expert opinion and theory. Proposed strengths/advantages of the KFI technique include:
- Dissociation provides amnesia and analgesia while maintaining airway tone and respiratory drive.
- Quicker than topicalization procedure.
- Can be used in uncooperative patients.
Theoretical downsides of KFI:
- It comes with all the often-quoted side effects of IV ketamine: hypersalivation, laryngospasm, N/V, passive regurgitation, hypertension, and possible worsening/precipitation of psychosis.
- Ketamine is often touted as hemodynamically neutral. However, is known to cause hypotension in patients who are critically ill and catecholamine deplete.
- One of the main concerns with KFI is the maintenance of airway reflexes, along with possible increased airway tone. Anecdotally, this can lead to significant difficulty when performing intubation:
- Patient may bite down on laryngoscope and ETT.
- Increased airway tone can make laryngoscopy more challenging.
- Patient may gag, cough, and adduct vocal cords during intubation which can render ETT advancement more challenging.
More information on KFI can be found HERE.
Take Home Point: KFI is likely more technically challenging, but it may provide an alternative if you would like to avoid RSI, but the patient is not amenable to an awake approach.
Take Home Points. Remember!
- Predicted difficulty, but you have some time? Use a “breathing intubation” technique.
- An awake technique is more straightforward than you think. Strongly consider it for a cooperative patient with predicted difficulty.
- Avoid oversedation! Go low and slow with anxiolysis and analgesia medications during awake intubation.
- Reassure and coach your patient during topicalization.
- Be prepared! Remember, an awake technique is just your “Plan A.”
- Consider KFI:
- In a predicted anatomic or physiologic difficult airway.
- If patients are not cooperative enough for an awake approach.
- If there is not enough time for an awake approach.
References
- Lundstrøm LH, Duez CHV, Nørskov AK, et al. Effects of avoidance or use of neuromuscular blocking agents on outcomes in tracheal intubation: a Cochrane systematic review. Br J Anaesth. 2018;120(6):1381-1393. doi:10.1016/j.bja.2017.11.106
- Cook T, Woodall N, Frerk C. 4th National Audit Project of The Royal College of Anaesthetists and The Difficult Airway Society (NAP4) Major Complications of Airway Management in the United Kingdom.; 2011. doi:10.1007/s12630-011-9576-5
- Brown CA 3rd, Sakles JC, Wick N. The Walls Manual of Emergency Airway Management. Fifth. Wolters Kluwer; 2018.
- Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management – Part 2 – Difficult airway. Can J Anesth. 2013;60(11):1119-1138. doi:10.1007/s12630-013-0020-x
- El-Boghdadly K, Onwochei DN, Cuddihy J, Ahmad I. A prospective cohort study of awake fibreoptic intubation practice at a tertiary centre. Anaesthesia. 2017;72(6):694-703. doi:10.1111/anae.13844
- Kovacs G, Law A. Airway Management in Emergencies.
- Alhomary M, Ramadan E, Curran E, Walsh SR. Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia. 2018;73(9):1151-1161. doi:10.1111/anae.14299
- Merelman AH, Perlmutter MC, Strayer RJ. Alternatives to Rapid Sequence Intubation: Contemporary Airway Management with Ketamine. West J Emerg Med. 2019;20(3):466-471. doi:10.5811/westjem.2019.4.42753




