Chest pain is one of the most common presentations to the emergency department (ED) and includes a wide differential diagnosis. In today’s post, we will review a less common cause of chest pain seen in the ED: pericarditis and myocarditis. We will also review considerations for these disease processes as it pertains to COVID-19.
Let’s start with a case: Joe is a 30-year-old male who presents with five days of pleuritic chest pain that is worse while supine. He is otherwise healthy, does not take any medications or use any recreational substances.
There is a very broad differential diagnosis for Joe’s presentation, but let’s take a deeper dive into pericarditis, which is on the differential for this patient.
PERICARDITIS
Pericarditis it the most common form of pericardial disease worldwide1. It is estimated that pericarditis is diagnosed in approximately 5% of patients presenting with non-ischemic chest pain to EDs in North America and Western Europe1. Previous studies have estimated that the incidence of pericarditis is between 16.1-27.7 cases per 100,000 population per year2,3.
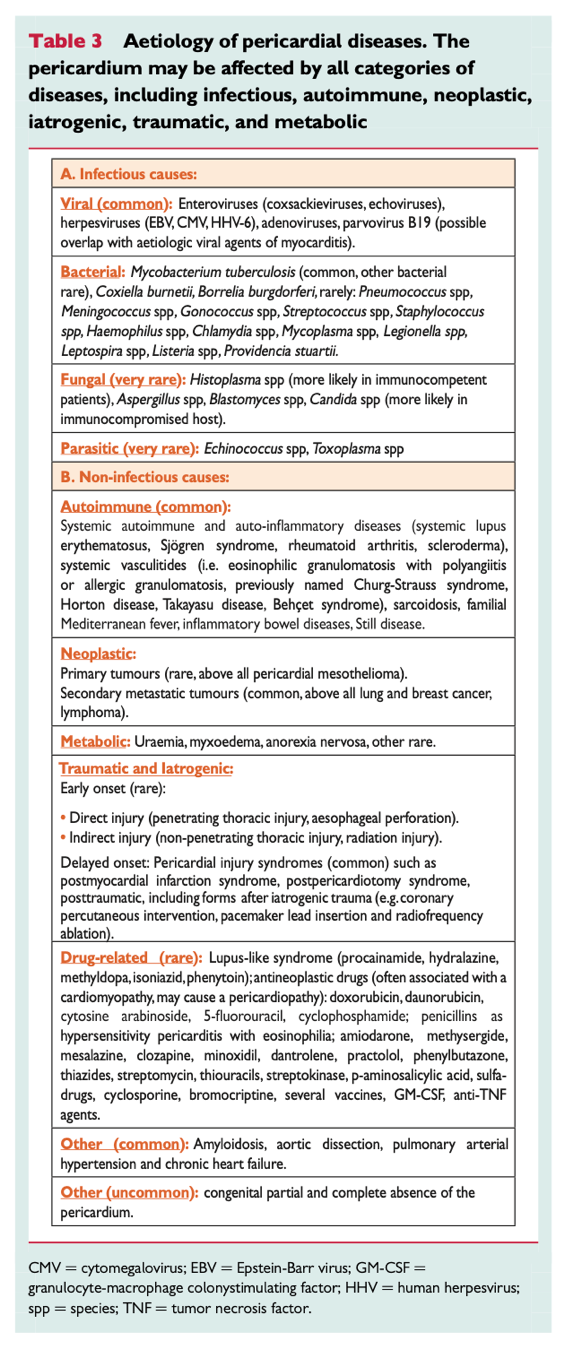
Etiology
- In Western Europe and North America, about 80-90% are deemed “idiopathic” and are presumed to be viral1.
- In countries with a high prevalence of tuberculosis (TB), this accounts for about 70% of pericarditis diagnoses. This carries a high degree of mortality: about 25% at 6 months in the absence of HIV and 40% in patients with HIV1. In developed countries, less than 5% of all cases are secondary to TB.
Diagnostic criteria
In order to make a diagnosis of pericarditis, two of out of the four diagnostic criteria below must be met. This is the definition from the most recent European Society of Cardiology (ESC) Guidelines from 2015.2
- Typical chest pain (85-90% of patients4)
- Sharp and pleuritic, improved by sitting up and leaning forward.
- Pericardial friction rub (18-85% of patients3,4)
- Superficial scratching or squeaking sound best heard with the diaphragm over the left sternal border.
- Pericardial effusion (31-60% of patients3,5)
- ECG changes (60-90% of patients4)
- Widespread ST elevation, PR depression with reciprocal changes in aVR (ST depression and PR elevation) are seen in the acute phase.
Investigations
- Laboratory
- CBC, electrolytes, urea, creatinine, troponin
- ESR/CRP
- Imaging
- Bedside point-of-care-ultrasound
- Chest xray
- ECG
What is the role of ESR/CRP?
- Elevation in ESR and CRP can be supportive of a diagnosis of pericarditis and measuring their levels is recommended by the ESC guidelines. These inflammatory markers are also helpful to monitor disease activity and efficacy of therapy during cardiology follow-up.2
- In a 2010 prospective study of 200 patients with viral or idiopathic pericarditis, 78% had an elevated CRP. Negative CRP at presentation was caused by early disease course in 34% of cases and previous anti-inflammatory therapies in 50%.6
- In another study by Prepoudis et al from 2021, they found that more than 25% of patients with a diagnosis of pericarditis had a normal CRP. This study only included patients presenting within 12h of pain onset, thus early presentation could have contributed to lower than expected CRP concentrations in this study.3
- Bottom line: Although ESR/CRP will often not change management in the ED, this information is very helpful when the patient is seen in follow up by cardiology and helps guide the efficacy of treatment. It may also be useful in helping with a diagnosis when diagnostic uncertainty exists.
Case progression:
Joe’s investigations show an elevated ESR and CRP and POCUS shows a small pericardial effusion. You diagnose him with pericarditis given that he meets 2/4 criteria. You are ready to write his discharge prescription and feel that he is appropriate for outpatient management.
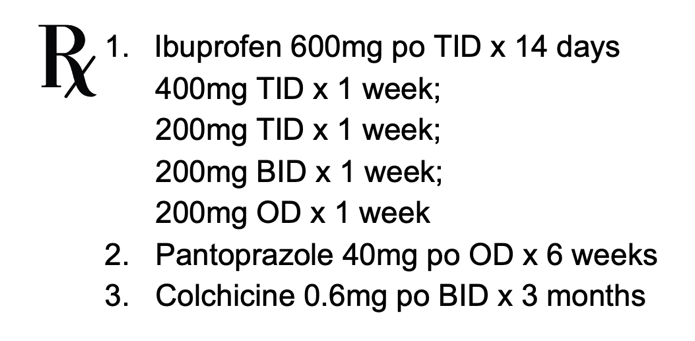
Treatment
- Aspirin or NSAIDs
- Ibuprofen 600-800mg TID
- ASA 650-1000mg TID
- Indomethacin 25-50mg TID
- Once symptoms have resolved, need to be tapered weekly for 2-4 weeks to reduce subsequent recurrence rate.
- For post-MI patients or patients who are already on ASA, recommend treatment with high-dose ASA rather than other NSAIDs.4
- Colchicine
- Weight-based dosing2:
- < 70kg → 0.6mg daily
- > 70kg → 0.6mg BID
- Duration: 3 months
- Used as an adjunct to NSAIDs to improve remission rates at one week and reduce recurrence rates in both acute and recurrent pericarditis.1
- The evidence for Colchicine comes from the COPE trial, a prospective, randomized, open label trial by by Imazio et al. examining 120 patients with first episode acute pericarditis. Patients in the ASA + colchicine group had a recurrence rate of 10.7% when compared to 32.3% in the ASA only group. This resulted in an NNT of 5.7
- Patients should also be counselled on the side effects of diarrhea which can be present in up to 23% of patients when taking colchicine.8
- Weight-based dosing2:
- Proton Pump Inhibitor
- Should be considered in all patients when treating with ASA/NSAIDs.
- Corticosteroids
- Not recommended as first-line therapy.
- Can be used in patients who cannot tolerate NSAIDs, have a contraindication, are pregnant or have renal failure.
- Recommend dosing of 0.2-0.5mg/kg/day followed by a slow taper.2
- Other therapies
- Oral azathioprine
- IV human immune globulins
- Anakinra
- Treatment with any of the above agents would be in consultation with cardiology as well as possibly rheumatology and would not be initiated by the emergency physician.
Disposition
- Patients with indicators of poor prognosis should have a cardiology consultation in the ED as they are at higher risk of treatment failure and complications.2
- Major RF:
- High fever >38C
- Subacute course (symptoms over several days without a clear acute onset)
- Evidence of large PCE (diastolic echo-free space >20mm)
- Cardiac tamponade
- Failure to respond within 7 days to NSAIDs
- Minor RF:
- Myopericarditis
- Immunosuppression
- Trauma
- Oral anticoagulants
- Patients without risk factors can be discharged home with appropriate treatment and outpatient cardiology consultation.
- Patients should be counselled on restriction of physical activity beyond ordinary sedentary lifestyle until resolution of symptoms or normalization of CRP for patients not involved in competitive sports.2,9
- Athletes should be counselled to return to sport only after symptoms have resolved and ESR/CRP/ECG/TTE are normal, with a minimum 3 month restriction.2,9
- Major RF:
Prognosis
- Most patients with acute pericarditis have a good long-term prognosis, especially those with presumed viral or idiopathic pericarditis.2
- In a prospective cohort study by Imazio and colleagues that looked at 453 patients 31 months after diagnosis of pericarditis, 18.3% had a recurrence, 3.1% had cardiac tamponade and 1.5% had constrictive pericarditis. Patients with a specific cause of pericarditis other than viral or idiopathic had a higher rate of complications, 38.2% vs 18.0%.10
Case Resolution
You get the prescription below ready for Joe, counsel him to restrict his physical activity and review reasons to return to the emergency department.
Take Home Points
- Normal ESR/CRP do not rule out pericarditis.
- Consult cardiology in ED when risk factors for poor prognosis present.
- On discharge:
- Prescribe NSAID taper, colchicine and PPI.
- Refer patients to cardiology.
- Counsel regarding activity limitation.
In addition to inflammation of the pericardium alone, the disease can further progress and involve the deeper tissues of the myocardium. Let’s have a look in more detail at this disease entity.
MYOCARDITIS
As per the world health organization (WHO), myocarditis is defined as an inflammatory disease of the myocardium diagnosed by established histological, immunological and immunohistochemical criteria.11,12 The incidence of the disease is difficult to define given changing definitions over the years, but it is estimated between 10-22 per 100,000 people.13,14 Myocarditis predominantly affects young patients with a median age of onset between 30-45 years and men are more affected than women.14
Etiology
- Etiology of myocarditis often remains undetermined and it can be caused by a variety of infections, systemic diseases and drugs.11
- See table below for a complete list of possible causes of myocarditis.
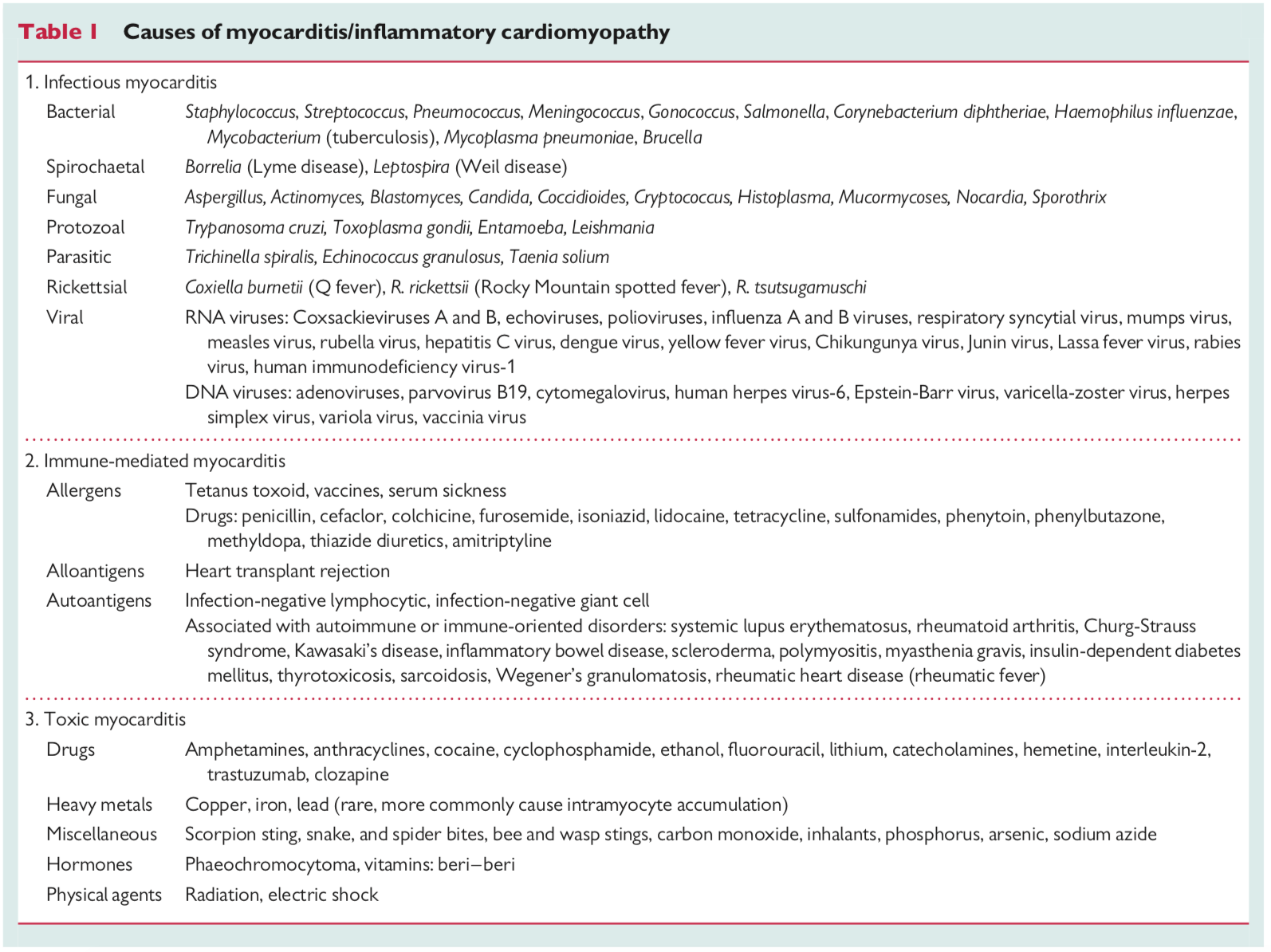
- Here is a list of suggested questions to consider asking on your clinical history pertinent to the causative agents of myocarditis:
- Any rashes? Specifically, any bulls-eye rashes? This question is important given the incidence of Lyme disease in the Ottawa Valley.15
- What medications do you take regularly? Are you on any chemotherapy treatment? Novel immune checkpoint inhibitors have been found to cause myocarditis (e.g. nivolimumab, pembrolizumab). 14
- Do you have a history of any autoimmune conditions such as lupus, dermatomyositis or inflammatory bowel disease?
- Have you had a recent mRNA vaccine?
Clinical Presentation
- Chest pain is the most frequent symptom, found in 85-95% of patients.14
- Dyspnea is the second most common symptom, in 19-49% of cases.14 If the myocarditis has also caused a cardiomyopathy, patients may present with symptoms consistent with heart failure such as orthopnea, paroxysmal nocturnal dyspnea and leg swelling.
- Patients may also present with ventricular arrhythmias leading to syncope.14,16
- Sudden cardiac death.
Investigations
- Laboratory
- CBC, electrolytes, creatinine,
- Troponin – would expect troponin to be elevated in setting of myocarditis
- ESR/CRP
- NT-proBNP
- Imaging
- Chest xray
- POCUS – looking for signs of LV dysfunction
- ECG
Diagnosis
- More common causes such as atherosclerotic and valvular heart disease should be excluded.
- Gold standard is histological or immunohistological evidence of an inflammatory cell infiltrate with or without myocyte damage that is obtained from an endomyocardial biopsy.16
- Cardiac MRI is becoming routine and is a sensitive and specific test for confirmation of acute myocarditis. It is also much less invasive than the above mentioned gold standard.16,17
Management
- Cardiology consultation in the ED for consideration of admission as well as further investigations.
Prognosis
- Prognosis and outcomes following diagnosis of myocarditis is highly variable and influenced by specific etiology.17
- In the review by Pollack et al., they report that patients who present with a preserved left ventricular (LV) ejection fraction typically recover in weeks to months. However, of patients presenting with significant LV dysfunction, 25% will have chronic systolic dysfunction, 50% will have complete resolution and the remaining 25% progress towards end-stage cardiomyopathy requiring transplant and/or death. Patients with giant cell myocarditis have a significantly worse prognosis with <20% of patients surviving at 5 years.17
- Ammirati and colleagues performed a retrospective multicenter registry from 19 Italian hospitals in 2018 and documented 443 patients with confirmed myocarditis. This was diagnosed either by endomyocardial biopsy or elevated troponin and characteristic changes seen on cardiac MRI.18
- In this cohort of patients, 26.6% had complicated acute myocarditis with LV systolic dysfunction, sustained ventricular arrhythmias or fulminant presentation (low cardiac output requiring inotropes/mechanical support). The remainder 73.4% had uncomplicated presentations.
- In hospital mortality and heart transplantation was 3.2% for the entire study population, however this was only seen in patients with a diagnosis of complicated acute myocarditis.
- There was 0% mortality at 5 years follow up in patients with uncomplicated acute myocarditis.
Take Home Points
- Keep myocarditis on the differential diagnosis for young patients presenting with chest pain and dyspnea. Have a low threshold to order a troponin in the workup of these patients.
- The prognosis following a diagnosis of myocarditis is highly dependent on the underlying etiology.
For the final section of this post, let’s have a look at have these diseases have changed in the setting of COVID-19.
MYOCARDIAL AND PERICARDIAL DISEASE IN THE SETTING OF COVID-19
The coronavirus disease 2019 (COVID-19) has affected millions of people since it was declared a pandemic on March 11 2020 by the WHO.19 In December 2020, Polack and colleagues published a multi-national, placebo-controlled, observer blinding efficacy trial that looked at a total of 43,448 patients who received two doses of the BNT162b2 COVID19 (Pfizer) vaccine 21 days apart.20 This study demonstrated 95% protection against COVID-19 in patients aged 16 years or older with minimal side effects.
As such, the Pfizer vaccine was granted emergency approval by the FDA on December 11 2020 and for the Moderna mRNA vaccine on Dec 18 2020.21,22 Similarly, Health Canada authorized the Pfizer vaccine for use on December 9 2020, followed by the Moderna vaccine on December 23 2020.23,24
As early as May 2021 there began to emerge a possible connection between COVID-19 mRNA vaccines and myocarditis. Here are three studies of many that identified a possible connection :
- Marshall and colleagues identified 7 cases of acute myocarditis or myopericarditis in adolescents who presented with chest pain all within 4 days of the Pfizer vaccine. All patients had elevated troponin measurements and cardiac MRI revealed late gadolinium enhancement characteristic of myocarditis. In this group of patients, 3 were treated with NSAIDs only and 4 received intravenous immune globulin as well as corticosteroids. None of the patients were critically ill and all were discharged from hospital.25
- Rosner and colleagues looked at 7 patients who were hospitalized for acute myocarditis-like illness after COVID-19 vaccination. All patients were males under the age of 40 and presented to the ED between 3 and 7 days following vaccination with acute onset chest pain and elevated troponin. Three patients underwent cardiac angiography and no coronary artery disease was identified. All patients had symptom resolution at the time of hospital discharge with a length of stay of 3 days (+/- 1day).26
- Larson and colleagues identified 8 males between the ages of 22 and 56 years old who presented following the first or second dose of the COVID-19 vaccine. All were found to have an abnormal troponin, transthoracic echocardiogram and cardiac MRI. Four patients were treated with NSAIDs or colchicine, 2 with corticosteroids and 3 did not require any treatment. All patients were discharged home with resolution of symptoms and preserved LV ejection fraction.27
In reaction to this, the FDA released a statement regarding the increased risks of myocarditis and pericarditis following vaccination on June 25 2021. 28 This was followed shortly by a similar warning by Health Canada on June 20 2021.29
This new finding is relevant for emergency physician and other primary care providers as patients will frequently present to the ED if they have post-vaccine reactions.
Barda and colleagues used data from the largest health care organization in Israel to evaluate the safety of the Pfizer vaccine.30
- They analyzed 173,106 patients with COVID-19 that were matched by sociodemographic variables to non-infected patients. There were 19 cases (0.01%) of myocarditis in the infected group compared 1 case (0.0005%) in the uninfected group with a risk ratio of 18.28.
- Furthermore, they analyzed 884,828 in each of the vaccinated and control cohort to look at possible adverse reactions following the vaccine. They reported 21 cases (0.0022%) of myocarditis in the vaccinated cohort, compared to 6 cases (0.0006%) in the unvaccinated group, corresponding to a risk ratio of 3.24.
- The limitations of this study include significant crossover of 26% into the vaccinated group over the course of the study, lack of randomization and possible missed or delayed diagnoses given out of network hospitals.
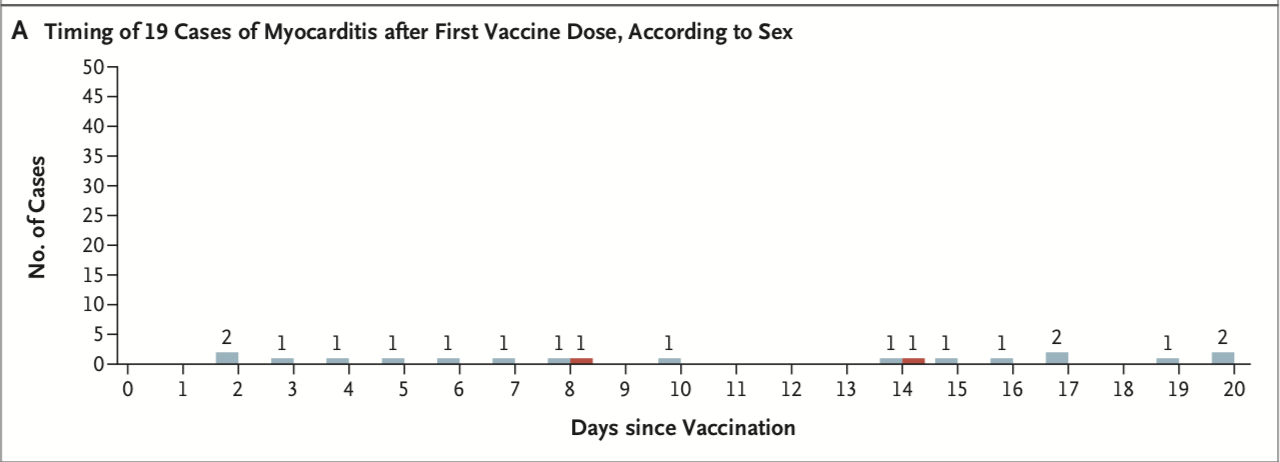
Mevorach and colleagues performed a retrospective review of data from December 2020 to May 2021 in Israel to investigate myocarditis following the Pfizer vaccine. Out of Israeli residents who were included during the surveillance period as per the Israeli Ministry of Health, 5,442,696 received a first dose and 5,125,635 received two doses.31
- There were 142 cases who developed myocarditis within 21 days after the first dose of the vaccine or within 30 days after the second dose. Of these 142 patients, 136 received a diagnosis of definite or probably myocarditis, 1 received a diagnosis of possible myocarditis and 4 has insufficient data.
- In the 136 cases of definite or probably myocarditis, the clinical presentation was mild in 129 (94.8%) of patients. One patient with fulminant myocarditis died. The LV ejection fraction was normal or mildly reduced in most patients and severely reduced in 4 patients.
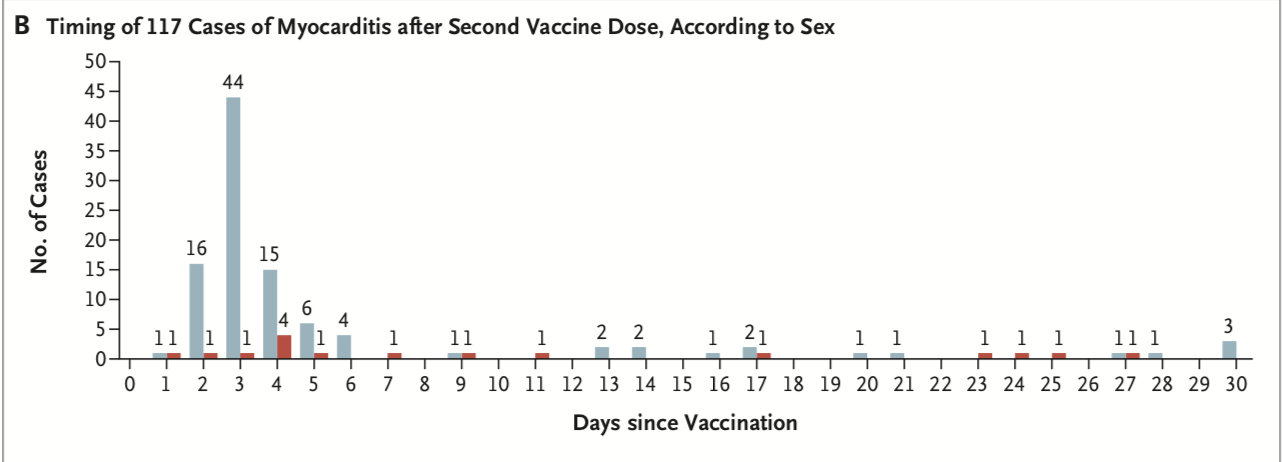
- Men and boy are predominantly affected with a spike in cases during the 7 days following the second vaccine dose.
- See graphs below that demonstrate the timing, age and gender distribution of post-vaccine myocarditis.
![]()
How many cases of post-vaccine myocarditis have we seen in Canada? In Ontario?
- Up to and including October 15 2021, there were 956 reports of myocarditis/pericarditis to Public Health Canada. Of those, 573 occurred following vaccination with Pfizer, and 357 following the Moderna vaccine.32
- In Ontario, as of October 10 2020, there were 438 reports of myocarditis/pericarditis following the COVID-19 mRNA vaccines. Within this group of patients, 242 (55.3%) required hospitalization for a median length of 2 days.32
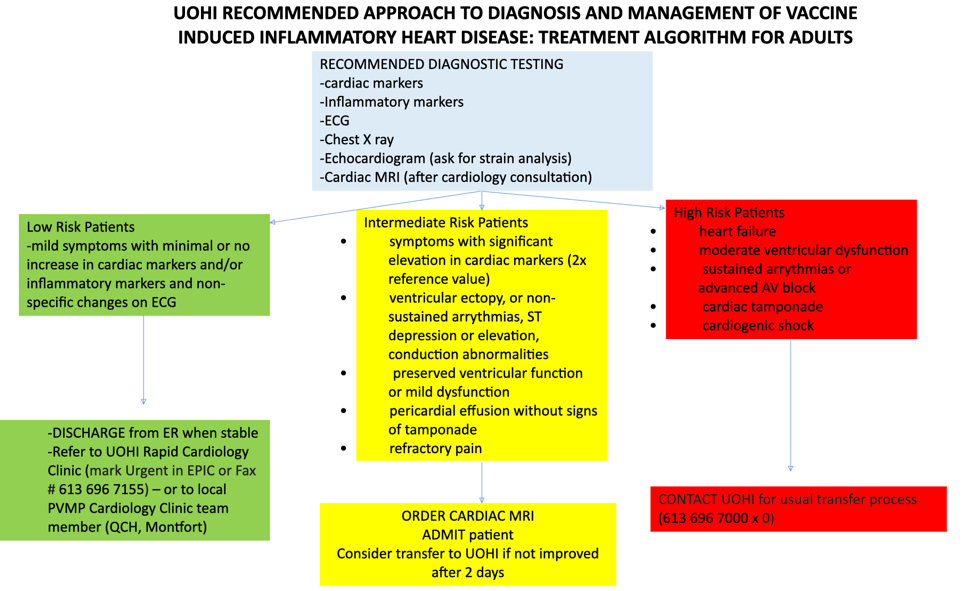
What is the management of patients who present to the ED with chest pain or dyspnea following a COVID-19 vaccine?
This is the local Ottawa Hospital/University of Ottawa Heart Institute algorithm for managing these patients when they present to the emergency department. It should be used for any patient presenting to the ED with symptoms such as chest pain, palpitations and shortness of breath within 42 days of a COVID-19 vaccine 33.
For all of these patients, ensure to fill out your local adverse events following immunization form. The form in Ottawa can be found here.
Take Home Points:
- Investigate for post-vaccine myocarditis in patients within 42 days of COVID-19 mRNA vaccination.
- Most patients have good prognosis following the disease.
- Fill out the Adverse Events form for these patients.
References
- Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA. 2015;314(14):1498. doi:10.1001/jama.2015.12763
- Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. European Heart Journal. 2015;36(42):2921-2964. doi:10.1093/eurheartj/ehv318
- Prepoudis A, Koechlin L, Nestelberger T, et al. Incidence, clinical presentation, management, and outcome of acute pericarditis and myopericarditis. European Heart Journal Acute Cardiovascular Care. 2022;11(2):137-147. doi:10.1093/ehjacc/zuab108
- McNamara N, Ibrahim A, Satti Z, Ibrahim M, Kiernan TJ. Acute pericarditis: a review of current diagnostic and management guidelines. Future Cardiology. 2019;15(2):119-126. doi:10.2217/fca-2017-0102
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis. Journal of the American College of Cardiology. 2004;43(6):1042-1046. doi:10.1016/j.jacc.2003.09.055
- Imazio M, Brucato A, Maestroni S, et al. Prevalence of C-Reactive Protein Elevation and Time Course of Normalization in Acute Pericarditis: Implications for the Diagnosis, Therapy, and Prognosis of Pericarditis. Circulation. 2011;123(10):1092-1097. doi:10.1161/CIRCULATIONAHA.110.986372
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine in Addition to Conventional Therapy for Acute Pericarditis: Results of the COlchicine for acute PEricarditis (COPE) Trial. Circulation. 2005;112(13):2012-2016. doi:10.1161/CIRCULATIONAHA.105.542738
- Terkeltaub RA, Furst DE, Bennett K, Kook KA, Crockett RS, Davis MW. High versus low dosing of oral colchicine for early acute gout flare: Twenty-four-hour outcome of the first multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-comparison colchicine study. Arthritis & Rheumatism. 2010;62(4):1060-1068. doi:10.1002/art.27327
- Seidenberg PH, Haynes J. Pericarditis: Diagnosis, Management, and Return to Play. Current Sports Medicine Reports. 2006;5(2):74-79. doi:10.1097/01.CSMR.0000306524.82124.47
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of Poor Prognosis of Acute Pericarditis. Circulation. 2007;115(21):2739-2744. doi:10.1161/CIRCULATIONAHA.106.662114
- Caforio ALP, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. European Heart Journal. 2013;34(33):2636-2648. doi:10.1093/eurheartj/eht210
- Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of Cardiomyopathies. Circulation. 1996;93(5):841-842. doi:10.1161/01.CIR.93.5.841
- Olejniczak M, Schwartz M, Webber E, Shaffer A, Perry TE. Viral Myocarditis—Incidence, Diagnosis and Management. Journal of Cardiothoracic and Vascular Anesthesia. 2020;34(6):1591-1601. doi:10.1053/j.jvca.2019.12.052
- Ammirati E, Frigerio M, Adler ED, et al. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy: An Expert Consensus Document. Circ: Heart Failure. 2020;13(11):e007405. doi:10.1161/CIRCHEARTFAILURE.120.007405
- Ontario Agency for Health Protection and Promotion (Public Health Ontario). Ontario Lyme disease map 2018: estimated risk areas. Published online 2018.
- Sagar S, Liu PP, Cooper LT. Myocarditis. The Lancet. 2012;379(9817):738-747. doi:10.1016/S0140-6736(11)60648-X
- Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis—diagnosis, treatment options, and current controversies. Nat Rev Cardiol. 2015;12(11):670-680. doi:10.1038/nrcardio.2015.108
- Ammirati E, Cipriani M, Moro C, et al. Clinical Presentation and Outcome in a Contemporary Cohort of Patients With Acute Myocarditis: Multicenter Lombardy Registry. Circulation. 2018;138(11):1088-1099. doi:10.1161/CIRCULATIONAHA.118.035319
- World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 — 11 March 2020.https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020.
- Polack FP, Thomas SJ, Kitchin N, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603-2615. doi:10.1056/NEJMoa2034577
- FDA Takes Key Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for First COVID-19 Vaccine.https://www.fda.gov/news-events/press-announcements/fda-takes-key-action-fight-against-covid-19-issuing-emergency-use-authorization-first-covid-19.
- FDA Takes Additional Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for Second COVID-19 Vaccine.https://www.fda.gov/news-events/press-announcements/fda-takes-additional-action-fight-against-covid-19-issuing-emergency-use-authorization-second-covid.
- Health Canada. Health Canada authorizes first COVID-19 vaccine.https://www.canada.ca/en/health-canada/news/2020/12/health-canada-authorizes-first-covid-19-vaccine.html.
- Health Canada. Health Canada authorizes Moderna COVID-19 vaccine.https://www.canada.ca/en/health-canada/news/2020/12/health-canada-authorizes-moderna-covid-19-vaccine.html.
- Marshall M, Ferguson ID, Lewis P, et al. Symptomatic Acute Myocarditis in 7 Adolescents After Pfizer-BioNTech COVID-19 Vaccination. Pediatrics. 2021;148(3):e2021052478. doi:10.1542/peds.2021-052478
- Rosner, C. M., Genovese, L., Tehrani, B. N., Atkins, M., Bakhshi, H., Chaudhri, S., … & Defilippi, C. R. Myocarditis Temporally Associated with COVID-19 Vaccination. Circulation. 2021;121(6):502-505.
- Larson KF, Ammirati E, Adler ED, et al. Myocarditis After BNT162b2 and mRNA-1273 Vaccination. Circulation. 2021;144(6):506-508. doi:10.1161/CIRCULATIONAHA.121.055913
- Coronavirus (COVID-19) Update: June 25, 2021.https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-june-25-2021.
- Health Canada. Health Canada updates Pfizer-BioNTech and Moderna COVID-19 vaccine labels to include information on myocarditis and pericarditis.https://recalls-rappels.canada.ca/en/alert-recall/health-canada-updates-pfizer-biontech-and-moderna-covid-19-vaccine-labels-include.
- Barda N, Dagan N, Ben-Shlomo Y, et al. Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. N Engl J Med. 2021;385(12):1078-1090. doi:10.1056/NEJMoa2110475
- Mevorach D, Anis E, Cedar N, et al. Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel. N Engl J Med. 2021;385(23):2140-2149. doi:10.1056/NEJMoa2109730
- Ontario Agency for Health Protection and Promotion (Public Health Ontario). Myocarditis and pericarditis following COVID-19 mRNA vaccines. Toronto, ON: Queen’s Printer for Ontario; 2021. :13.
- Lamacie, Mariana; Mielniczuk, Lisa; Beanlands, Rob; Liu, Peter; Crean, Andrew; Gauthier, Nadine; Gosh, Nina; Birnie, David; Small, Gary; Buchan, Arianne; Kafil, Tahir. UOHI/TOH Task Force on COVID-19 Vaccine-Induced Inflammatory Heart Disease. Published online 2021.



Nice post.
Minor correction. Under Pericarditis > Treatment > 2. Colchicine, weight based treatment…
It should read 0.6mg and not 6mg.
Thanks
Thanks! Change made.