Blast injuries resulting from explosions have the capacity to cause life-threatening multisystem injuries in multiple victims simultaneously. The biggest potential challenge in managing blast injuries is the creation of large numbers of simultaneous critically ill casualties. Once notified of a possible bombing or explosion, Emergency Physicians should immediately consider activating hospital disaster and contingency plans. The majority of injuries resulting from explosions are similar to those we encounter in our everyday trauma practice, though there are specific injuries to look out for and some injuries unique to blasts.
In this post. we will review the basic pathophysiology, sequelae, and management of blast injuries.
For other topics related to Military Medicine, please see our posts on Damage Control Resuscitation, TCCC and Recent Updates, Prolonged Field Care, Inhalation Injuries, Abdominal Stab Wounds, and Resuscitative Thoracotomy.
What causes Explosions?
- Accidental: e.g. industrial accidents (factory and mining operations, fuel transportation/storage)
- Non-accidental: deliberately set or detonated
- Manufactured: implies standard, military-issued, mass-produced weapons
- Improvised: small quantities, devices used outside of their intended purpose
- Unexploded ordnance: undetonated military explosive devices contaminating abandoned battlefields
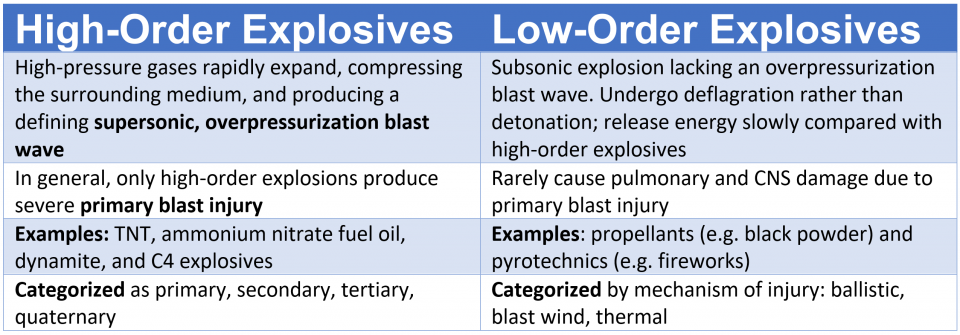
What is the difference between High-order and Low-order explosives?
What is the difference between a Blast Wave and Blast Wind?
- Blast wave
- Refers to the pressure differentials (over- and under-pressurization) created by an explosion
- Blast wind
- Refers to the flow of superheated air that can interact with people and objects and cause injury or damage
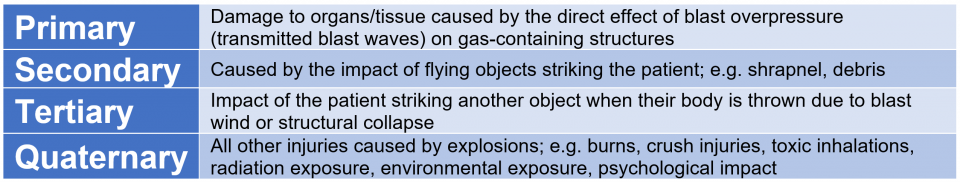
What are the Types/Categories of Blast Injuries?
Blast injuries (from high-order explosives) are generally categorized as primary to quaternary. A casualty may be injured by one or several mechanisms.
What factors affect the Severity of Blast Injuries?
The extent and pattern of injuries are the result of several factors:
- Amount and composition of the explosive material (e.g. shrapnel, CBRN)
- High-order vs low-order explosive
- Secondary blast injuries
- Debris that is displaced by the blast wind of the explosion and penetrates or interacts with the body surface
- Military explosives are designed to fragment to maximize damage (shrapnel)
- Terrorist bombers often place screws or other debris in/around bombs
- Responsible for the majority of casualties and mortality in many explosions
- Injuries can include fractures, amputations, lacerations, dislocations, and any type of soft tissue injury
- Debris that is displaced by the blast wind of the explosion and penetrates or interacts with the body surface
- Surrounding environment (e.g. enclosed space, protective barriers)
- Blasts in confined spaces (e.g. in a building, bus, mine) or underwater have the highest associated mortality
- Explosions leading to structural collapse and entrapment produce more orthopedic injuries and can cause crush injuries and compartment syndrome; longer extrication time increases mortality
- Solid surfaces reflect blast waves, therefore, a person standing next to a wall may suffer increased primary blast injury due to reflections, while someone standing behind solid cover may experience less injury
- Tertiary injuries are determined by what surface casualty strikes (e.g. hard flat surface, impaled on object, etc.)
- Distance between the victim and the blast
- Pressure wave intensity declines with the cubed root of distance from the explosion
- Delivery method (if a bomb is involved)
- Other environmental hazards (e.g. other propellants, flammable objects)
What are the most common injuries due to Primary Blast Injuries?
Pathophysiology: The leading edge of a blast wave is called the blast front. When the blast front strikes a casualty, it creates enormous, near-instantaneous rises in ambient pressure (e.g. C4 explosions can create initial pressures of over 30 GPa or 4 million psi). Air is easily compressible. Because of this, air-filled structures such as the lungs, bowel, and middle ear are most susceptible to primary blast injuries. Primary blast injuries can be subtle and have a delayed presentation.
The most common injuries occurring are:
- Blast ear (acoustic barotrauma)
- The ear is the organ most susceptible to primary blast injury
- Most commonly results in tympanic membrane (TM) rupture and middle ear damage, but can also lead to hemotympanum, cochlear damage, and ossicle fracture or dislocation
- Symptoms: decreased hearing or hearing loss, otalgia, tinnitus, vertigo, bleeding from the ear
- If there is bleeding from the ear, consider that the blast was intense enough to cause injury to the lungs and hollow organs
- At > 5 psi, the bony ossicles of the ear can be dislocated, fractured, and/or permanently destroyed
- TM rupture indicates a high-pressure wave (>40kPa or 6 psi; theoretically, the threshold for lung injury is 100 kPa or 15 psi) and may correlate with more severe organ injury, though this has recently been called into question
- Conversely, intact TMs do not necessarily imply the absence of serious injury, especially if the casualty was wearing hearing protection (e.g. military, police)
- All patients exposed to a blast should have an otologic assessment and audiometry
- Blast lung (pulmonary barotrauma)
- The most common fatal primary blast injury
- Includes pulmonary contusions, hemo/pneumothorax, systemic air embolism, ARDS, interstitial parenchyma damage, and/or subcutaneous emphysema
- Pulmonary contusion is the most common injury and it can be delayed in presentation up to 48 hours
- Acute gas embolism most commonly occludes CNS blood vessels, resulting in neurologic deficits that must be differentiated from traumatic causes
- Symptoms: dyspnea, cough, hemoptysis, and/or chest pain
- Blast brain (traumatic brain injury)
- Injury to brain parenchyma (mTBI or concussion), without direct injury to the head
- Symptoms: headache, fatigue, confusion, poor concentration, amnesia, decreased level of consciousness, depression, anxiety, and/or insomnia
- Blast eye (ocular barotrauma)
- Symptoms: eye pain/irritation, swelling, periorbital contusion or ecchymosis, lacerations or bleeding from the eye, decreased vision, blindness, hyphema, subconjunctival hemorrhage
- Up to 10% of all blast survivors have significant eye injuries
- These injuries involve perforations from high-velocity projectiles; can lead to globe rupture
- Can occur with minimal initial discomfort and result in delayed presentation
- Liberal referral for ophthalmologic screening
- Blast belly (intestinal barotrauma)
- More common with underwater than open-air injuries
- Includes abdominal hemorrhage and perforation (immediate and delayed), solid organ injury, testicular rupture, ischemia from air embolism
- The colon is the most common area of hemorrhage and perforation, though any portion of the GI tract can be injured
- Solid organs can also be contused or lacerated; however, hollow organ damage is much more frequent
- As with blast lung, intestinal perforation can present acutely or be delayed up to 48 hours
- Abdominal injuries may be occult, missed even with CT, and serial examinations are often required
- Symptoms: abdominal pain, nausea, vomiting, vomiting blood, rectal pain, testicular pain, unexplained hypovolemia, abdominal distention, and/or rigidity
- Thoracic primary blast injury
- The heart can also be damaged by the blast wave
- Symptoms/Signs: chest pain, tachycardia, decreased pulse pressure, cardiac dysrhythmias, pericardial tamponade (in the absence of penetrating trauma), and/or hypotension
- Primary blast injury produces the following unique cardiovascular response (which is sufficient to cause death in the absence of other demonstrable physical injury):
- Immediate CVS response (within seconds): decrease in HR, stroke volume, and cardiac index
- The normal reflex (increase in SVR) does not occur, so BP drops
- If this response is not fatal, recovery usually occurs within 15 minutes to 3 hours
What are the important assessment and management steps during Prehospital care?
- Ensure scene safety
- Be wary of the potential for dual explosions (in non-accidental explosions, a delayed explosion may be planned to injure rescuers)
- Screen for CBRN contamination; activate appropriate response and decontaminate if necessary
- Perform triage and/or trauma primary survey
- Attend to ABCs
- Rapidly control life-threatening external hemorrhage; early use of tourniquets
- Oxygen should be administered to all patients with respiratory distress, abnormal lung auscultation, or significant thoracic trauma
- Assess for major traumatic injuries as in any other trauma patient
- Initiate measures to prevent hypothermia
- Report: number of casualties, nature and size of explosion, timing, casualty proximity to blast epicenter, casualty displacement by blast wind, secondary fires, entrapment in collapsed structures, etc.
What Blood Work should be considered for Blast Injury patients?
- If the explosion occurred in an enclosed space or was accompanied by fire: test carboxyhemoglobin and electrolytes (acid/base status)
- Pulse oximetry readings may be misleading in cases of carbon monoxide poisoning
- Consider/treat for cyanide poisoning if the explosion occurred in an enclosed space and anion gap metabolic acidosis exists
- Major trauma: Hgb, crossmatch, screen for DIC
- Crush injury, compartment syndrome, or severe burns: consider rhabdomyolysis, hyperkalemia, renal failure
- Most patients injured by significant explosions should have a screening urinalysis
- Military white phosphorus (a widely used component of military munitions) is a severe pulmonary irritant and burns can cause hypocalcemia and hyperphosphatemia; serial levels are required
What Imaging studies are helpful in the work-up of Blast Injury patients?
Indications for CXR:
- Exposure to high overpressure
- TM rupture
- Respiratory symptoms
- Abnormal chest auscultation
- External signs of thoracic trauma
If significant abdominal pain is present, consider abdominal imaging (AXR or CT) to detect pneumoperitoneum from enteric rupture. Intestinal barotrauma is more common with underwater than air blast injuries.
As with the standard trauma assessment, FAST is a potentially useful tool. A positive FAST in an unstable patient is an indication for surgical exploration of the abdomen. Though, a negative FAST is unreliable in the setting of penetrating trauma and should be followed up with CT imaging. U/S can also reliably rule out pericardial effusion.
What are the important assessment and management steps during Emergency Department care?
Standard Trauma Management
- Primary and Secondary survey, with specific attention to the lungs, abdomen, and TMs
- Penetrating wounds (secondary blast injury), blunt trauma (tertiary/secondary blast injury), and burns are treated in the standard fashion
- Perform standard hemostatic resuscitation with blood products; correct coagulopathy; consider early fresh whole blood, if available
- In TBI, prevent hypoxia and hypotension
- A retrospective review during combat operations in Afghanistan and Iraq demonstrated that severe head injury was the most common cause of death in casualties who reached medical treatment facilities alive but subsequently died from injuries
- For pulmonary contusions, observation and repeat CXR may be necessary; definitive airway management and ventilatory support may be required
- For open wounds, consider broad-spectrum antibiotics and tetanus toxoid
Specific Considerations
- Treat shrapnel wounds (secondary blast injury) as low-velocity gunshot wounds
- For persistent abdominal pain or vomiting: consider admission for observation for intestinal hematoma (difficult to detect in the ED, even with CT imaging)
- White phosphorus (WP) burns require unique management
- Initial management: copious lavage, removing particles, and covering with saline-soaked gauze to prevent further combustion
- A Wood lamp may help identify WP particles
- Definitive treatment: rinse with 1% copper sulfate and remove the WP particles, then copious saline lavage.
- Never apply copper sulfate as a dressing; excess absorption can cause intravascular hemolysis and renal failure
- WP injury can lead to hypokalemia and hyperphosphatemia with ECG changes, cardiac arrhythmias, and death
- Cardiac monitor, serial electrolytes / extended lytes
- Closely track serum calcium; IV calcium may be required
- Initial management: copious lavage, removing particles, and covering with saline-soaked gauze to prevent further combustion
- Consider consultations as necessary to Trauma Surgery, ICU, ENT, Thoracic Surgery, Orthopedics, Plastic Surgery, Urology, Toxicology, etc.
- Consider transfer as necessary to a Burn Center, Level 1 Trauma Center, or a center with Hyperbaric Oxygen capabilities (for acute gas embolism)
What should be the Disposition of Blast Injury patients?
- Safe to Discharge Home after Observation:
- Open-space explosions, without apparent significant injury, normal VS, unremarkable lung and abdominal exam
- DC after 4 hours of observation
- Return to ED if: SOB, abdominal pain, vomiting, or any concerns
- Ensure close follow-up of wounds, head injuries, eye, ear, and stress-related complaints
- Prolonged Observation:
- Significant closed-space explosions, in-water explosions, or TM rupture = higher risk of delayed complications
- CXR, and selected imaging depending on Hx/Px
- Even if normal physical exam and imaging, these patients should have more intensive observation over a longer period
- Motivated, reliable, and asymptomatic patients may be sent home after 4 hours of observation
- Admission:
- Significant burns, suspected air embolism, radiation or WP contamination, abnormal VS, abnormal lung exam, evidence of pulmonary contusion or pneumothorax, abdominal pain, vomiting, hypoxia, or penetrating injuries to the thorax, abdomen, neck, or cranial cavity.
How do we manage patients thought to have arterial gas embolism (AGE) or cerebral AGE?
- Air embolism can present as stroke, MI, acute abdomen, blindness, deafness, spinal cord injury, or claudication
- Positive pressure ventilation (PPV) and positive end expiratory pressures (PEEP) should be avoided if possible in pulmonary blast injury due possible alveolar rupture and subsequent air emboli
- However, mechanical ventilation often cannot be avoided
- If possible, reduce tidal volume to limit peak inspiratory pressure (PIP) and minimize ventilator-induced barotrauma
- Consider permissive hypercapnia
- Treat with 100% oxygen
- Left lateral recumbent position to minimize risk of embolism out of the heart into the vascular system during PPV
- Hyperbaric Oxygen is the definitive treatment; transfer to a HBO-capable center may be required
- ASA may be helpful by reducing inflammation-mediated injury, though, consider the potential harm in the acute trauma patient
References
- Pennardt, A., Lavonas, E.J., Talavera, F., Levy, D.B., Mills, T.J., and Danzl, D. Blast Injuries. Medscape. 2016 Feb. https://emedicine.medscape.com/article/822587-overview.
- Jorolemon MR, Krywko DM. Blast Injuries. [Updated 2019 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430914/
- Explosions and Blast Injuries: A Primer for Clinicians. Center for Disease Control. Available from: https://www.cdc.gov/masstrauma/preparedness/primer.pdf Accessed 2019/08/11
- Plurad, D.S. Blast Injury. 2011. Military Medicine. 176, 3:276. Available from: https://academic.oup.com/milmed/article-abstract/176/3/276/4345300. Accessed on 2019/08/11
- Mathews ZR, Koyfman A. Blast Injuries. J Emerg Med. 2015 Oct. 49 (4):573-87.
- Champion HR, Holcomb JB, Young LA. Injuries from explosions: physics, biophysics, pathology, and required research focus. J Trauma. 2009 May. 66(5):1468-77; discussion 1477.
- Wolf SJ, Bebarta VS, Bonnett CJ, Pons PT, Cantrill SV. Blast injuries. Lancet. 2009 Aug 1. 374(9687):405-15.
- Moore JX, McGwin G Jr, Griffin RL. The epidemiology of firework-related injuries in the United States: 2000-2010. Injury. 2014 Nov. 45 (11):1704-9.
- Harrison CD, Bebarta VS, Grant GA. Tympanic membrane perforation after combat blast exposure in Iraq: a poor biomarker of primary blast injury. J Trauma. 2009 Jul. 67(1):210-1.
- Ashkenazi I, Olsha O, Turegano-Fuéntes F, Alfici R. Tympanic membrane perforation impact on severity of injury and resource use in victims of explosion. Eur J Trauma Emerg Surg. 2015 Dec 9.
- Keene DD, Penn-Barwell JG, Wood PR, Hunt N, Delaney R, Clasper J, et al. Died of wounds: a mortality review. J R Army Med Corps. 2015 Oct 14.
- Ozer O, Sari I, Davutoglu V, Yildirim C. Pericardial tamponade consequent to a dynamite explosion: blast overpressure injury without penetrating trauma. Tex Heart Inst J. 2009. 36(3):259-60.
- DeWitt DS, Prough DS. Blast-induced brain injury and posttraumatic hypotension and hypoxemia. J Neurotrauma. 2009 Jun. 26(6):877-87.
- Explosions and blast injuries: a primer for clinicians. Last reviewed May 26, 2005. CDC Emergency Preparedness & Response Web site. Available at http://www.bt.cdc.gov/masscasualties/explosions.asp.
- Nelson TJ, Wall DB, Stedje-Larsen ET, Clark RT, Chambers LW, Bohman HR. Predictors of mortality in close proximity blast injuries during Operation Iraqi Freedom. J Am Coll Surg. 2006 Mar. 202(3):418-22.
- Ritenour AE, Baskin TW. Primary blast injury: update on diagnosis and treatment. Crit Care Med. 2008 Jul. 36(7 Suppl):S311-7.
- Stuhmiller JH, Phillips YY, Richmond DR. The physics and mechanisms of primary blast injury. In: Bellamy AFR, Zajtchuk R, eds. Conventional Warfare: Ballistic, Blast, and Burn. 1991:247-70.
- Tuggle DW. Blast injury. J Okla State Med Assoc. 2003 Sep. 96(9):419-21.
- Wightman JM, Gladish SL. Explosions and blast injuries. Ann Emerg Med. 2001 Jun. 37(6):664-78.


