Even without an interest in military or high treat medicine, the science from military conflicts can have a significant influence on the medicine you practice. In fact, a lot can be learned in times of stress and conflict, and every Emergency Physician should have at least an awareness as to what our military colleagues are doing down-range. Although we don’t have firearms or ambushes aimed our way, and we may not be in direct danger in the strictest sense; just as they do, we have lives to save in a high stakes / high stress environment, and we need every advantage, every ounce of preparedness we can get to be effective. This blog post will provide a brief overview of the emerging area of military medicine known as Prolonged Field Care (PFC) and its numerous applications to rural/community medicine.
After reading this post, through an understanding of Prolonged Field Care, in the resource-constrained non-tertiary care environment, you will be able to:
- Integrate a holistic and evidence-based approach in the prolonged care setting
- Optimize communication using formats familiar and useful to all parties involved
- Avoid the common pitfalls of teleconsultation
For further information regarding Prolonged Field Care, please see prolongedfieldcare.org
For further information on Tactical Combat Casualty Care (TCCC) – see our blog posts on the basics of TCCC, recent updates, and deployedmedicine.com
For further information on Damage Control Resuscitation – please see our previous blog post
For other topics related to Military Medicine, please see our posts on Emergency Resuscitative Thoracotomy, Inhalation Injuries, Abdominal Stab Wounds, and Blast Injuries.
What are the differences between Civilian and Military trauma?
Before we dive into Prolonged Field Care, let’s briefly highlight the major differences seen in military and civilian trauma.
These differences are mainly secondary to:
- Protective equipment worn or not worn by casualties
- Patient population
- Mechanisms of injury
Civilian Medicine has:
- In terms of wounding patterns, because of a lack of protective ballistic armor/helmets
- More torso/abdomen/head trauma,
- More wounds per person, and
- Less exsanguinating extremity injury
- In terms of the patient population, civilian medicine includes special populations, chronic conditions, medications, etc. that otherwise healthy military aged personnel generally do not have
Military Medicine has:
- Higher incidences of penetrating trauma
- 75% by GSW and explosive fragmentation
- Higher energy and higher lethality of wounding agents
What is Prolonged Field Care?
- Before the term PFC was coined and a working group was formed, there had previously been no concerted effort to study and standardize the care of casualties in the operational environment for prolonged periods
- PFC occurs after TCCC when evacuation to higher levels of care is not immediately possible
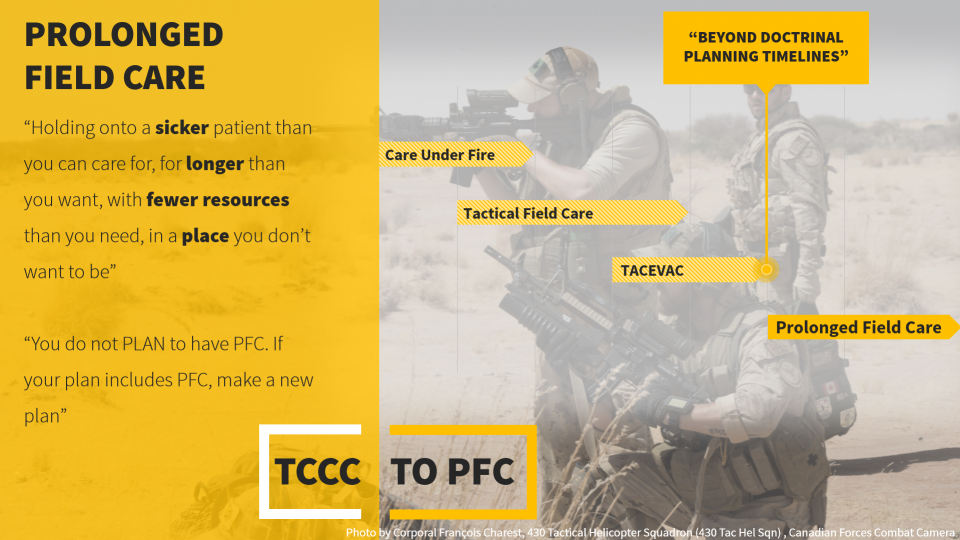
- Prolonged Field Care is “[h]olding onto a sicker patient than you can care for, for longer than you want, with fewer resources than you need, in a place you don’t want to be”
- This doesn’t just occur in the operational setting; it occurs in civilian settings as well
- The official definition for PFC is “[f]ield medical care, applied beyond ‘doctrinal planning time-lines’ … in order to decrease patient mortality and morbidity. [It] utilizes limited resources, and is sustained until the patient arrives at an appropriate level of care.”
- Practically, Prolonged Field Care is simply:
- Applying holistic evidence-based medicine in the “management of complex patients over extended periods of time in an austere, resource constrained environment”
- It’s like having a trauma team and admitting service packed into one/two people
- Its important to note that you do not PLAN to have Prolonged Field Care, if you are prepared that is better, but if you suspect you’ll end up providing PFC, then you make a new plan
- Its like Survival training or Mass Casualty training, nobody plans to be in it, but we need to prepare for it
Why is Prolonged Field Care Necessary?
In the Civilian sense, we need it…
- Because PFC can happen to ANYONE that practices medicine outside of a trauma center
- Its an all too common scenario that critically ill patients who are unfortunate enough to fall ill outside of large city centers cannot be transported in a timely manner to an appropriate medical facility
- Outside the bubble of tertiary care medicine and Level 1 Trauma centers, available personnel, resource utilization, available skill sets, and surgical / specialist capabilities are major considerations
- As specialists, such as ourselves, remain in or move to large centers, more responsibility falls to our community/rural colleagues
In terms of the Military…
- As operations transition from established and conventional environments with mature medical and evacuation resources, like in Iraq and Afghanistan, to operations with small Special Forces teams in more dispersed/austere environments appropriate medical services are unlikely to be available in a timely fashion, if at all
- Just as these military providers may be the ONLY medical providers available to any casualties in these environments, our rural EM colleagues are often the ONLY medical providers available in a timely fashion to their casualties
Look at the map…
- If we just do a quick size comparison, if we look at the land mass of Iraq and Afghanistan, and the personnel and infrastructure required for timely transport there… compared to the size of the continents that various military groups are now operating in… We see a huge discrepancy
- Similarly, if we compare the size of the Ottawa area, and the number of paramedic services we need to reach and deliver patients in a timely fashion… compared to the land mass of the U.S. and Canada… Then we begin to understand how thinly healthcare providers must be spread outside of metropolitan areas and why delays exist
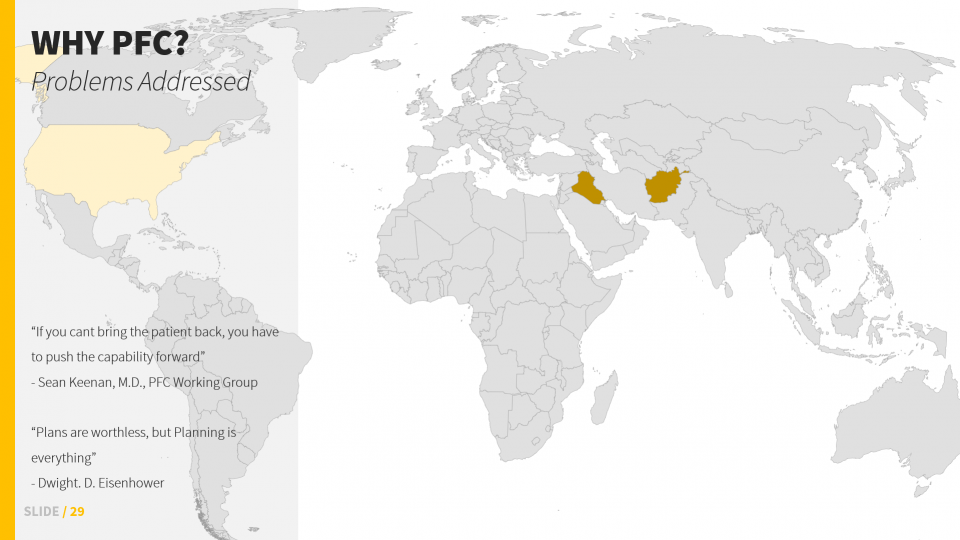
So then, what’s the solution?
- “If you cant bring the patient back [i.e. to a tertiary care center], you have to push the capability forward”
- PFC addresses this operational constraint – and can be translated to the rural civilian context
The solutions most readily available are:
- (1) training to increase austere critical care and evacuation capabilities and
- (2) providing access to expert consultation in real time
We will talk about each of these in turn as both these solutions “bring the expert to the patient”
How is Prolonged Field Care organized and conceptualized?
- Just like everything else in military medicine, there’s an acronym, and a staged approach
- Ruck, Truck, House, Plane – these aren’t linear; but conceptual and represent guidelines
- These stages are unique to each mission but are pretty self-explanatory:
- RUCK is gear carried by medical personnel
- TRUCK is any additional equipment carried in vehicles
- HOUSE is gear that can only be maintained at a team house or support site
- And PLANE is any gear available during evacuation
- These stages are unique to each mission but are pretty self-explanatory:
- This model, most importantly, allows planning and a shared understanding between boots on the ground and the command element as to what capabilities are available to care for patients at each level
- Similar considerations and principles are used in stocking EDs, ambulances, transport vehicles, expeditions, etc.
- A detailed understanding of capabilities is essential to proper planning across a system
- Having a common language to speak here sets the ground work for collaboration
- Similar considerations and principles are used in stocking EDs, ambulances, transport vehicles, expeditions, etc.
What are the MUST HAVE pieces of equipment for the austere medical provider?
Concept credit to Dr. Doug Powell, PFC WG
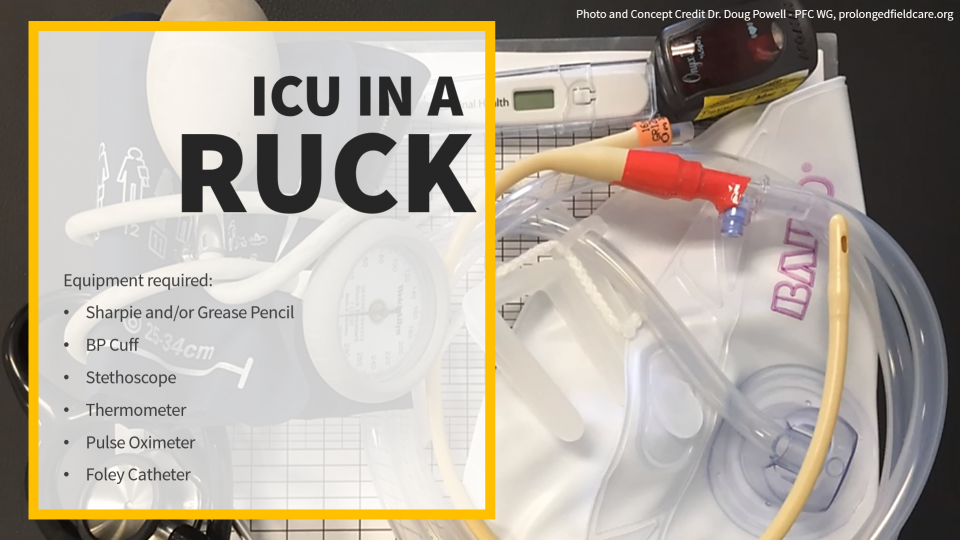
- We’re going to argue that you can provide (near) ICU level monitoring in a backpack
- But in terms of management, you’ll for sure exhaust your supplies quite quickly
- So, you’ll want to move to a phase where you can cache supplies as soon as possible (or you’ll consider proper stocking of your ED for this situation should it occur)
- But in terms of management, you’ll for sure exhaust your supplies quite quickly
- (Near) ICU level monitoring in a back pack? Its sounds crazy but bear with us, and think about this…
- What are the most important pieces of information we use to make decisions in the critical care setting, it’s not the fancy stuff… it’s the basics!
- Vital signs, mental status, pain, neurological function, and organ perfusion (urine output = one window)
- The most important aspects of critical care are diligent one-to-one monitoring – this is trending VS and early recognition of problems – and clinical expertise
- What are the most important pieces of information we use to make decisions in the critical care setting, it’s not the fancy stuff… it’s the basics!
- The GOAL is to use these low tech tools to prevent high tech interventions!
- Trend vital signs to detect problems and gradual/subtle changes so you can intervene early
What are the 10 Essential Capabilities of the Prolonged Field Care provider?
These are the capabilities you want to make sure you can accomplish during any austere medicine circumstance, whether that is planning for an expedition or stocking your rural ED. These capabilities are divided into minimum requirements, better, and best – recognizing that it is not always feasible to have all the equipment you could ever want.
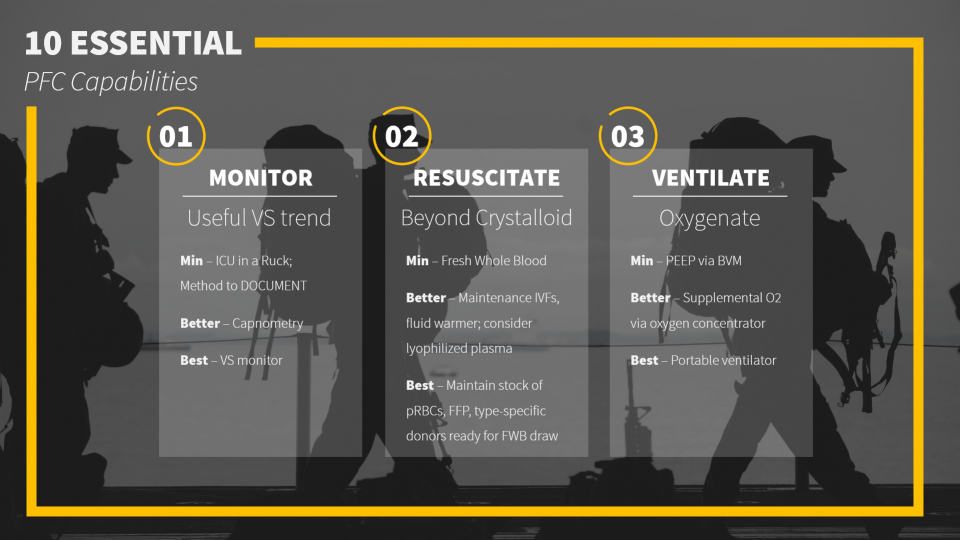
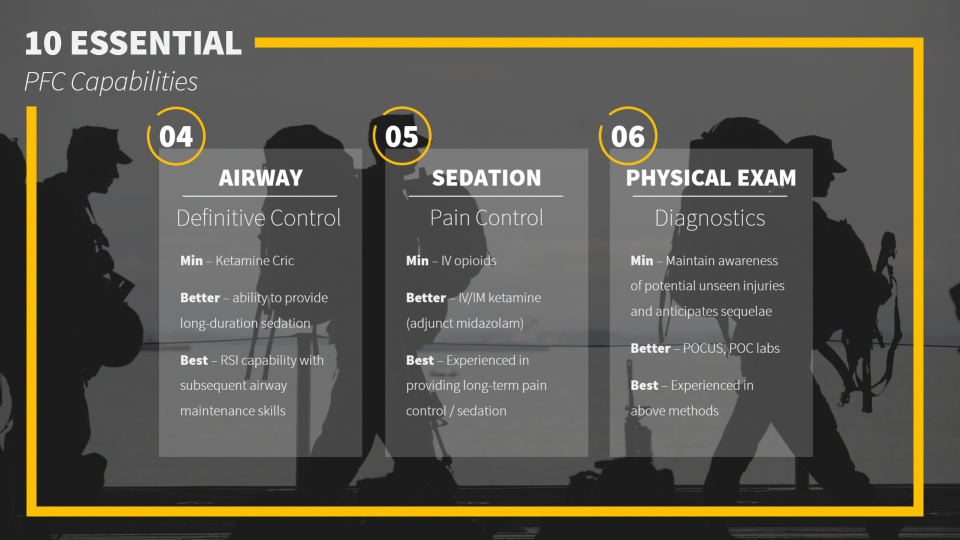
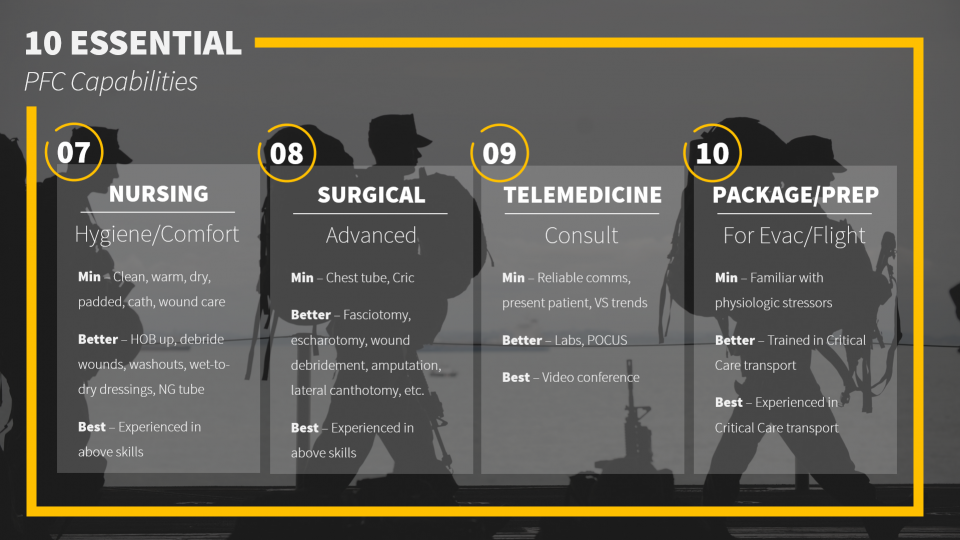
To summarize these essential capabilities, the RAVINES mnemonic is useful:
RAVINES
- Resuscitation, Reduce Tourniquets
- Airway, including Cric care
- Ventilate/Oxygenate – using lung protective strategy
- Initiate Telemedicine and Evacuation early
- Nursing care – including monitoring/trending VS, ins/outs, head of the bed (HOB) up, DVT prophylaxis, turning, passive range of motion, oral hygiene – these are all important in the prolonged field care setting
- Environmental considerations – hypo/hyperthermia, ear plugs, sun screen, chap stick, padding pressure points, motion sickness prophylaxis
- Surgical procedures
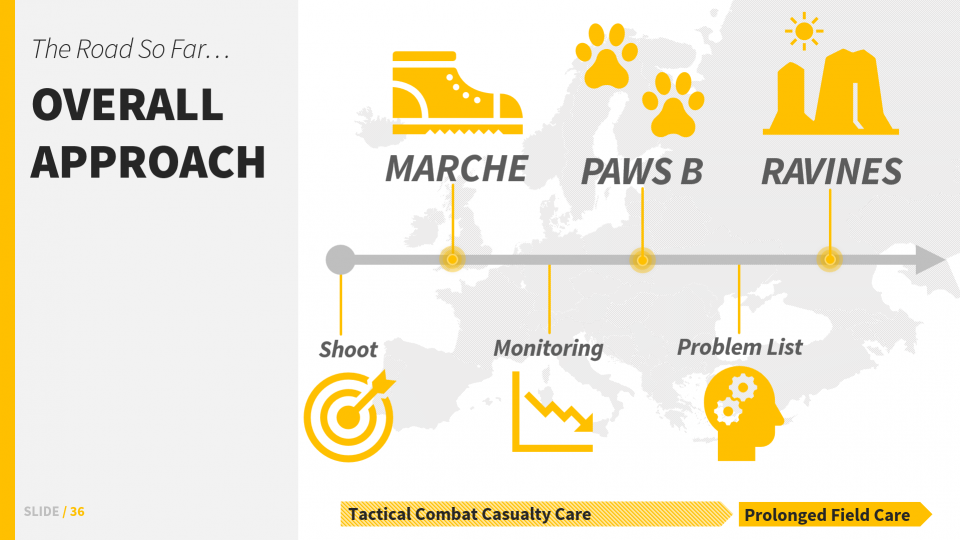
How do we combine TCCC and Prolonged Field Care?
To bring it all together, the general step-wise flow looks like this:
- S – MARCHE – PAWS B – RAVINES
- General flow
- Shoot back
- MARCHE (see our Intro to TCCC post)
- Begin VS monitoring/trending
- MARCHE + PAWS B
- Therapeutic pause, detailed secondary survey, problem list creation and prioritization
- PFC: RAVINES
- General flow
Documentation in Prolonged Field Care
The most important aspect of PFC is proper documentation for several reasons:
- It allows early recognition of developing issues (i.e. shock, sepsis, organ dysfunction, etc.)
- It promotes problem list creation and intervention prioritization
- And it allows the transfer of concise and complete information for handover
Two examples of military medical documentation are the TCCC Card and the PFC Flowsheet
TCCC Card = Minimum
- Designed to be used under stress
- Simple, succinct, easy/fast to complete
It includes:
- The ATMIST acronym: age/sex, timing, mechanism, injuries, signs/symptoms, treatments
- Time of all key interventions
- And an annotated diagram for physical exam and tourniquet times
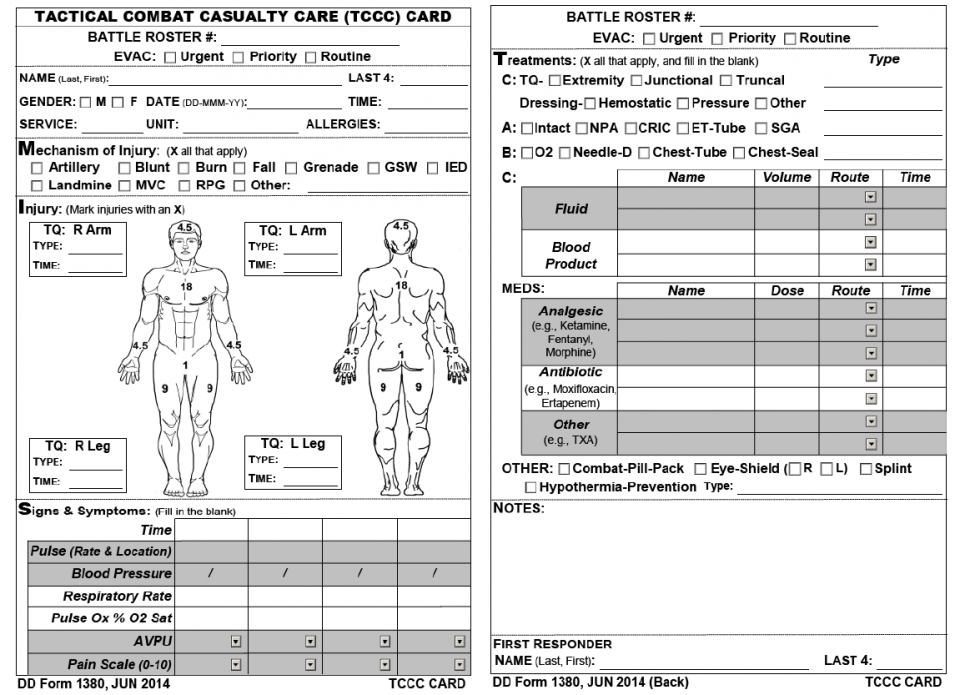
Joint Trauma System, Documentation in Prolonged Field Care CPG, 72. Nov 2018
The most important aspect here is that information is recorded and presented in a format that is familiar to all parties involved.
Prolonged Field Care Casualty Card = Better
When prehospital care transitions from TCCC to Prolonged Field Care, documentation should transition from the TCCC card to the PFC flowsheet. It consists of two pages.
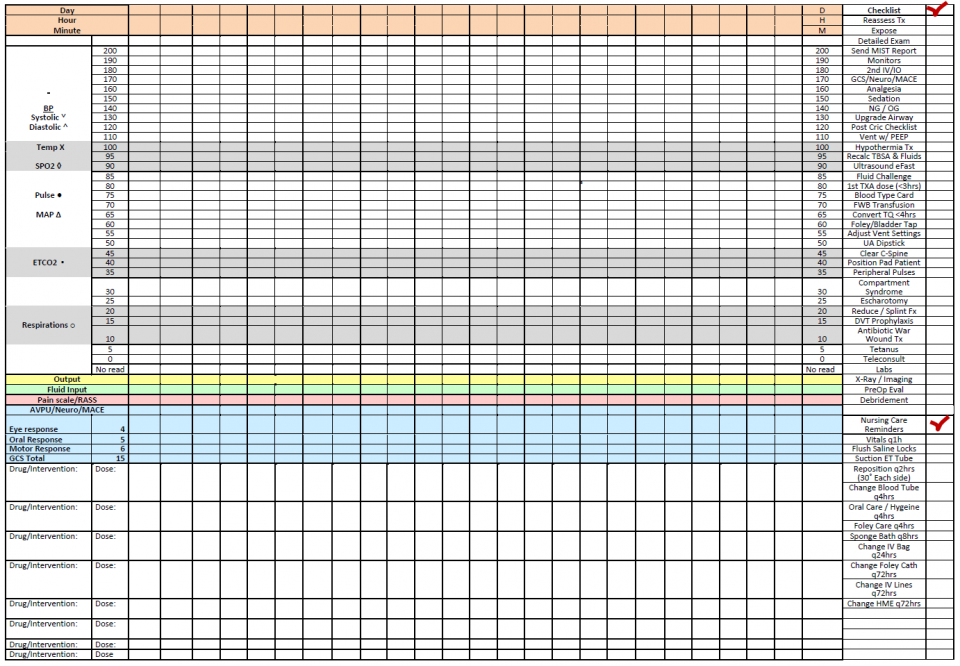
Joint Trauma System, Documentation in Prolonged Field Care CPG, 72. Nov 2018
Joint Trauma System, Documentation in Prolonged Field Care CPG, 72. Nov 2018
- The PFC Casualty Card is used to document trends over time and is useful for recognizing important clinical changes in complex casualties
- It not only serves to document care and identify trends but also contains a checklist of patient care and nursing interventions that may be needed
How can Military Telemedicine improve our Civilian consultation practices?
- The principle behind telemedicine and consultations:
- Enhances the skills of a provider who is physically caring for a patient, through input from an expert, without having to train the first provider to the level of the expert
- It brings the capability (the expertise) to the patient, expanding the catchment area of those who can receive specialist-level care and increases (temporarily) the scope of practice of the requesting provider
- It’s interesting to note that in the Military context, rehearsal of telemedicine consultation between providers and remote consultants has shown that communication is optimized when the caller completes a telemedicine script before calling and uses it during the consultation.
- So, should we meet and discuss with our consultants how they want information presented to them?
- Just as its the consultants’ responsibility to diligently consider the case and offer input/expertise, its our responsibility to logically present what consultants want to hear and need to know to take action by “speaking the language of the consultant” and asking a clear clinical question
This is how the military does it… another acronym…
- PREP
- Prepare:
- Develop a hierarchy of who to contact
- This may be self-evident in tertiary centers (junior, senior, fellow, staff), but in the community, what happens after you’ve called the one attending General Surgeon on call and they don’t pick up?
- After we’ve figured that out …
- We should rehearse presenting the consultation in a format that is familiar to both parties and caters to the needs of the receiving team (remember, we’re asking them for help)
- Develop a hierarchy of who to contact
- Recognize (when you should call):
- Call when you have a clinical question beyond your scope of practice
- Recognize your limitations, call before treatable conditions become more problematic
- Execute:
- Send available patient information (images, flow sheets, call scripts) by email or text ahead of the call
- Call using a script (or a standardized format familiar to both parties)
- Perform:
- Understand the capabilities and limitations of the technology available
- Perform training calls and after action reports (Quality Improvement)
- Prepare:
Optimizing communication during consultation
In terms of the actual information you want to receive or get across, you should focus on 3 areas:
- Live input – for the ongoing situation
- Anticipatory input – if this, then what; what complications/course is expected
- Capabilities – in addition to transmitting medical information, its important for the caller to provide information about their capabilities and care context
- Such as: level of the provider, available medications/equipment, monitoring, imaging, consultants in-house, surgical support, etc.
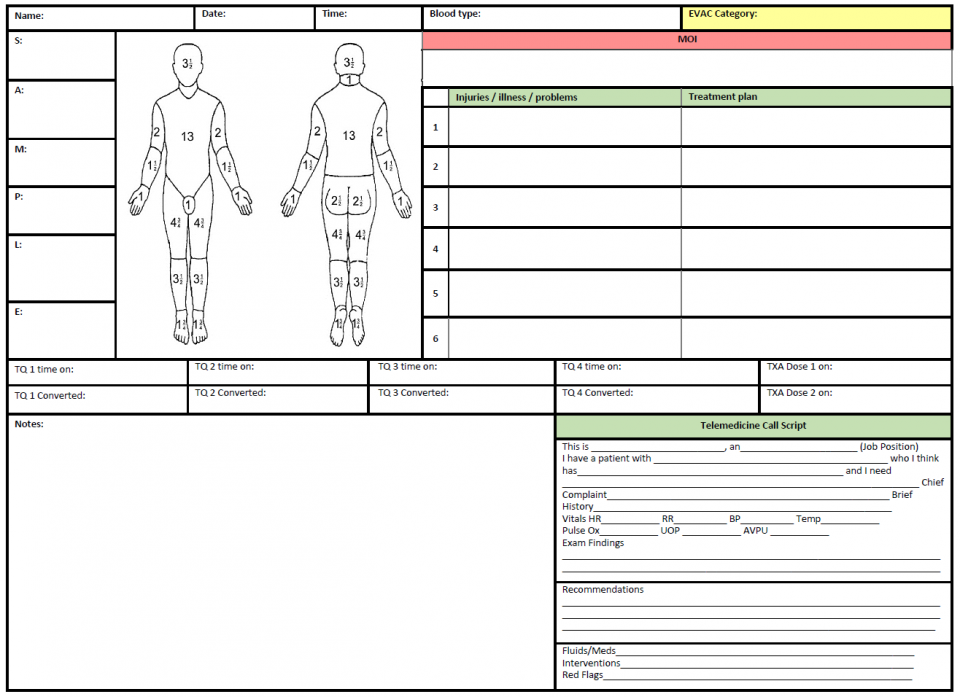
The Virtual Critical Care Consultation Service = Best
- The lessons we just covered were gleaned from the implementation and iterative improvement of the VC3 (virtual critical care consultation) service
- This service was extensively tested in field training exercises and validated in several real-world encounters
- It was developed in 2015 to provide medics with on-demand, virtual consultation with experienced critical care physicians 24 hours a day, from anywhere in the world
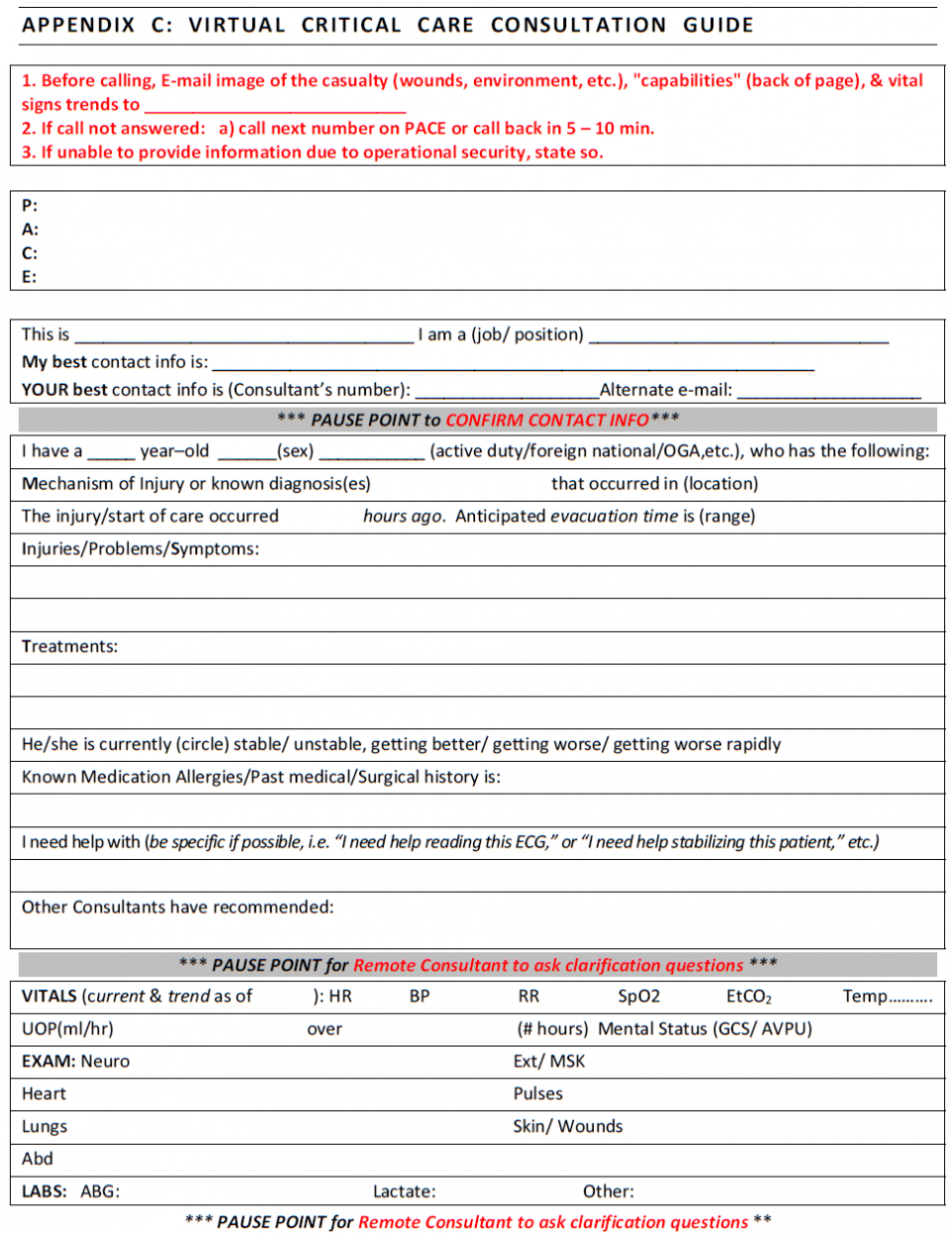
Joint Trauma System, Documentation in Prolonged Field Care CPG, 72. Nov 2018
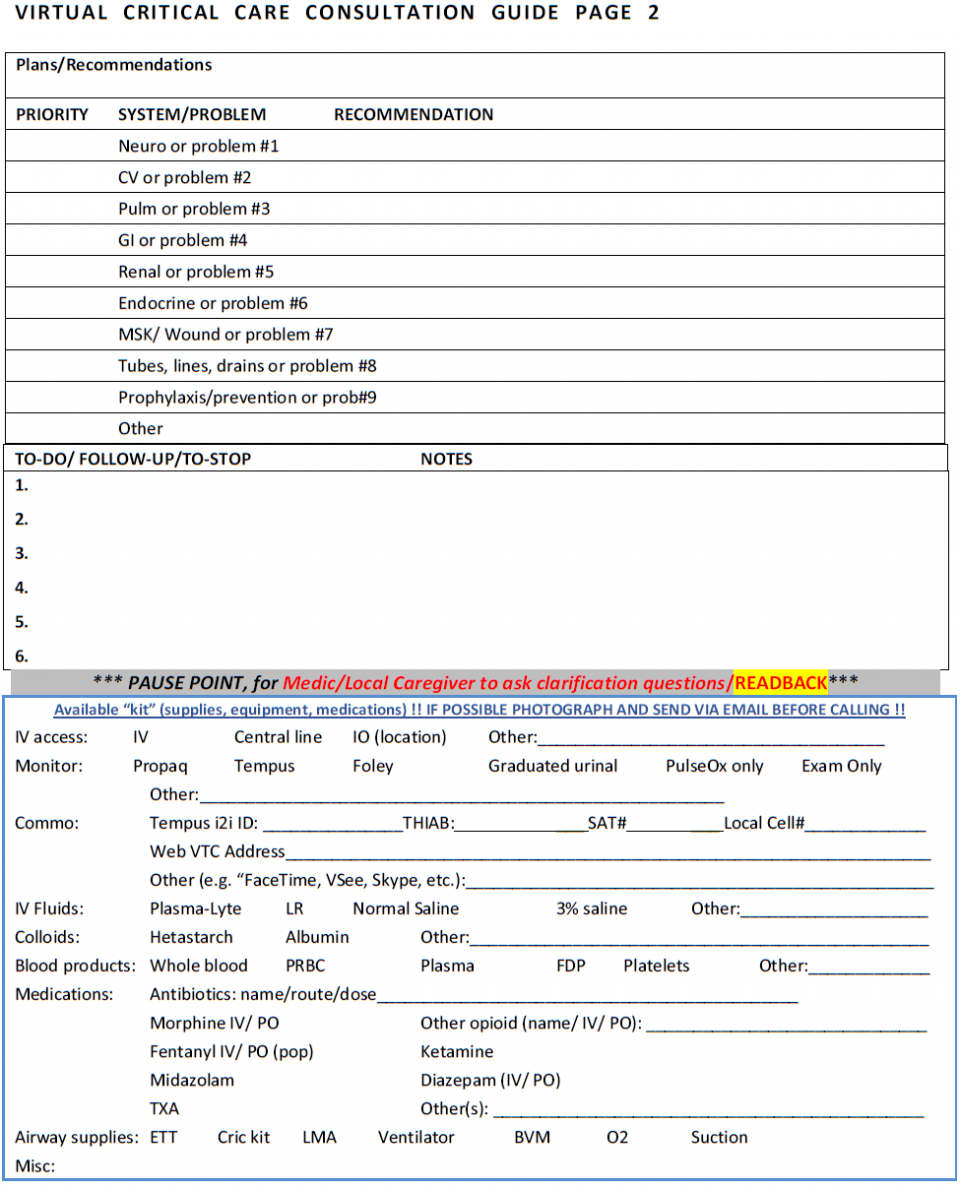
Joint Trauma System, Documentation in Prolonged Field Care CPG, 72. Nov 2018
- At the end of each section, there’s a “pause point” designed to give the consultant or medic an opportunity to review the information presented and to ask clarifying questions
- The section on capabilities is intended to be sent ahead of the voice consultation as a form of background information
- However, medics often send images of the entire script, which allows consultants to review the case before receiving the phone call and often reduces talk time and may facilitate more concise recommendations.
Take Home Points
All in all, we’ve covered the basics of Prolonged Field Care and its numerous applications to civilian medicine. We hope we’ve been able to show you the relevance and importance of understanding how our military colleagues practice. Now, through an understanding of Prolonged Field Care, in the resource-constrained non-tertiary care environment, you can:
- Integrate a wholistic and evidence-based approach in the prolonged care setting
- Optimize communication using formats familiar and useful to all parties involved
- Avoid the common pitfalls of teleconsultation
References
Agarwal HS, Saville BR, Slayton JM, et al. Standardized postoperative handover process improves outcomes in the intensive care unit: a model for operational sustainability and improved team performance. Crit Care Med. 2012;40: 2109–2115.
Benjamin Baker, DO; Doug Powell, MD; Jamie Riesberg, MD; Sean Keenan, MD. “Prolonged Field Care Working Group Fluid Therapy Recommendations.” Journal of Special Operations Medicine. 2016. Volume 16, Edition 1/Spring 2016.
Callaway DW; Smith ER; Cain J; Shapiro G; Burnett WT; McKay SD; and Mabry R. “Tactical Emergency Casualty Care (TECC): Guidelines for the provision of prehospital trauma care in high threat environments.” Journal of Special Operations Medicine Volume 11, Edition 3 / Summer/Fall 2011
Callaway, DW; Smith, ER; Shapiro, G; Cain, JS; McKay, SD; Mabry, RL. “The Committee for Tactical Emergency Casualty Care (C-TECC): Evolution and application of TCCC guidelines to civilian high threat medicine.” Journal of Special Operations Medicine Volume 11, Edition 2 / Spring 2011
Catchpole KR, de Leval MR,McEwan A, et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth. 2007;17:470–478.
Leopoldo C. Cancio, MD; Doug Powell, MD; Britton Adams, NREMT-P, ATP; Kenneth Bull, MD; Alexander Keller, MD; Jennifer Gurney, MD; Jeremy Pamplin, MD; Stacy Shackelford, MD; Sean Keenan, MD. “Management of Burn Wounds Under Prolonged Field Care.” Journal of Special Operations Medicine. 2016. Volume 16, Edition 4/Winter 2016.
Brendon Drew, DO; David Bird, PA-C, MPAS; Michael Matteucci, MD; Sean Keenan, MD. “Tourniquet Conversion: A Recommended Approach in the Prolonged Field Care Setting.” Journal of Special Operations Medicine. 2015. Volume 15, Edition 3/Fall 2015.
Grathwohl KW, Venticinque SG. Organizational characteristics of the austere intensive care unit: the evolution of military trauma and critical care medicine; applications for civilian medical care systems. Crit Care Med. 2008;36(7 suppl):S275–S283.
Lettieri CJ, Shah AA, Greenburg DL. An intensivist-directed intensive care unit improves clinical outcomes in a combat zone. Crit Care Med. 2009;37:1256–1260.
Lilly CM, McLaughlin JM, Zhao H, et al. A multicenter study of ICU telemedicine reengineering of adult critical care. Chest. 2014;145:500–507.
Lilly CM, Cody S, Zhao H, et al. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011;305:2175–2183.
Paul Loos, 18D; Erik Glassman, MS, NRP; Dan Doerr, 18D (Ret); Roger Dail, 18D; Jeremy Pamplin, MD Douglas Powell, MD; Jamie Riesberg, MD; Sean Keenan, MD; Stacy Shackelford, MD. “Joint Trauma System, Documentation in Prolonged Field Care CPG, 72.” Nov 2018.
Christopher J. Mohr, 18Z; Sean Keenan, MD. “Prolonged Field Care Working Group Position Paper: Operational Context for Prolonged Field Care.” Journal of Special Operations Medicine. 2015. Volume 15, Edition 3/Fall 2015
CPT Dawn Ostberg, RN, NC, USA; SFC Paul Loos, 18D, USA; COL (Ret) Elizabeth Mann-Salinas, RN, NC, USA; Cody Creson, 18D, USA; MAJ Douglas Powell, MD, USA; LTC Jamie Riesberg, MD, MC, USA; COL Sean Keenan, MD, MC, USA; Col Stacy Shackelford, MD, USAF,MC. “Joint Trauma System, Nursing Intervention in Prolonged Field Care CPG, 70.” Jul 2018.
LTC Jeremy Pamplin, MD; MAJ Andrew D. Fisher, PA-C; SFC Andrew Penny, 18D; SFC Robert Olufs, 18D; SFC Justin Rapp, 18D; Dr. Katarzyna Hampton, MD; LTC Jamie Riesberg, MD; MAJ Doug Powell, MD; COL Sean Keenan, MD; Col Stacy Shackelford, MD. “Joint Trauma System, Analgesia and Sedation Management During Prolonged Field Care CPG, 61.” May 2017.
Doug Powell, MD; Robert D. McLeroy, MD; Jamie Riesberg, MD; William Vasios, MPAS; Ethan Miles, MD; Jeffrey Dellavolpe, MD; Sean Keenan, MD; Jeremy Pamplin, MD. “Telemedicine to reduce medical risk in austere medical environments: the Virtual Critical Care Consultation (VC3) service.” Journal of Special Operations Medicine. 2016;16(4):102–109
Prolonged Field Care Working Group Position Paper: Prolonged Field Care Capabilities. June 2014. https://prolongedfieldcare.org/wp-content/uploads/2014/11/pfc-wg-position-paper-pfc-capabilities.pdf. Accessed May 2019.
SFC Justin Rapp, 18D, USA; MAJ Timothy Plackett, MC, USA; SGT Jonathon Crane, 68D, USA; SFC Jonathan Lu, 18D, USA; LTC David Hardin, MC, USA; SSG Paul Loos, 18D, USA; SFC (Ret) Richard Kelly, 18D, USA; Maj Andrew Hall, MC, USAF; COL Clinton Murray, MC, USA; COL Sean Keenan, MC, USA; Col Stacy Shackelford, USAF, MC. “Joint Trauma System, Acute Traumatic Wound Management in the Prolonged Field Care Setting CPG, 62.” Jul 2017.
William Vasios, APA-C; Jeremy C. Pamplin, MD; Doug Powell, MD; Paul Loos, 18D, ATP; Jamie Riesberg, MD; Sean Keenan, MD. “Teleconsultation in Prolonged Field Care Position Paper.” Journal of Special Operations Medicine. 2017. Volume 17, Edition 3/Fall 2017.
Thomas Walters, PhD; Douglas Powell, MD; Andrew Penny, NREMT-P; Ian Stewart, MD; Kevin Chung, MD; Sean Keenan, MD; Stacy Shackelford, MD. “Management of Crush Syndrome Under Prolonged Field Care.” Journal of Special Operations Medicine. 2016. Volume 15, Edition 3/Fall 2016
Weled BJ, Adzhigirey LA, Hodgman TM, et al. Critical care delivery: The Importance of Process of Care and ICU Structure to Improved Outcomes: An Update From the American College of Critical Care Medicine Task Force on Models of Critical Care. Crit Care Med. 2015;43:1520–1525.
David Van Wyck, DO; Paul Loos, 18D; Nathan Friedline, MD; Drew Stephens, MD; Brian Smedick, PA-C; Randall McCafferty, MD; Stephen Rush, MD; Sean Keenan, MD; Doug Powell, MD; Stacy Shackelford, MD. “Joint Trauma System, Traumatic Brain Injury Management in Prolonged Field Care CPG, 63.” Aug 2017.



Good afternoon Dr. Hoang,
Thanks for writing that, something I’ve been shouting from the roof tops since I found out about PFC. Agree 100%, but talk to the Wilderness Medical Society, or most anybody else, is very much the lone voice in the forest. The other difference between military and civilian trauma care, is that Beatle Baily to Gomer Pile on up, most everyone is trained in coTCCC and carries a BOK. We do see rifle wounds, (not as common as hand gun wounds), knife wounds, explosive injuries and MVA. The other thing I yang about, is the “0” responder concept. John or Jane Q. Public trained in AHA CPR (and suction/clearance to level of glottis) and a Stop the Bleed class, with the addition of a few tools, with the opportunity for near immediate intervention, unique in all of medicine to stop or reverse processes, an opportunity typically passed by the time the cavalry arrives. Consider the Central Nervous Apnea associated with concussion. Minor probably won’t notice, moderate to severe, maybe they breath on their own, maybe not. You don’t even need to understand the pathophysiology of what’s happening, you just need to look and see that the dudes not breathing, open the airway, maybe a few breaths…
All prehospital interventions, military/civilian/first responder/EMS/Doc, are predicated on keeping the patient (s) alive, tweaking them as much as possible, and delivering them to higher, the sooner the better, and it all falls apart, when for whatever reason, we need to hold onto them. Then we need to up our game, and we typically can’t because “PFC scenarios don’t occur outside the military”. And yet on a regular basis, it dose happen.
True story, 20ish y/o female, rock climbing, takes a ~30′ tumbling fall into a creak. ED Doc helping out with the SAR team. On arrival she is GCS 15 with good numbers. On exam, she has distal neuropathies, pelvis is tender on palpation, and she is hypothermic. Getting late in the afternoon, and their helo don’t do night stuff, so the need to hold onto her over night. She remains stable through out, and is evacuated in the AM, no harm, no foul. BUT, that MOI could have presented very differently. If she was unstable on arrival or became unstable while under their care, they still would have to hold her over night. ED protocols, depending on the patient and Doc, but typically get you 2 hours max, then 1of 3 things happens, patient walks out, dies or gets admitted, so we’re down to 10 hours. I contend prehospital damage control resuscitation, all kinds of tourniquets, pelvic wraps and O negative low antigen blood, damage control surgery for non compressible hemorrhage, and critical care level interventions, in the woods, or anywhere else.
Until coTCCC and PFC is common and in place, people will continue to die unnecessarily
And then there’s rescue medicine.